Corneal dystrophy: Conditions and symptoms
What is corneal dystrophy?
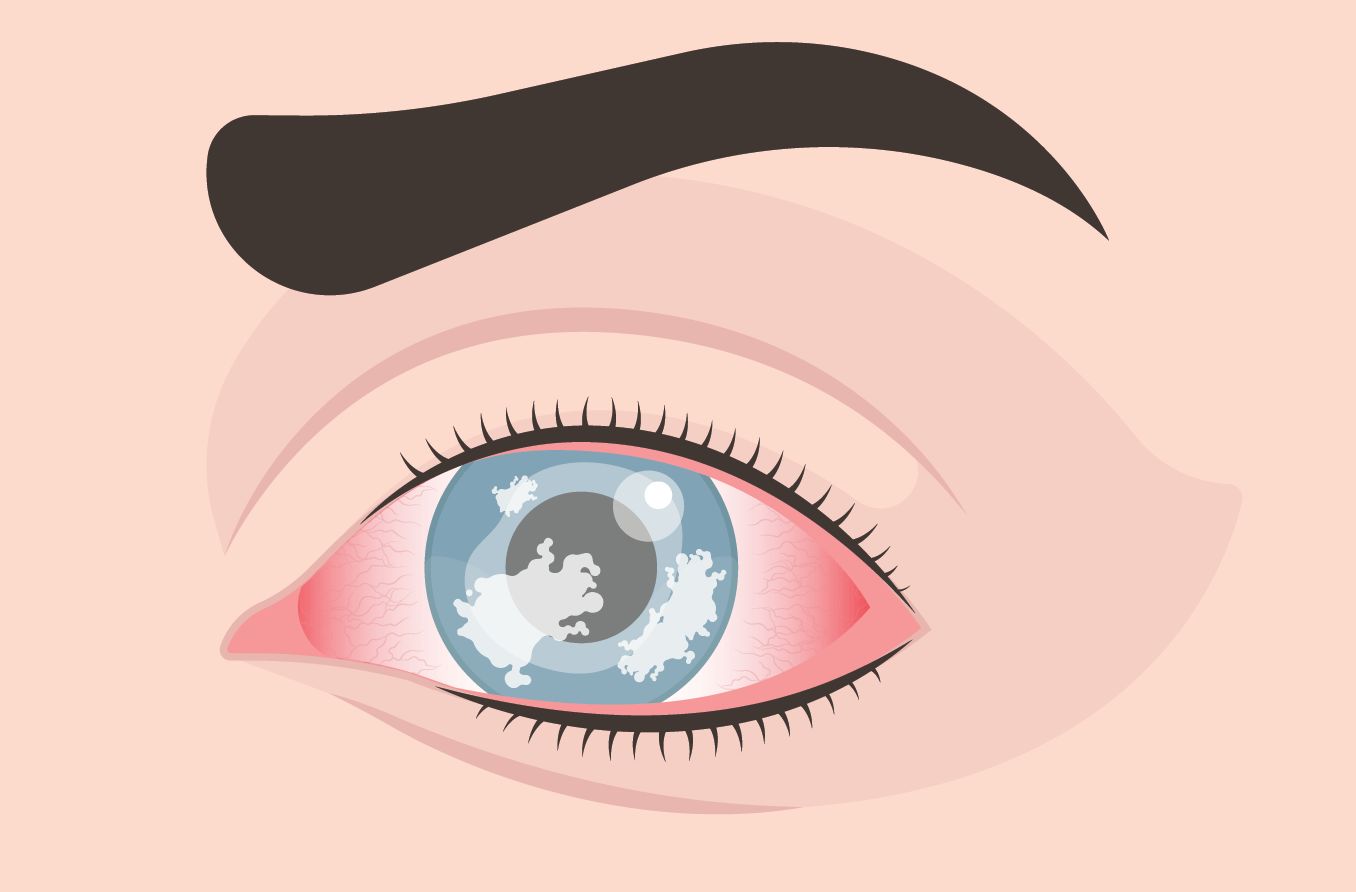
Corneal dystrophies are a group of over 20 corneal conditions that are slow-progressing, inherited disorders. They are non-inflammatory and result in a buildup of material in the cornea of both eyes. Typically, the dystrophy affects one layer of the cornea and progresses into the other layers.
At the beginning stages of the condition, patients often have few, if any, symptoms. Over time, the buildup of material causes the cornea to lose its transparency, resulting in progressive visual acuity loss, among other symptoms.
The cornea provides the majority of the focusing power of the eye. It is made of five layers — the epithelium, Bowman’s layer, the stroma, Descemet’s membrane and the endothelium. These five layers of the cornea provide structure and a progressive line of defense against disease and particles.
The average age that corneal dystrophy begins to affect the eyes varies among the different types but is generally between the early teens to 40s. This group of conditions is usually limited to the eyes and does not affect other areas of the body.
The corneal dystrophies are often categorized by which of the five layers of the cornea they affect:
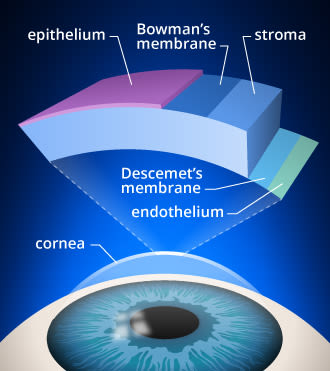
Layers of the cornea. Corneal cross-linking strengthens bonds in the stroma of the cornea, which is the layer from which tissue is removed during LASIK surgery.
Anterior – Epithelium and Bowman’s layer
Stromal – Stroma (middle layer)
Posterior – Descemet’s membrane and endothelium
Each dystrophy affects the layers of the cornea differently, and so the symptoms of cornea
l dystrophy are quite varied. Treatment includes eye drops and ointment, pain relievers, and medical and surgical management for severe cases.
SEE RELATED: Corneal deposits
What are the anterior corneal dystrophies?
The anterior dystrophies affect the anterior cornea, resulting in abnormalities in the epithelium and Bowman’s membrane, which are the protective layers of the cornea.

Corneal dystrophy [Image credit: Permission granted by © 2022 American Academy of Ophthalmology]
A symptom that a number of people with anterior corneal dystrophies suffer from is recurrent corneal erosion (RCE). This is when the corneal epithelium does not adhere to the eye properly and breaks down as soon as the eyes are opened after sleeping. It can lead to sudden onset of pain, foreign body sensation, blur, tearing and light sensitivity.
Map dot fingerprint corneal dystrophy
This dystrophy affects the epithelium and Bowman’s membrane. It causes an abnormal folding of the epithelium, giving the appearance of a map or fingerprint.
Although this does not always cause vision loss or pain, it can cause recurrent corneal erosions in about one in ten people who have this condition. It may cause changes in prescription as well.
Map dot corneal dystrophy is also known as “epithelial basement membrane disorder” (EBMD) or epithelial corneal dystrophy.
Meesmann corneal dystrophy
This condition is also known as juvenile epithelial dystrophy, as symptoms can appear as early as the first year of a baby’s life. This rare condition results in clusters of small, transparent cysts in the epithelium.
Symptoms include slight irritation and a small amount of blur and decrease in visual acuity. Excessive tearing and light sensitivity are also common. Corneal clouding is not common in Meesmann corneal dystrophy.
Reis bucklers corneal dystrophy
This anterior corneal dystrophy causes scarring and clouding of Bowman’s membrane, resulting in blurry vision or double vision in one eye. It often results in painful, recurrent corneal erosions and severe visual impairment in early childhood. By 20 years of age, decreased vision and foreign body sensation are typical. It is also known as granular corneal dystrophy type III.
What are the stromal (middle layer) corneal dystrophies?
The stoma is the middle corneal layer made of water and collagen. It provides 90% of the cornea’s thickness and gives it structure and elasticity. It is important to keep the stroma from swelling in order to keep the cornea transparent.
Keratoconus
Keratoconus (conical cornea) is considered an ectatic dystrophy. This means that the cornea gets progressively thinner and takes on a distorted, cone-like shape. It typically begins in adolescence and progresses into an individual’s 30’s. Although doctors are still not certain about the mechanism, loss of collagen in the cornea is commonly seen in the disease.
It is managed by glasses, contact lenses or surgical intervention. An outpatient procedure such as corneal cross-linking surgery can strengthen the bonds between collagen fibers in the cornea. This slows down the progression of the disease.
Lattice dystrophy
This dystrophy is due to abnormal overlapping protein fibers in the stroma (giving the appearance of a glass-like lattice). The protein fibers cause the cornea to become cloudy, decreasing vision.
There are two types of Lattice dystrophy:
Type I – This type often causes recurrent corneal erosions, vision loss and irregular astigmatism. Symptoms become significant in patients by their 20s and 30s.
Type II – This type has other medical disorders associated with it, such as dry, itchy and lax skin as well as cardiac abnormalities and facial paralysis.
The ocular symptoms of lattice dystrophy can be treated by drops and ointments. If symptoms become severe, a corneal transplant surgery may be necessary.
Granular corneal dystrophy
This stromal dystrophy also occurs in two variations:
Type I – This condition is said to resemble “breadcrumbs” because of the accumulation of small granules that give it this appearance. Early in the disease, there are no symptoms, but patients may experience a visual acuity decrease by their 40s or 50s. Light sensitivity and recurrent corneal erosions may occur as well.
Type II – This condition is also known as Avellino corneal dystrophy. The opacities develop early in life and are a mixture of Type I and lattice dystrophy. Patients who are older may have clouding of the cornea resulting in blurry and decreased vision.
Macular corneal dystrophy
This condition usually begins to cause clouding of the cornea after age 3 and during the first decade. It is due to deposits of abnormal material in the stroma. Eye irritation along with visual acuity loss are early symptoms. By age 20 or 30, vision loss may be severe. Painful recurrent erosion, decreased corneal sensation and light sensitivity are common symptoms.
Schnyder crystalline corneal dystrophy
This dystrophy usually begins in the early teens, but it can develop in babies as well. Fat and cholesterol deposits progressively accumulate and cause the stroma to become opaque. This results in blurred, hazy vision. Patients with this condition complain of worse vision in environments that cause glare.
What are the posterior corneal dystrophies?
These dystrophies affect the endothelium and Descemet’s membrane, a protective layer of collagen fibers. The endothelium is a single layer of cells that pump excess water out of the stroma to keep it from swelling (which would cause haziness and blurred vision).
Fuchs’ endothelial corneal dystrophy
This is the most common dystrophy. In fact, nearly 40% of corneal transplants were due to Fuchs’ according to a 2012 study.
It causes progressive damage to the endothelium as well as thickening of Descemet’s membrane. An important function of the endothelium is to pump fluid out of the stroma. This prevents the stroma from swelling and becoming cloudy. In Fuchs’ corneal disease, the number of functioning endothelial cells decreases with time, resulting in a swollen, cloudy stroma.
In the early stages of the disease, vision is most blurry in the morning because fluid builds up overnight and clears as the day progresses. In the later stages of the disease, the cornea stays swollen the entire day, causing constant blur.
Additional symptoms include:
Development of cataract
Foreign body sensation (grittiness, a feeling of something in the eye)
Glare and halos
Light sensitivity
Diminishing color vision contrast
This condition is more common in women. It can be treated by eye drops and ointments or even a hairdryer held at arm’s length to dry the corneal surface. Eventually, Fuchs’ dystrophy may require corneal transplant surgery or an endothelial keratoplasty (EK). An EK is a procedure that transplants healthy endothelial cells on the cornea.
READ MORE: Fuchs' corneal dystrophy: 7 things you should know
What is the treatment for corneal dystrophy?
There are over 20 types of corneal dystrophy, each affecting the corneal layers differently. Due to this, the symptoms and treatment for corneal dystrophy can vary. Treatment is very specific to the cause and severity of the disease.
Eye drops such as artificial tears and ointments can be used for comfort and relief. Glasses and contact lenses can treat decreased visual acuity. Contact lenses can also be used as a bandage or for protection.
As the dystrophy progresses, surgical intervention may be needed. This can include:
Penetrating keratoplasty (PK) – This is a full-thickness cornea transplant. A diseased cornea is replaced with a healthy donor cornea.
Endothelial keratoplasty (EK) – This is a partial corneal transplant that does not need stitches.
Phototherapeutic keratectomy (PTK) – The outermost diseased layers are removed by a laser to allow healthy tissue to regrow.
Can corneal dystrophies be prevented?
Unfortunately, corneal dystrophies cannot be prevented. Since they are a genetic disorder, they run in families. To diagnose corneal dystrophy, a doctor will ask about family history in addition to performing a thorough eye exam.
Staying current with routine comprehensive eye exams can help diagnose a corneal dystrophy early in children and adults. This will allow for treatment to begin as soon as possible and possibly slow down the progression of the disease. If you notice persistent eye pain or blurry vision, contact an eye doctor as soon as possible.
SEE RELATED: Keratoplasty Surgery
Corneal dystrophy. StatPearls [Internet]. August 2021
Corneal dystrophies. National Organization for Rare Disorders. Accessed October 2021.
Meesmann corneal dystrophy. American Academy of Ophthalmology. EyeWiki. June 2020.
Two cases of Reis-Bücklers corneal dystrophy (granular corneal dystrophy type III) caused by spontaneous mutations in the TGFBI gene. Journal of the American Medical Association. April 2006.
Anatomy of cornea and ocular surface. Indian Journal of Ophthalmology. February 2018.
Corneal stromal dystrophies. American Academy of Ophthalmology. EyeWiki. April 2021.
Schnyder crystalline corneal dystrophy. National Center for Biotechnology Information Genetic Testing Registry. Accessed October 2021.
Fuchs' dystrophy. John Hopkins Medicine. Accessed October 2021.
Facts about corneal disease. Columbia University Department of Ophthalmology. Accessed October 2021.
Keratoconus. Johns Hopkins Medicine. Accessed March 2022.
Corneal cross-linking. American Academy of Ophthalmology. January 2022.
Page published on Wednesday, October 20, 2021






