Strabismus and crossed eyes explained

Strabismus is a misalignment of the eyes, making it impossible for them work together as a team.
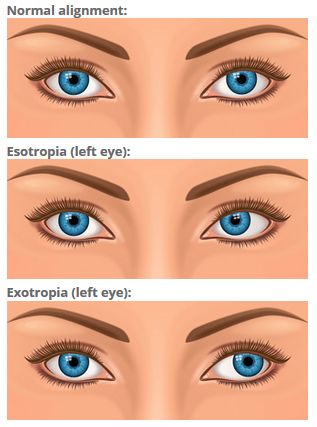
If you have strabismus, one eye looks directly at the object you are viewing, while the other eye is misaligned inward (esotropia, or "cross-eyed"), outward (exotropia), upward (hypertropia) or downward (hypotropia).
Strabismus can be constant or intermittent. Also the misalignment might always affect the same eye (unilateral strabismus), or the two eyes may take turns being misaligned (alternating strabismus).
To prevent double vision from congenital and early childhood strabismus, the brain ignores the visual input from the misaligned eye, which typically leads to amblyopia or "lazy eye" in that eye.
Different studies provide different estimates of the prevalence of strabismus among children and teenagers worldwide. Most research suggests about 1 to 3 percent of the global population has strabismus.
Strabismus signs and symptoms
The primary sign of strabismus is a visible misalignment of the eyes, with one eye turning in, out, up, down or at an oblique angle.
Corneal light reflex (Hirschberg) test: A screening test for strabismus that evaluates eye alignment based on the location of reflections of light shined at the eyes.
When the misalignment of the eyes is large and obvious, the strabismus is called "large-angle," referring to the angle of deviation between the line of sight of the straight eye and that of the misaligned eye. Less obvious eye turns are called small-angle strabismus.
Typically, constant large-angle strabismus does not cause symptoms such as eye strain and headaches because there is virtually no attempt by the brain to straighten the eyes. As a result, if left untreated, large-angle strabismus usually causes severe amblyopia in the turned eye.
Less noticeable cases of small-angle strabismus are more likely to cause disruptive visual symptoms, especially if the strabismus is intermittent or alternating. In addition to headaches and eye strain, symptoms may include an inability to read comfortably, fatigue when reading and unstable or "jittery" vision. If small-angle strabismus is constant and unilateral, it can lead to significant amblyopia in the misaligned eye.
Both large-angle and small-angle strabismus can be psychologically damaging and affect the self-esteem of children and adults with the condition, as it interferes with normal eye contact with others, often causing embarrassment and awkwardness.
Newborns often have intermittent crossed eyes due to incomplete vision development, but this frequently disappears as the infant grows and the visual system continues to mature. Most types of strabismus, however, do not disappear as a child grows.
Routine children's eye examinations are the best way to detect strabismus. Generally, the earlier strabismus is detected and treated following a child's eye test, the more successful the outcome. Without treatment, your child may develop double vision, amblyopia or visual symptoms that could interfere with reading and classroom learning.
What causes strabismus?
Each eye has six external muscles (called the extraocular muscles) that control eye position and movement. For normal binocular vision, the position, neurological control and functioning of these muscles for both eyes must be coordinated perfectly.
Strabismus occurs when there are neurological or anatomical problems that interfere with the control and function of the extraocular muscles. The problem may originate in the muscles themselves, or in the nerves or vision centres in the brain that control binocular vision.
Genetics also may play a role: If you or your spouse has strabismus, your children have a greater risk of developing strabismus as well.
Accommodative esotropia
Occasionally, when a long sighted child tries to focus to compensate for uncorrected long-sightedness, he or she will develop a type of strabismus called accommodative esotropia, where the eyes cross due to excessive focusing effort.
This condition usually appears before 2 years of age but also can occur later in childhood.
Often, accommodative esotropia can be fully corrected with glasses or contact lenses.
Strabismus surgery
In some cases, the only effective treatment for a constant eye turn is strabismus surgery.
If your optometrist finds that your child has strabismus, he or she can refer you to an ophthalmologist who specialises in strabismus surgery.
The success of strabismus surgery depends on many factors, including the direction and magnitude of the eye turn. In some cases, more than one surgery may be required. The strabismus surgeon can give you more information about this during a pre-surgical consultation.
Strabismus surgery also can align the eyes of adults with long-standing strabismus. In many cases of adult strabismus, however, a significant degree of amblyopia may remain even after the affected eye is properly aligned. This is why early treatment of strabismus is so important.
The earlier strabismus is treated surgically, the more likely it is that the affected eye will develop normal visual acuity and the two eyes will function together properly as a team.
Non-surgical strabismus treatment
In some cases of intermittent and small-angle strabismus, it may be possible to improve eye alignment non-surgically with vision therapy.

Esotropia (crossed eyes) needs to be treated early in life to prevent amblyopia.
For example, convergence insufficiency (CI) is a specific type of intermittent exotropia in which the eyes usually align properly when viewing a distant object, but fail to achieve or maintain proper alignment when looking at close object, such as when reading, resulting in one eye drifting outward.
Convergence insufficiency can interfere with comfortable reading, causing eye strain, blurred vision, double vision and headaches.
There also is some evidence that suggests CI can cause attention problems and affect academic performance in children. One study found that children with exotropia (including convergence insufficiency) at an early age were significantly more likely to develop attention deficit hyperactivity disorder (ADHD), adjustment disorder and learning disabilities by early adulthood.
Certain types of strabismus also have been associated with an increased risk of myopia. A study that monitored 135 children with intermittent exotropia over a 20-year period and found that more than 90 percent of these children became myopic by the time they reached their 20s.
It appears non-surgical vision therapy can be an effective treatment for convergence insufficiency. Published research has shown that 73 percent of children with symptomatic convergence insufficiency had a successful or improved outcome following a 12-week program of vision therapy combined with eye exercises performed at home.
Sometimes, a strabismus surgeon may recommend a program of vision therapy for a period of time after strabismus surgery to treat amblyopia and other binocular vision problems that may remain after surgery. In these cases, the term "orthoptics" ("ortho" = straight; "optics" = eyes) rather than "vision therapy" might be used to describe this treatment.
Questions to ask
When consulting with your optometrist or strabismus surgeon prior to treatment, here are a few important questions to ask:
If surgery is recommended, enquire whether one surgery will suffice or if additional procedures are likely to be necessary.
Ask the eye surgeon about the success rates for the type of strabismus and the surgery he or she is recommending.
Ask what criteria are used to determine if the treatment is a success. In other words, is "success" defined as reducing the eye turn so the eyes are better aligned and look more natural in appearance, or is success defined as eyes that are perfectly aligned with normal visual acuity, eye teaming and depth perception.
For optometrists or orthoptists, ask about the success rate, likely duration and costs of vision therapy (or orthoptics).
Remember, children do not "outgrow" strabismus. For best visual outcomes and to prevent developmental delays and other problems, seek treatment for strabismus as soon as possible.
Page published on Monday, 16 March 2020






