Diabetic retinopathy and macular oedema treatment

Diabetic retinopathy is damage to the light-sensitive retina in the back of the eye caused by type 1 or type 2 diabetes.
Chronic high blood sugar levels from the disease damage tiny blood vessels in the retina, causing them to leak fluid or blood into the retinal tissues. Damage to retinal blood vessels also causes bleeding into the posterior chamber of the eye that contains the normally clear vitreous gel.
Eventually, these changes can cause irreparable damage to the retina and leads to vision problems that cannot be corrected with glasses or contact lenses.
Diabetic retinopathy is associated with the proliferation of a protein called vascular endothelial growth factor (VEGF) in the retina.
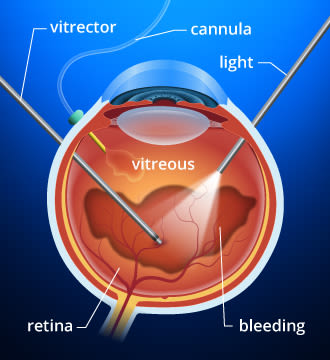
If you have a diabetic vitreous hemorrhage, you may require a vitrectomy to remove the clear, gel-like substance in your eye's interior.
VEGF stimulates the production of new blood vessels in the retina (neovascularisation) to bring more oxygen to the tissue when retinal blood circulation is inadequate due to diabetes.
Unfortunately, these tiny new blood vessels that form in the retina in response to VEGF are fragile and increase in number, leading to additional fluid leakage, bleeding and scarring in the retina leading to progressive vision loss.
Blood vessel leakage from diabetic retinopathy can cause fluid to accumulate in the macula, which is the most sensitive part of the retina that is responsible for our sharpest vision and colour vision.
This condition — called diabetic macular oedema (DME) — is the primary cause of vision loss associated with diabetic retinopathy.
Lasers for diabetic retinopathy treatment
Laser treatment of diabetic eye disease generally targets the damaged eye tissue. Some lasers treat leaking blood vessels directly by "spot welding" and sealing the area of leakage (photocoagulation). Other lasers eliminate abnormal blood vessels that form due to neovascularisation.
Lasers also may be used to destroy non-essential tissue in the periphery of the retina, which may help reduce the production of VEGF and improve blood flow to the central retina.
After laser treatment of the peripheral retina, some blood flow bypasses this region and instead provides extra nourishment to the central portion of the retina. The resulting boost of nutrients and oxygen helps maintain the health of cells in the macula that are essential for detailed vision and colour perception. However, some peripheral vision could be lost due to this treatment.
The two types of laser treatments commonly used to treat significant diabetic eye disease are:
Focal or grid laser photocoagulation
This type of laser energy is aimed directly at the affected area or applied in a contained, grid-like pattern to destroy damaged eye tissue and clear away scars that contribute to blind spots and vision loss. This method of laser treatment generally targets specific, individual blood vessels.
Panretinal laser photocoagulation (PRP)
With this method, about 1,200 to 2,400 tiny spots of laser energy are applied to the periphery of the retina, leaving the central area untouched.
Treatment of clinically significant DME also entails using fluorescein angiography to provide images of the eye's interior. These images accurately guide application of laser energy, which helps "dry up" the localised swelling in the macula. A fluorescein angiogram also can identify the location of blood vessel leakage caused by proliferative diabetic retinopathy.
While laser treatment for diabetic retinopathy usually does not improve vision, the therapy is designed to prevent further vision loss. Even people with 20/20 vision (6/6) who meet treatment guidelines should be considered for laser therapy to prevent eventual vision loss related to diabetes.
What to expect before, during and after laser treatment
Laser treatment typically takes place in a clinic or eye hospital and no overnight stay in a hospital is required.
Make sure you have someone drive you to and from the hospital or clinic on the day you have the procedure. Also, you'll need to wear sunglasses afterward because your eyes will be temporarily dilated and light sensitive.
Before the procedure, you will receive a topical anesthetic or possibly an injection adjacent to the eye to numb it and prevent it from moving during the laser treatment.
Your ophthalmologist will make the following adjustments to the laser beam before it is aimed into the eye:
The amount of energy used
The size of the "spot" or end of the beam that is directed into the eye
The pattern applied by the laser beam onto the targeted area
A laser treatment typically lasts at least several minutes, but more time may be required depending on the extent of your eye condition.
During laser treatment, you might experience some discomfort, but you should feel no pain. Right after a treatment, you should be able to resume normal activities. You might have some discomfort and blurry vision for a day or two after each laser treatment.
The number of treatments you need will depend on your eye condition and extent of damage. People with clinically significant diabetic macular oedema may require three to four different laser sessions at two- to four-month intervals to stop the macular swelling.
If you have proliferative diabetic retinopathy (PDR) — meaning that leakage of fluid has begun in the retina — the laser treatment should take from 30 to 45 minutes per session, and you may require up to three or four sessions.
Your chance of preserving your remaining vision when you have PDR improves if you receive panretinal laser photocoagulation as soon as possible following diagnosis.
Non-laser treatment of diabetic macular oedema
Injection of corticosteroids or other medications into the eye — either directly or in the form of an injectable implant — sometimes is recommended over laser procedures for the treatment of diabetic macular oedema.
Or in some cases, a combination of drug injections and laser treatment may be recommended.
Recent studies have shown that drugs called anti-VEGF that are injected into the eye can be as effective as some laser therapies.
As diabetic retinopathy worsens, in addition to VEGF, other small "signal" proteins (cytokines) are released by cells, causing additional inflammation in the retina that can cause or worsen DME.
Corticosteroids have been shown to have a beneficial effect by decreasing the amount of VEGF and other inflammatory cytokines produced by cells (a process called "downregulation"), which can lead to a reduction of diabetes-related macular oedema.
Risks associated with intraocular steroid treatment for DME include steroid-induced cataracts and glaucoma. Vision loss from cataracts usually can be restored with cataract surgery. To reduce the risk of glaucoma, your ophthalmologist might recommend preventive use of glaucoma eye drops or even glaucoma surgery.
Vitrectomy and other surgical treatments for diabetic eye disease
In some people who have proliferative diabetic retinopathy, bleeding into the vitreous (vitreous hemorrhage) makes laser photocoagulation treatment impossible because the blood obscures the surgeon's view of the retina.
If the vitreous hemorrhage fails to clear within a few weeks or months, a surgical procedure called a vitrectomy may be performed to remove the bloody vitreous and replace it with a clear gel-like material. After the vitrectomy, laser photocoagulation can be applied. The laser procedure is performed either at the time of the vitrectomy or shortly thereafter.
Retinal bleeding and vitreous hemorrhage also can cause bands of scar tissue to form. These bands of scar tissue can cause traction on the retina that may lead to a retinal detachment. If you have been diagnosed with diabetic retinopathy and experience flashes of light and a sudden loss of peripheral vision (both are symptoms of a detached retina), see your optometrist or ophthalmologist immediately.
Page published on Monday, 16 March 2020






