Dry eyes: Symptoms and causes

Why are my eyes so dry?
Dry eye syndrome, also called dry eye disease (DED), is a condition in which the eyes do not make enough tears. DED can also occur when your eyes don’t create the correct type of tears. The condition is extremely common, affecting over 16 million Americans.
The chances of having DED increase with each decade of life, but it can affect people of any age. DED becomes even more common after age 50. People often experience DED in both eyes. It's possible to have dry eye symptoms in one eye only, but this is uncommon.
DED can be temporary or chronic. Examples of temporary dry eyes include dryness that you may experience when on vacation in a dry climate or when you’ve had too much screen time. Temporary dry eye is usually treated easily, and results are seen quickly. However, temporary symptoms that occur regularly and go untreated can lead to chronic DED.
Chronic dry eye syndrome is an inflammatory disorder that affects the tears and surface of the eye. It affects 5% to 30% of Americans aged 50 and older. The exact cause of chronic dry eyes is unknown, but experts have determined two different types: aqueous tear-deficient and evaporative.
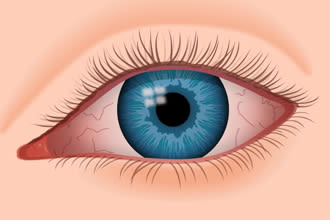
Dry eyes can become red and irritated, causing a feeling of scratchiness.
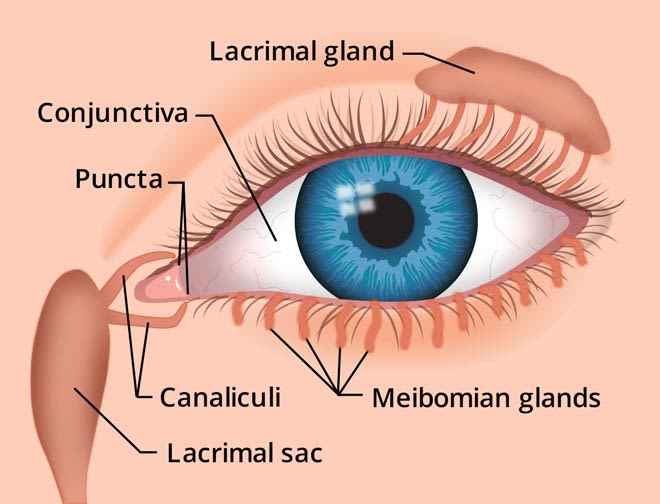
Aqueous tear-deficient DED occurs when the lacrimal gland cannot produce enough water-based tears to keep the eye’s surface hydrated and healthy.
Evaporative DED happens due to inflammation of the meibomian glands in the eyelids. These glands produce an oily substance over the watery tears that keeps them from evaporating too quickly.
DED and chronic dry eye syndrome can affect vision, but they very rarely cause permanent vision loss. While treatment for temporary dry eye disease and chronic dry eye syndrome are the same, chronic dry eyes often require long-term treatment. It’s also important to note that temporary dry eye can develop into chronic dry eye if left untreated.
The way the brain processes the pain signals caused by dry eye can vary widely between different people. Some people have minimal clinical signs of dry eye but still suffer tremendously from dry eye pain. In these patients, the brain amplifies the dry eye nerve impulses, and this is called neuropathic DED.
Other patients have lots of evidence that their eyes are dry when they are examined, but their eyes do not feel dry at all. These patients are said to have neurotrophic DED.
In most cases, DED is caused by a mix of aqueous tear-deficient and evaporative DED. Most cases of DED also do not fall in the extreme neurotrophic or neuropathic categories but somewhere in between.
SEE RELATED: Blocked tear ducts: Causes, symptoms and treatment
Causes of dry eyes
Dry eyes can occur because of several causes. Factors ranging from natural bodily processes to bad habits can be the cause of your dry, itchy eyes.
Below are a few causes behind eye dryness. It’s important to note that one or more causes can be contributing to your symptoms.
Natural causes
There are some contributing factors to chronic dry eyes that are out of your control. These factors include aging, being female and experiencing hormone changes.
Although DED can occur at any age, it becomes more common after age 50. As you get older, the eyes naturally produce fewer tears. This often leads to dry, gritty eyes.
Another natural process that affects eye hydration is changes in certain hormones, like estrogen and progesterone. These changes frequently affect women’s vision.
The biggest hormone changes occur during puberty, pregnancy, breastfeeding and menopause. The changes in hormone levels can cause dry eyes. Other hormone changes, like menstruation and being on birth control, can also affect tear production.
Environmental causes
Eye dryness can occur due to environmental factors, such as dry climate or high winds. This can be the case both indoors and outdoors.
Regarding indoor environments, air conditioning, ceiling fans and forced air heating systems can decrease indoor humidity. An example of this is in the cabins of airplanes. This extremely dry air can lead to dry eye problems, especially among frequent flyers.
When considering outdoor environments, dry climates, high altitudes and dry or windy conditions can increase dry eye risks. Outdoor conditions can also trigger allergies, which can cause dry eyes. Additionally, taking antihistamines to relieve allergies can also cause dry eyes.
Health related causes
Underlying health conditions can affect the eyes’ ability to produce tears. Certain diseases, such as diabetes, thyroid-associated conditions, lupus, rheumatoid arthritis and Sjogren's syndrome, can contribute to dry eye problems.
A condition that directly causes DED is called lagophthalmos. It’s characterized by incomplete closure of the eyelids when blinking or sleeping. Lagophthalmos has many causes, including natural aging, eye infections and nerve damage from trauma or cosmetic blepharoplasty.
Not only can certain conditions cause DED, but the medications you take for a condition may cause it as well. Many prescription and nonprescription medicines increase the risk of dry eye symptoms. Some of these include antihistamines, antidepressants, blood pressure medications such as beta-blockers or diuretics, and birth control pills.
Eye dryness is common after eye surgeries like LASIK and other corneal refractive procedures. In most cases, dry eye discomfort after eye surgery is temporary and resolves within a few weeks of the procedure.
Wearing masks, such as those worn with CPAP machines or to protect against the spread of infectious disease like COVID-19, can also dry the eyes. Ill-fitting or improperly worn masks can force the air out the top of the mask and over the surface of the eyes. Wearing glasses with a mask can direct the air over the eyes even more.
Habit-related causes
There are some cases of DED that can be traced back to certain habits. For example, frequent and prolonged computer use can dry the eyes out. This is because we tend to blink our eyes less fully and less frequently when using a computer, smartphone or other portable digital device. This leads to greater tear evaporation and increased risk of dry eye symptoms.
Another habit that is heavily linked to DED is wearing contact lenses. It can be difficult to determine if wearing contact lenses causes dry eyes. However, people who wear contact lenses more frequently have dry eye symptoms.
Smoking is a bad habit for many reasons, including its effect on the eyes. In addition to dry eyes, smoking has been linked to serious eye problems, including macular degeneration, cataracts and uveitis.
Dry eyes at night
It’s possible for dry, itchy eyes to feel worse at certain points, like at nighttime. If you find that your eyes feel the driest before you go to sleep, one or more of these reasons could be why:
Contact lenses – Wearing contact lenses all day, especially if paired with computer use, can cause the eyes to be particularly dry at nighttime.
Environmental factors – Being exposed to wind, pollution, screen time and other elements throughout the day can take a toll on the eyes. So, by the end of the day, they can be dried out and fatigued.
Screen time – Checking emails and social media before bed not only affects your sleep quality but can cause your eyes to feel dry.
Some ways to help nighttime dry eye are to protect your eyes when wearing contact lenses. You can do this by applying over-the-counter eye drops to keep the eyes fresh and by only wearing contact lenses for the recommended duration set by your eye doctor.
Avoiding screen time before bed and using a humidifier in your room to add moisture to the air can also help with nighttime eye dryness.
Dry eyes in the morning
Waking up with gritty eyes usually means that something during the night is causing your eyes to dry out. Some reasons behind dry eyes in the morning include:
Nocturnal lagophthalmos – Being unable to fully close your eyes while sleeping can result in seriously dry eyes when you wake. This can be caused by floppy eyelid syndrome— a condition where the eyelids become soft and will open during sleep.
Certain medication – Taking medication before bed is often recommended for various prescriptions. If eye dryness is a side effect of the medication, taking it before bed may cause the eyes to be dry and irritated in the morning.
Sleeping conditions – Sleeping with a fan blowing on your face, having a ceiling fan going, or sleeping directly below an air vent can cause the eyes to be dry in the morning.
Solutions to dry eyes in the morning can include wearing a sleep mask to protect the eyes from air being produced by fans or air vents. You may also find relief by applying eye drops or ointments to the eyes right before bedtime.
SEE RELATED: Dry eye masks
Dry eye symptoms
Dry eye disease can show itself in many ways. It’s also common for symptoms to vary between individuals who experience them. The symptoms you feel may worsen during or after certain activities, like spending time outside on a windy day or wearing contact lenses.
Symptoms of dry eyes and dry eye syndrome include:
Tired, heavy eyes
Gritty, scratchy feeling
Photophobia (light sensitivity)
Blurred vision
Feeling like something is in your eye (foreign body sensation)
Mucus in or around the eyes
Discomfort when wearing contact lenses
And, as odd as it may sound, watery eyes can also be a symptom of DED.
This is because dryness on the eye's surface can sometimes lead to overproduction of the watery part of your tears as a protective mechanism. But this "reflex tearing" does not stay on the eye long enough to correct the underlying dry eye condition.
In addition to these symptoms, dry eyes can cause inflammation and (sometimes permanent) damage to the surface of the eye.
Diagnosing dry eye syndrome
The only way to know for sure if you've got chronic dry eyes is to have your eye doctor perform one or more dry eye tests during an eye exam. Some dry eye tests they may run include:
The Schirmer’s test
The Schirmer's test consists of placing a slip of paper under each eye and keeping them there for five minutes. The paper absorbs tears released from the eyes, which is used to measure the volume of tears produced.
Tear breakup time test
This test measures how quickly tears evaporate from the eye’s surface.
Fluorescein dye drops are placed in the eyes, and the patient is asked not to blink. The amount of time between the last blink and the first appearance of a dry spot in tear film is the “tear breakup time.” Tear breakup time under 10 seconds may indicate chronic dry eyes.
Tear osmolarity test
During this test, a device is hovered along the eyelid margin, where it collects tears. The device measures how much salt is in the tear film compared to its water content. This will generate a concentration number between 290 and 400 mOsm/L. Normal osmolarity concentration falls between 275-307 mOsm/L.
MMP-9 inflammation test
MMP-9 is an inflammatory molecule that is present on the surface of eyes with chronic DED. To check for these molecules, a small amount of tears is absorbed onto a strip of paper. In the case of DED a red line will appear — similar to a pregnancy or COVID test.
Fluorescein dye test
This test uses orange dye and a blue light to check for foreign bodies in the eye. It also checks the corneal tissues for injury.
Lissamine green staining is another dye test that increases visibility of degenerated cells in the conjunctiva. This particular dye is commonly used to diagnose or rule out DED.
Careful examination of your eyes by an eye doctor can reveal the presence and severity of chronic dry eye syndrome. Your doctor can then determine the best type of dry eye treatment to keep your eyes healthy, comfortable and seeing well.
SEE RELATED: Epiphora: Excessive eye watering
Treatment and medication for dry eyes
There’s no shortage of options when it comes to chronic dry eye treatment. From your run-of-the-mill eye drops to medical procedures, there’s something for everyone. Talk to your doctor about your specific dry eye symptoms. They can help you determine which treatment is best for your case.
Eye drops and nasal sprays
Mild cases of dry eyes resulting from situational causes may be treated with frequent use of artificial tears or other lubricating eye drops. In fact, artificial tears are usually the first step in dry eye treatment.

Artificial tears usually are the first step in dry eye treatment.
There are many brands of artificial tears that are available over the counter (OTC) without a prescription. They come in a wide variety of ingredients and viscosity (thickness).
If your eye doctor determines that prescription relief is needed for your symptoms, they may recommend one or more medicated eye drops.
Prescription eye drops
Restasis, CEQUA and Xiidra are three FDA-approved prescription eye drops given for DED.
Restasis is an eye drop form of the immunosuppressant cyclosporine. It works by reducing inflammation in the eyes and, in turn, increasing tear production naturally. A generic alternative to Restasis, known as cyclosporine ophthalmic eye drops, can be purchased with a prescription.
CEQUA is another cyclosporine eye drop like Restasis. While the two are similar, CEQUA uses a technology that allows higher concentrations of medicine to be delivered into the eye with minimal irritation. Another key difference between them is in their formulation. CEQUA is a water-based solution that has the medication absorbed in tiny droplets called nanomicelles, while Restasis is an oil-based solution. There is currently no generic version of CEQUA eye drops.
Xiidra is another non-steroidal eye drop that works by targeting the inflammatory cells that cause dry eye.
Users are often happy with the results provided by any of these prescription eye drops. While it’s possible for patients to start seeing results in as little as two weeks, it can take months to notice improvements.
Nasal spray for dry eye
Tyrvaya (teer-VI-uh) is a prescription nasal spray that can relieve symptoms of DED. It works through your nasal passage to naturally activate the production of tear film.
Rather than relying on artificial tears, Tyrvaya helps users create natural tears of their own. Common side effects include nose and throat irritation, sneezing and coughing.
For the best results, spray Tyrvaya once into each nostril twice per day.
Be sure to follow your eye doctor’s directions concerning which eye drops to use and how often you use them. Using a different brand or multiple brands of artificial tears will make it difficult to assess the success of the dry eye treatment your doctor recommended.
SEE RELATED: Best contacts for dry eyes
Punctal plugs and temporary punctal occlusion
Punctal plugs sometimes are used in dry eye treatment to help tears remain on the eye’s surface longer. A punctal plug is a small, sterile device that is inserted into the small opening (puncta) of the tear duct. These ducts are in the inner corner of the upper and lower eyelids.
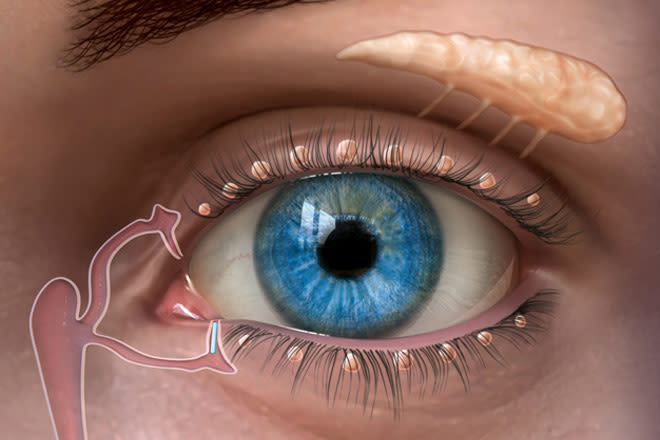
A punctal plug inserted in the tear duct of the lower eyelid to keep the eye’s tear film from draining away too quickly. Image: Oasis Medical, Inc.
After one or both of these openings have been plugged, tears drain away from the eye at a slower rate. This helps the tear film stay on the eye’s surface longer, relieving DED symptoms.
So where do the tears go? If one of the puncta is left open, the tears will still drain, just at a slower rate. Tears also leave the surface of the eye through evaporation from the eye’s surface. But if punctal plugs cause watery eyes, one or more of the plugs can be removed.
Meibomian gland expression
A large percentage of DED cases are caused by poor oil (meibum) secretion from meibomian glands. These glands are located along the margin of the eyelids, and their openings are near the base of the eyelashes.
The oil secreted from meibomian glands helps keep the tear film from evaporating too quickly from the eye’s surface. If the openings to the glands get clogged, the oil cannot be released and do its job.
This is called meibomian gland dysfunction (MGD) — a significant cause of evaporative dry eye symptoms. To treat meibomian gland dysfunction and evaporative dry eye, your eye doctor may perform an in-office procedure called meibomian gland expression.
The tear drainage system keeps the eye moist and protected.
Before this procedure, warm compresses may be applied to your eyelids. Then, a forceps-type device is used to squeeze the clogged contents from the meibomian glands. Contents may include hardened meibum and other substances.
There may be some discomfort during the procedure, as significant pressure must be applied to the eyelids. However, the results usually make any short-term discomfort from the procedure worth it.
Eyelid massage devices
In-office treatments like LipiFlow and iLUX are performed with devices that apply localized heat and pulsating pressure to express the meibomian glands. While the two treatments vary slightly, the methods they use to treat meibomian gland dysfunction are the same.
Each treatment involves placing an instrument over the upper or lower eyelid. The instrument administers heat ranging from 100°F to 111°F to the area. This heat loosens the stagnant meibum clogging the meibomian glands.
Once the meibum is loosened, the device puts pressure on the eyelids to help remove it from the glands. Lipiflow and iLUX treatments take around 12 minutes per eye and render very similar results. A study comparing iLUX and LipiFLow found no significant difference between the two in regard to their effectiveness in treating meibomian gland dysfunction.
Intense pulsed light for dry eye (IPL)
Intense pulsed light (IPL) has long been used to treat rosacea on the skin. Rosacea on the skin and eyelid often occurs together.
Ocular rosacea is characterized by dilated blood vessels coursing along the eyelash margin in patients suffering from blepharitis and may contribute to dry eye symptoms.
In IPL treatment, a hand-held device flashes bright light onto the skin. The light is filtered to allow only wavelengths that can be absorbed by the dilated blood vessels. It’s believed that treating the dilated vessels helps with associated inflammation that contributes to dry eye symptoms.
Many patients experience relief from their dry eye symptoms after IPL and become less dependent on other measures to keep their eyes comfortable. For this reason, IPL treatment may be well-suited for DED patients who don't want to be troubled by the inconvenience of frequent eye drop use.
Patients usually require four to six monthly IPL treatments for optimum effects. It's important to discuss details with your doctor to determine if IPL treatment is right for you.
IPL treatment is not covered by health insurance or vision insurance, and it may not be appropriate for patients with certain skin pigmentations.
Warm compress
An alternative (and potentially more comfortable) way to help open clogged meibomian glands is to apply warm compresses to closed eyelids to soften the hardened meibum.
The best type of warm compress is one that stays hot for at least five minutes. Studies have shown that meibum doesn’t soften adequately if the eyelids are heated for a shorter time. And a hot washcloth, besides being messy, will generally need to be reheated before five minutes have passed.
Studies have also shown that applying moist heat is the best. You can find compresses that deliver moist heat for the appropriate amount of time at drugstores or your doctor’s office.
The recommended application time for warm compresses is between five and 10 minutes. The length of time that the compresses should be heated in the microwave will be indicated in the instructions. It is important to make sure that the compresses are comfortably hot and do not burn the eyelids. The more often the warm compresses are applied the better, but twice a day is most practical for many patients.
Additional treatments for advanced DED
For patients with severe DED, especially when other treatments have failed, there are several advanced treatments. These are usually only available in eye centers that specialize in dry eye care.
One such therapy is called autologous serum tears and involves the regular application of diluted blood serum to the eye. Blood serum contains anti-inflammatory molecules as well as nutrients and antioxidants. This treatment does require a blood draw and is usually not covered by insurance.
Another treatment is the application of a sterile amniotic membrane to an eye damaged by severe DED. The amniotic membrane stays in place for two to seven days to allow the eye to heal. Amniotic membranes contain molecules that have anti-inflammatory and anti-scarring properties.
Finally, a fitting with a scleral lens (a special type of large rigid contact lens) may allow the eye to heal. The lens will keep saline solution and tears on the surface of the eye. Some patients may have a tough time inserting such a large lens, but most can learn.
Nutritional supplements
Doctors sometimes recommend nutritional supplements as part of a holistic dry eye treatment plan.
Experts believe that supplements containing omega-3 fatty acids can help dry eyes. Good sources of omega-3s include cold-water fish such as salmon, sardines, herring and cod. For a vegetarian source of omega-3s, some eye doctors recommend flaxseed, chia seeds, walnuts and kidney beans, among other options.
Drinking more water might also help relieve dry eye symptoms. Dehydration often makes dry eye problems worse. This is especially true during hot, dry and windy weather.
Home remedies
If you have mild dry eye symptoms, there are several things you can try to get relief before going to the doctor:
Blink more often. Research has shown that people tend to blink much less frequently than normal when viewing a computer, smartphone or other digital display. This decreased blink rate can cause or worsen dry eye symptoms. Make a conscious effort to blink more often when using these devices. Also, perform full blinks, gently squeezing your eyelids together, to fully spread a fresh layer of tears over your eyes.
Take frequent breaks during computer use. A good rule of thumb here is to look away from your screen at least every 20 minutes. When you do this, look at something at least 20 feet from your eyes and focus on it for at least 20 seconds. Eye doctors call this the "20-20-20 rule," and following it can help relieve dry eyes and computer eye strain.
Thoroughly remove eye makeup. Eyeliner and other eye makeup can clog the openings of the glands at the base of the eyelashes, leading to meibomian gland dysfunction and evaporative dry eye. At the end of the day, be diligent about removing all makeup from your eyelids and eyelashes.
Clean your eyelids. When washing your face before bedtime, gently wash your eyelids to remove bacteria that can cause blepharitis and meibomian gland problems that lead to dry eye symptoms. Wash your lids and lashes with a mild cleanser, such as diluted baby shampoo or pre-moistened eyelid wipes sold in drugstores.

Wraparound-style eyewear with side shields can protect your eyes from moisture-robbing wind and irritating debris.
Wear quality sunglasses. Sun exposure and dry climate can contribute to dry eyes. When outdoors in daylight hours, always wear sunglasses that block 100% of the sun's UV rays.
Use a humidifier. Dry air inside your home, particularly in dry climates, or in cold climates in winter, can contribute to making your eyes dry. Consider adding a humidifier to increase the relative humidity inside your home.
READ MORE about home remedies for dry eyes
Risk factors and prevention
While dry eye syndrome can affect anyone, there are certain characteristics that put a person at a higher risk of developing symptoms. Some of these risk factors include:
Being over the age of 50
Being female
Having certain autoimmune or inflammatory diseases, like Sjogren’s syndrome or lupus
Wearing contact lenses
Taking hormones, like birth control or hormone replacement therapy
Having a vitamin deficiency, specifically in vitamin A
Some risk factors are beyond a person’s control. Fortunately, there are some things you can do to prevent or reduce symptoms of dry eye, such as:
Using artificial tears or ointments at bedtime to avoid dry eye in the morning
Avoiding things like blow dryers, desk fans, and other sources of forceful air flow
Adding humidity to particularly cold or warm rooms by using a humidifier or placing a pan of water next to your radiator
Incorporating more vitamins into your diet, like vitamin A and omega-3 fatty acids
Protecting your eyes from wind, pollution and other irritants by wearing sunglasses when outside
Staying hydrated by drinking plenty of water
When to see an eye doctor
If home remedies, prevention measures and over-the-counter treatment do not seem to improve your symptoms, or if your symptoms get worse, it may be time to see an eye doctor.
It’s possible that your dry eye symptoms are caused by an underlying condition. In this case, treatment for the primary cause may be required. Your eye doctor can assess your symptoms and their severity and establish the appropriate treatment route for you.
READ MORE: Infographic: Dry eye syndrome
What is dry eye? Symptoms, causes and treatment. American Academy of Ophthalmology. EyeSmart. July 2022.
Dry eye. National Eye Institute. April 2022.
Dry eye. American Optometric Association. Accessed January 2023.
Chronic dry eye. Healthy Women. Accessed January 2023.
Dry eye disease: when to treat and when to refer. Australian Prescriber. October 2018.
Dry eye syndrome. Mount Sinai. December 2020.
How hormones can affect eyes and vision. American Academy of Ophthalmology. EyeSmart. October 2018.
Preparation is key to fighting dry eye while traveling. Optometry Times. July 2022.
Better manage nocturnal lagophthalmos for dry eye patients. Optometry Times. February 2020.
Face mask-associated ocular irritation and dryness. Ophthalmology and Therapy. July 2020.
Increased screen time and dry eye: another complication of COVID-19. Eye & Contact Lens: Science & Clinical Practice. August 2021.
Prevalence of dry eye syndrome in association with the use of contact lenses in Saudi Arabia. BMC Ophthalmology. March 2021.
Nocturnal lagophthalmos and sleep quality in patients with dry eye disease. Life. July 2020.
Dry eye. Better Health Channel. April 2021.
Tear system. Cleveland Clinic. Accessed November 2022.
Dry eye. Johns Hopkins Medicine. Accessed November 2022.
Tear breakup time (TBUT). University of Iowa Ophthalmology and Visual Sciences. Accessed November 2022.
Is it or isn't it dry eye? The Ophthalmologist. December 2021.
The TearLab osmolarity system FAQs. Tear Lab. Accessed November 2022.
InflammaDry. Quidel. Accessed January 2023.
Dyes in ophthalmology. American Academy of Ophthalmology. EyeWiki. July 2022.
Restasis (eye drops) uses, dosage, side effects. Drugs.com. May 2022.
Practical guidance for the use of cyclosporine ophthalmic solutions in the management of dry eye disease. Clinical Ophthalmology. July 2019.
Xiidra: uses, dosage, side effects & warnings. Drugs.com. October 2022.
Tyrvaya (varenicline solution) nasal spray. Tyrvaya. Accessed January 2023.
Punctal plugs. American Academy of Ophthalmology. March 2022.
Non‐pharmaceutical treatment options for meibomian gland dysfunction. Clinical and Experimental Ophthalmology. April 2021.
Comparison of the iLUX and the LipiFlow for the treatment of meibomian gland dysfunction and symptoms: a randomized clinical trial. Clinical Ophthalmology. February 2020.
Intense pulsed light (IPL) therapy. American Academy of Ophthalmology. EyeWiki. September 2022.
Intense pulsed light therapy in the treatment of meibomian gland dysfunction: current perspectives. Clinical Optometry. October 2019.
Meibomian gland dysfunction and treatment. American Association for Pediatric Ophthalmology and Strabismus. December 2020.
Not a dry eye in the house: latest treatments. Review of Ophthalmology. October 2022.
The benefits of fish oil for dry eye. American Academy of Ophthalmology. EyeSmart. October 2020.
Efficacy of omega-3 fatty acid supplementation for treatment of dry eye disease: a meta-analysis of randomized clinical trials. Cornea. January 2019.
The 20-20-20 rule. Canadian Association of Optometrists. Accessed January 2023.
Effects of eye cosmetics usage, knowledge, hygiene and management towards dry eye symptoms among university students. Malaysian Journal of Medicine and Health Sciences. October 2022.
Dry eye syndrome. MedlinePlus [Internet]. Bethesda (MD): National Library of Medicine (US). December 2020.
TFOS DEWS II Report. Tear Film and Ocular Surface Society. Boston, MA, USA. Accessed January 2023.
Floppy eyelid syndrome: a comprehensive review. The Ocular Surface. January 2020.
Page published on Monday, 16 March 2020
Medically reviewed on Saturday, 28 January 2023






