Cornea transplant surgery (keratoplasty)
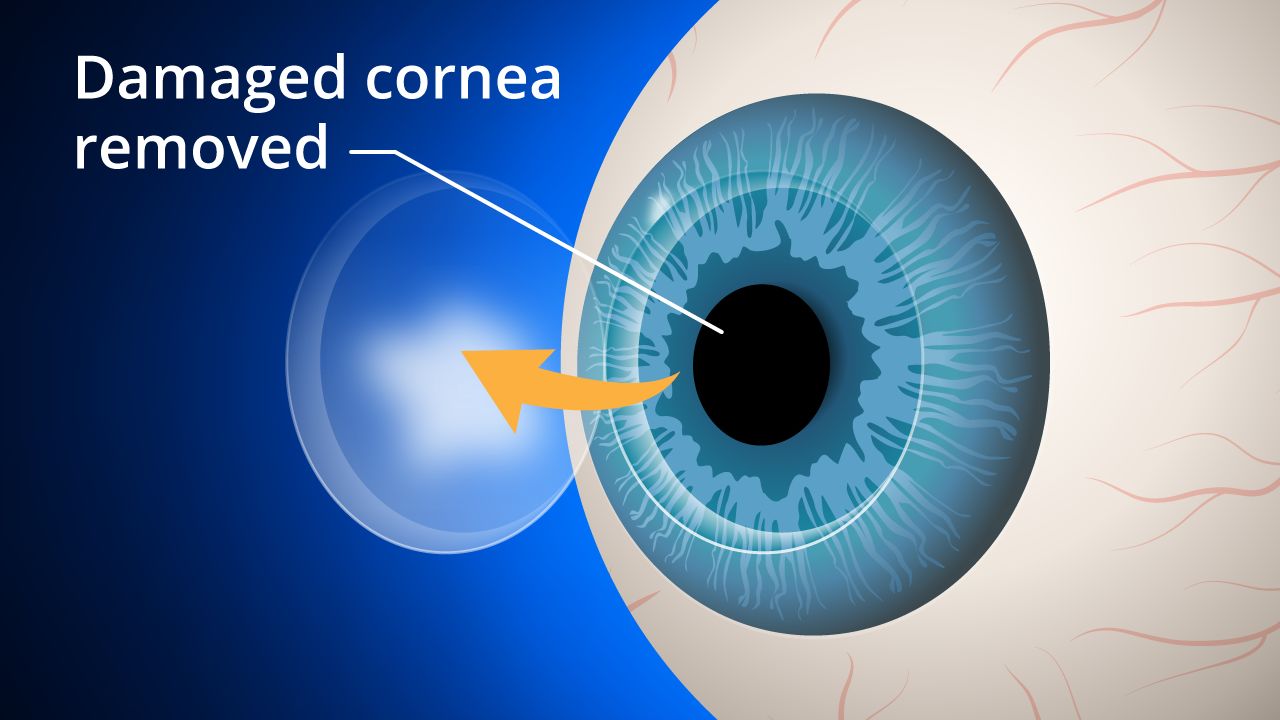
A cornea transplant replaces diseased or scarred corneal tissue with healthy tissue from an organ donor.
There are two main types of cornea transplants: Full thickness cornea transplant surgery (also known as penetrating keratoplasty) and back layer cornea transplant surgery (also known as endothelial keratoplasty).
In these procedures the portion of the cornea that has been damaged due to disease or injury, is replaced with healthy corneal tissue (usually from a donor program). An unhealthy cornea affects your vision by scattering or distorting light and causing glare and blurred vision. A cornea transplant may be necessary to restore your functional vision.
Corneal eye disease is the fourth most common cause of blindness (after cataracts, glaucoma and age-related macular degeneration) and affects more than 10 million people worldwide, according to the World Health Organization.
Do you need a corneal transplant?
A healthy, clear cornea is essential for good vision. If your cornea is damaged due to eye disease or eye injury, it can become swollen, scarred or severely misshapen and distort your vision.
A cornea transplant may be necessary if eyeglasses or contact lenses can't restore your functional vision, or if painful swelling can't be relieved by medications or special contact lenses.
Conditions that can affect the clarity of your cornea and put you at risk of needing a corneal transplant include:
Scarring from infections, such as eye herpes or fungal keratitis
Scarring from trichiasis (a condition where eyelashes grow inwardly, toward the eye, and rub against your cornea)
Hereditary conditions such as Fuchs' dystrophy
Eye diseases such as advanced keratoconus
Corneal ectasia (thinning of the cornea and irregular corneal shape)
Rare complications from LASIK surgery
Chemical burns of the cornea or damage from an eye injury
Excessive swelling (edema) of the cornea
Graft rejection following a previous corneal transplant
Corneal failure due to cataract surgery complications
Are you a corneal transplant candidate?
A cornea transplant is performed to improve the function of the cornea and improve vision. If pain is caused by a significantly diseased or damaged cornea, a cornea transplant may relieve that symptom.
With these factors in mind, you also should consider several important questions before you decide to undergo a corneal transplant:
Does your functional vision impede your job performance or your ability to carry out daily activities?
Can your vision be corrected with special contact lenses or other less invasive measures?
Are you able to take enough time off from work or school (up to six months to a year in some cases) to recover properly?
All of these questions, in conjunction with a thorough screening and consultation with your eye care professional, must be carefully considered before you make the final decision to have a corneal transplant.
Before a keratoplasty procedure
If you and your eye care professional decide a cornea transplant is the best option for you, your name may placed on a waiting list. You may need to wait some time for suitable tissue from a donor eye to become available for a corneal transplant.
Before a donor cornea is released for use in transplant surgery, it is checked for clarity and screened for the presence of any diseases such as hepatitis and AIDS, in accordance with the appropriate medical regulatory organization.
During a corneal transplant
Your eye surgeon will first administer either local or general anesthesia, depending on your health, age, eye injury or disease, and whether or not you prefer to be asleep during the procedure.
If local anesthesia is used, an injection is made into the skin around your eye to relax the muscles that control blinking and eye movements, and eye drops are used to numb your eye. You will be awake during the procedure and most people don't report any discomfort.
After the anesthesia has taken effect, an instrument called a lid speculum is used to keep your eyelids open. Your surgeon then measures the affected corneal area to determine the size of the donor tissue needed.
Traditional corneal transplant surgery. During traditional corneal transplant surgery (penetrating keratoplasty) a circular button-shaped, full-thickness section of your damaged cornea is removed with a surgical instrument called a trephine or with a femtosecond laser.
A matching corneal "button" is then removed from the donor eye and positioned and sutured into place on your cornea. The sutures (stitches) remain in place typically for a year or more after surgery.
Lastly, a plastic shield is placed over your eye to protect it during healing.
Penetrating keratoplasty surgery generally takes one to two hours and most procedures are performed on an outpatient basis, meaning you can go home a short while after the surgery. (You will need someone to drive you home.)
Endothelial keratoplasty. In endothelial keratoplasty, only the innermost layer of the cornea (called the endothelium) is replaced, leaving the overlying healthy corneal tissue intact. (The endothelium controls the fluid balance in the cornea, and if it becomes damaged or diseased, this can cause significant corneal swelling and loss of vision.)
During an endothelial keratoplasty (EK) procedure, the eye surgeon makes a tiny incision and places a thin disc of donor tissue containing a healthy endothelial cell layer on the back surface of your cornea. An air bubble is used to position the new endothelial layer into place. The small incision is self-sealing and typically no sutures are required.
Endothelial keratoplasty has several advantages over full-thickness penetrating keratoplasty. These include:
Faster recovery of vision
Less operating time
Minimal removal of corneal tissue
No related suture complications
Faster recovery of vision
Reduced risk of astigmatism after surgery
Less impact on the structural integrity of the eye and less susceptibility to injury after surgery
The EK corneal graft procedure has become the preferred technique for patients with Fuchs' dystrophy and other endothelial disorders of the cornea. However, traditional full-thickness penetrating keratoplasty is the best treatment if much of your cornea is diseased or scarred.
Recovering from a corneal transplant
Total cornea transplant recovery time can be up to a year or longer.
Initially, your vision will be blurry for the first few months — and in some cases may be worse than it was before — during the initial stage of the healing process.
As your vision improves, you gradually will be able to return to your normal daily activities. For the first several weeks, heavy exercise and lifting are prohibited. However, you should be able to return to work within a week after surgery, depending on your job and how quickly your vision improves.
Steroid eye drops will be prescribed for several months to help your body accept the new corneal graft, as well as other medications to help control infection, discomfort and swelling.
You should keep your eye protected at all times by wearing a shield or a pair of eyeglasses so that nothing inadvertently bumps or enters your eye.
If stitches were used in your keratoplasty, these usually are removed three to 17 months after the procedure, depending on the health of your eye and the rate of healing.
If needed, adjustments can be made to the sutures surrounding the new corneal tissue to help reduce the amount of astigmatism resulting from an irregular eye surface.
As with any type of surgery, always follow the instructions of your eye surgeon to help minimize corneal transplant complications and expedite healing.
Cornea graft rejection
Cornea transplants are performed routinely and have a reasonable success rate. In fact, cornea grafts are the most successful of all tissue transplants.
Like any other surgical procedure, a cornea transplant comes with certain risks. For most people, having their vision improved or restored outweighs the potential complications associated with cornea transplant surgery. But all risks should be understood and considered before undergoing a keratoplasty procedure.
Complications of a corneal transplant can be significant and can include corneal graft rejection, eye infection and problems associated with the use of stitches.
Rejection of the donor tissue is the most serious complication after a corneal transplant. This occurs in 5% to 30% of patients. Transplant rejection is when your body's immune system detects the donor cornea as a foreign body and attacks and tries to destroy it.
One study found that having glaucoma and corneal swelling associated with previous cataract surgery can increase your chances of cornea graft rejection.
Warning signs and treatment
Recognizing the main warning signs of corneal transplant rejection is the first step to preventing graft failure.
These can be remembered using the acronym RSVP:
Vision loss
Pain
Rejection signs may occur as early as one month or as late as several years after surgery.
Your eye care professional will prescribe medication that can help reverse the rejection process. If detected early, the graft will be successful 9 out of 10 times, according to the Cornea Research Foundation of America.
Should your graft fail, corneal transplant surgery can be repeated. While repeat surgery generally has good outcomes, overall rejection rates increase with the number of corneal transplants you have.
Vision after a cornea transplant
Your eyesight should gradually improve a few weeks after a corneal graft, but it could take anywhere from a couple of months up to a year to have stable vision in the eye that receives the donor tissue.
You may be left with a degree of myopia (nearsightedness) and astigmatism, because the curve of the donor corneal tissue can't match exactly the curve of your natural cornea.
Correcting your vision following keratoplasty can be somewhat unpredictable and it's possible that significant astigmatism may be present after a cornea transplant procedure.
Mild refractive errors caused by corneal transplant surgery can be corrected with glasses; otherwise contact lenses are required.
Rigid gas permeable contact lenses and hybrid contact lenses usually are the most suitable contacts for corneal transplant patients due to the irregularity of the cornea after transplant. However, soft contact lenses sometimes are an option as well.
Because your vision will fluctuate during the first few months following your surgery, you should wait until your eye care professional says your vision is stable before you fill an eyeglass prescription or are fitted with contact lenses.
After your eye has fully healed and any stitches have been removed, you may be eligible to undergo laser eye surgery such as LASIK or PRK to improve your ability to see with or without glasses or contacts by reducing myopia and astigmatism.
Artificial corneas and biosynthetic corneas
Human donor tissue is the preferred — and most successful — option for replacing a diseased or injured cornea. However, for patients who are at high risk of corneal transplant failure with human donor tissue (patients who have experienced previous graft rejections with human cornea transplants) and have no other options to improve vision, artificial cornea tissue might be used.
An artificial cornea (also called a keratoprosthesis) is made from a biologically inert material. A cornea transplant procedure using an artificial cornea typically is reserved for patients who have:
A severe autoimmune disease
Chemical burns
Limited or no access to human donor tissue; or
Had multiple previous human donor cornea transplant failures
Another area of ongoing research is the development of biosynthetic corneal tissue from a human gene that regulates the natural production of collagen (the most common structural protein in the body, which can regenerate and repair damaged eye tissue).
While the field of biosynthetic corneas is still in its infancy, this approach potentially could be an effective option if human donor tissue is not appropriate or available.
FIND AN OPTICIAN: if you're concerned about your vision, visit an optician near you.
Page published on Wednesday, 16 March 2022







