Are There More Than 3 Types of Cataracts?
What are the three types of cataracts?
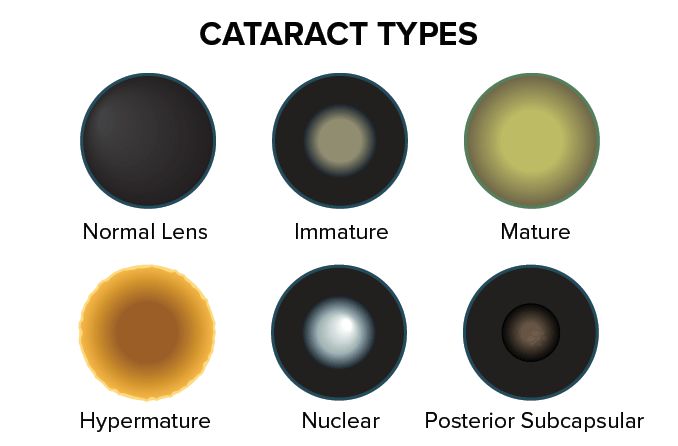
The three most common types of cataracts are nuclear, cortical and posterior subcapsular cataracts. Each one affects a different part of your eye's lens. They're usually caused by natural changes inside your lens as you get older.
There are other types of cataracts, too. Some develop after you get hurt or alongside another health problem. They can also happen for other reasons.
Surgery is the only way to treat a cataract for good.
Age-related cataracts
Most cataracts start to develop sometime after you turn 40. They happen when microscopic proteins in your eye's lens break down and clump together over time. After a while, these clumps look like cloudy areas on the lens.
This cloudiness is what causes the vision problems people can experience with cataracts. It interferes with light being able to properly focus on the retina.
You can get age-related cataracts in one eye or both.
The three main types are:
Nuclear
Cortical
Posterior subcapsular
Nuclear cataracts
A nuclear cataract is cloudiness in the "core" of your lens. It's one of the most common types of cataracts.
The center of your lens turns yellow and gets harder as you age. This is a normal part of the aging process called nuclear sclerosis. If it gets severe enough, it becomes a nuclear cataract.
Nuclear cataracts can cause blurry vision, dull colors, poor vision in low light, and other eyesight problems. They can make it look like you're looking through a dirty window or a smudgy pair of glasses. Updated glasses won’t solve the vision problem.
Cortical cataracts
Clouding in a cortical cataract starts along the edge of the lens. It's another common type.
At first, cortical cataracts can be shaped like white wheel spokes or wedges. Over time, they spread farther into the center of the lens and block more light from reaching the retina. That makes your cataract symptoms worse.
The most common symptom is glare, which can make bright lights (like car headlights) much more distracting. Cortical cataracts can also hurt your near vision, distance vision and contrast sensitivity (how well you can see light objects against other light objects).
Posterior subcapsular cataracts
A posterior subcapsular cataract (PSC) is cloudiness in the back layer of your lens. They don't happen as often as nuclear and cortical cataracts, but they are more common in younger people.
Many PSCs grow faster than other types of age-related cataracts. This can make your vision worsen more quickly.
People with a PSC can experience glare and difficulty seeing in bright light. It can also be harder to see near or far objects, but near-distance vision problems are more common.
Less common types of cataracts
Cataracts aren't always related to someone's age. In addition to other types, these can be:
Anterior subcapsular
Traumatic
Snowflake
Christmas tree
Anterior subcapsular cataracts
An anterior subcapsular cataract (ASC) is located along the front of your lens.
Many ASCs occur after an eye injury. Some develop when another medical condition or treatment causes inflammation in the eye.
Sometimes, doctors don't know why they happen.
Traumatic cataracts
A traumatic cataract usually develops after someone hurts their eye. Injuries can be blunt (something like a ball that makes forceful contact with the eye area) or penetrative (something enters the eye).
They can also happen to people who are electrocuted, burned with chemicals or exposed to high levels of certain radiation.
Traumatic cataracts can form within hours or even minutes of an eye injury. Some of them take months or years to develop.
Many traumatic cataracts are shaped like a rose (rosette) or star (stellate).
Snowflake cataracts
People with diabetes are up to five times more likely to get cataracts, including snowflake cataracts. They're also called "diabetic cataracts," but it's much more common for diabetes to cause cortical, posterior subcapsular or other types of cataracts.
Snowflake cataracts cause a cloudy area in the center of the lens with "arms" that extend toward the edge. It can resemble the shape of a snowflake.
Most of these cataracts affect young people who have uncontrolled or undiagnosed diabetes. In some cases, it's the first sign of diabetes a doctor sees.
Christmas tree cataracts
Christmas tree cataracts don't cause gray-white clouding like most other types do. Instead, they're made of many iridescent specks that can look like the reflection of Christmas tree lights in your eye.
Their medical name is polychromatic cataracts. Polychromatic comes from the Ancient Greek words for "many colors."
Christmas tree cataracts are rare. They're more common in people who have a muscular disease called myotonic dystrophy.
Pediatric cataracts
Children can get cataracts too, but it’s rare. They can develop any time, even before a child is born.
Many different types of cataracts can impact a child's eyesight. Together, they're known as pediatric cataracts.
Some of them are:
Congenital
Posterior polar
Cerulean
Congenital cataracts
Congenital cataracts are present at birth. Around one in every 2,400 newborns is diagnosed with this rare condition.
Roughly one-third of congenital cataracts are caused by another disease. A third of cases are caused by genetic traits passed down by a parent, and a third happen for an unknown reason.
About one in every 250 newborns has at least some cloudiness on their lens. Most of these cases are very mild and never progress or cause vision problems. It’s possible to never even know about it unless an ophthalmologist examines your eyes for another reason.
Posterior polar cataracts
Posterior polar cataracts (PPC) are one type of congenital cataract. They're also rare, but researchers don't know exactly how rare they are.
A PPC is a cloudy area on the back-center part of the lens. Some of them resemble a bull's eye or the rings of an onion.
Most of the time, PPCs affect both eyes. They can be diagnosed any time, but some don't cause noticeable symptoms until someone is 30 to 50 years old.
Cerulean cataracts
A cerulean cataract is a rare eye problem that looks like pale, blue-white spots on the lens. This is why many people call them "blue dot cataracts."
Most children don't show symptoms until they're 18 to 24 months old. Surgery is the only treatment, but many people wait until they're adults to have the procedure.
Secondary cataracts
Cataract surgery helps millions of Americans every year, but it can cause a common complication called posterior capsule opacification (PCO). It's also known as a "secondary cataract."
A secondary cataract is cloudiness that develops behind your new artificial lens in the natural lens capsule. As many as half of all patients get it within five years of their surgery. It isn't a true cataract, but it can cause similar vision problems.
Fortunately, it's easy to treat using a non-invasive procedure called YAG laser capsulotomy. Most people only need it once.
READ MORE: What to expect before, during and after cataract surgery
Cataract. EyeWiki. American Academy of Ophthalmology. May 2023.
What are cataracts? EyeSmart. American Academy of Ophthalmology. September 2022.
Cataracts. National Eye Institute. January 2023.
Cataract. American Optometric Association. Accessed May 2023.
Bilateral anterior subcapsular cataract development following initiation of enfortumab vedotin. International Medical Case Reports Journal. October 2021.
Traumatic cataract surgery. EyeWiki. American Academy of Ophthalmology. February 2023.
Cataract in diabetes mellitus. World Journal of Diabetes. March 2019.
Cataracts and their treatment in people with diabetes. ADA Clinical Compendia. May 2019.
Newborn with bilateral congenital cataracts: Never forget congenital rubella syndrome. Paediatrics & Child Health. March 2020.
Posterior polar cataract. EyeWiki. American Academy of Ophthalmology. January 2023.
Posterior polar cataract. StatPearls [Internet]. December 2022.
Cerulean cataract. EyeWiki. American Academy of Ophthalmology. February 2023.
Cerulean cataract. National Center for Advancing Translational Sciences. February 2023.
Cataract surgery practice patterns worldwide: A survey. BMJ Open Ophthalmology. January 2021.
What is posterior capsulotomy? EyeSmart. American Academy of Ophthalmology. September 2022.
Posterior capsular opacification. Cleveland Clinic. February 2023.
Cataract. StatPearls [Internet]. July 2022.
Traumatic rosette cataract. BMJ Case Reports. November 2018.
Posterior capsule opacification. EyeWiki. American Academy of Ophthalmology. January 2023.
Page published on Thursday, August 20, 2020
Page updated on Tuesday, August 15, 2023
Medically reviewed on Thursday, June 22, 2023






