Descemetocele and corneal perforation from corneal ulcers
What is a corneal descemetocele?
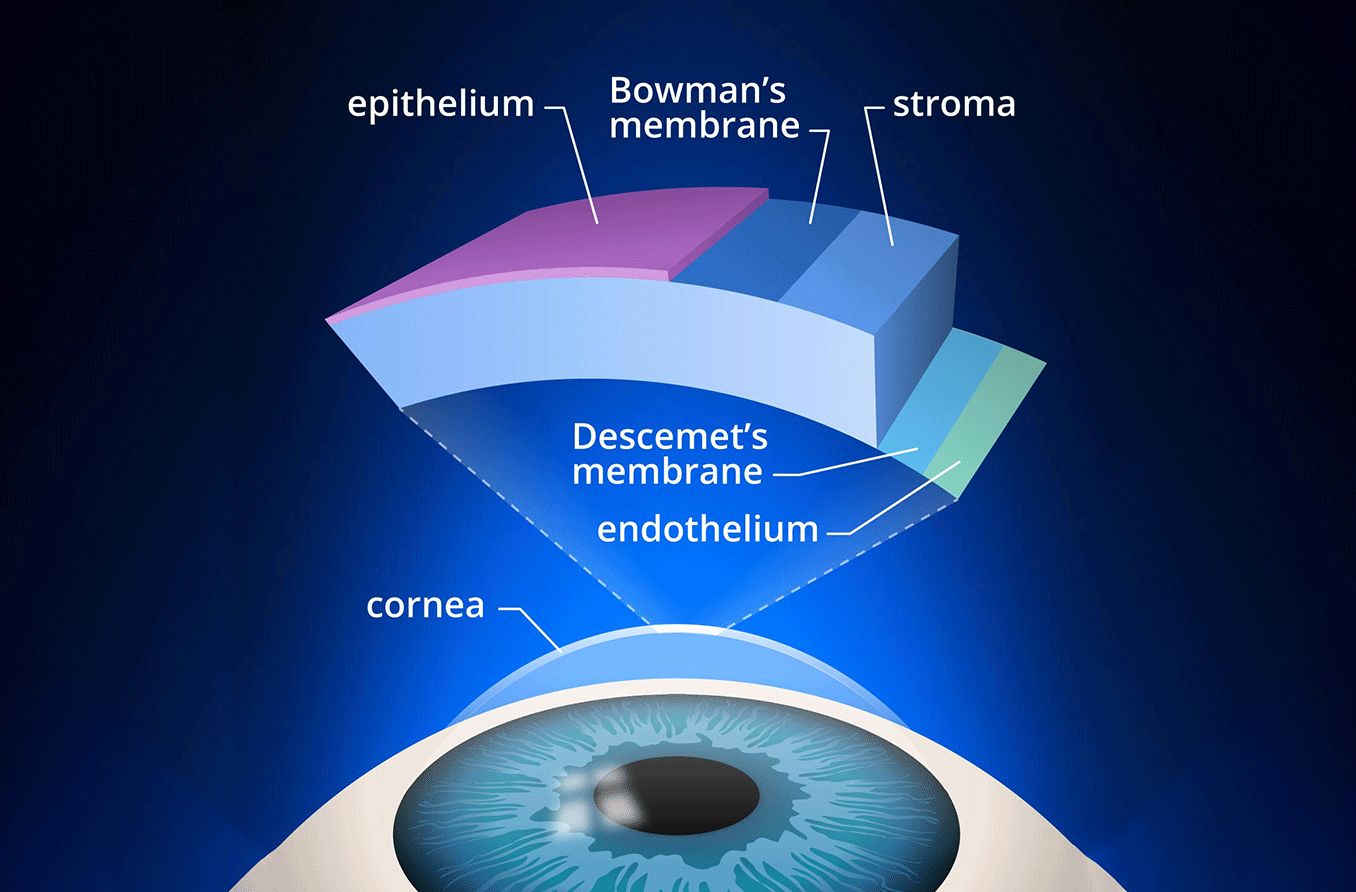
A corneal descemetocele is a condition in which the Descemet membrane, a layer of the cornea, protrudes through a thin area in the corneal layers above it. The cornea is made up of three main layers:
The epithelium on the surface of the eye
The stroma in the middle
The endothelium on the inside
The Descemet membrane anchors the endothelium to the stroma. The endothelium is also adjacent to the fluid that circulates inside the eye (the aqueous humor). Since this fluid is under pressure, it can press the endothelium and the Descemet membrane forward through a damaged cornea, just like an inner tube can bulge through a thin spot in a tire.
Corneal descemetoceles are rare but dangerous. They are usually caused by a corneal ulcer. If left untreated, they can cause the cornea to leak and the eye to lose pressure.
Corneal ulcers are considered a medical emergency. It is important to seek immediate care if you have any of the associated symptoms.
What causes a corneal descemetocele?
A descemetocele can develop from corneal ulcers that have been left untreated. Corneal ulcers are open sores that form on the cornea — the clear layer of tissue on the outside of the eye. These sores can cause the structure of the cornea to weaken.
When the Descemet membrane is the only layer of the cornea to remain intact, pressure from inside the eye may cause it to bulge out. This results in a corneal descemetocele.
Corneal ulcers can be caused by:
Infections of bacteria, viruses, fungi or parasites
Autoimmune diseases
Exposure of the eyeball
Trauma to the cornea, such as a corneal abrasion
People at risk for corneal ulcers include those who:
Have had cold sores, shingles or chickenpox
Have eyelids that do not close completely or are damaged
Have severe rheumatoid arthritis or lupus
Have had an injury or chemical burn to their cornea
Have a type of allergy called atopic disease
What are the symptoms of a corneal descemetocele?
Corneal descemetocele can lead to a sudden loss of visual clarity, depending on where the protrusion is located. It will also likely cause eye pain and watering. These may develop after symptoms associated with corneal ulcers.
Symptoms of a corneal descemetocele may include:
Photophobia (light sensitivity)
A white patch on the cornea
One common sign of a descemetocele is a white, cloudy ring circling the protrusion.
Because of the similarities in their appearance, corneal ulcers may be mistaken for conjunctivitis (pink eye).
How is a corneal descemetocele diagnosed?
To help diagnose a corneal ulcer and potential descemetocele, your eye doctor will likely perform a slit lamp examination. This exam involves the use of a microscope with a bright light, called a slit lamp. The microscope allows the doctor to examine the structure of the eye.
Your doctor may take a sample of the infected tissue for further examination. This will allow them to determine what kind of infection is present.
They may also perform a Seidel test, which will help them determine whether the cornea is perforated and actively leaking fluid. The Seidel test uses a dye called fluorescein, which highlights any fluid leaking out of the cornea.
How is a corneal descemetocele treated?
Your eye doctor will focus on two main things when treating descemetoceles: ocular integrity and the root cause of the corneal ulcer. Reinforcing the corneal structure is vital, as this will help prevent new holes (corneal perforations) from forming in the cornea.
Depending on the size of the descemetocele and the doctor’s experience, any of the following treatment options may be used:
Tissue adhesive – This glue-like substance helps hold tissue together. This is a helpful alternative to stitches.
Amniotic membrane transplantation – The inner layer of placenta can be used as a graft to help heal the surface of the eye.
Conjunctival flaps – This is a procedure in which a thin flap of conjunctiva is pulled over the area of the cornea that’s been impacted. The flap is then secured with sutures. The conjunctiva is a thin membrane that covers the white of the eye (the sclera).
Corneal transplantation – Also called keratoplasty, this is the use of a donor’s cornea to replace the patient’s affected cornea.
Conjunctival resectioning – This is the surgical removal of about 3 millimeters of conjunctiva near the ulcer.
The variety of conditions that lead to descemetoceles means that there are multiple treatment options. Other treatment options can include:
Antibiotics to treat infection
Lubricating eye drops to treat dry eye
Drops to reduce eye pressure
Bandage contact lens, a special type of contact used to help heal the cornea rather than improve visual acuity
Anti-collagenase medications and/or vitamin C to help treat corneal ulcers
Anti-inflammatory medications and/or immunosuppressants to help reduce inflammation
What risks are associated with a corneal descemetocele?
If a corneal descemetocele goes untreated, the protrusion (or hernia) may rupture or burst, leading to a corneal perforation. This means that a hole has formed through all layers of the cornea.
Other possible complications of a corneal descemetocele include:
A weakened anterior chamber – When the space containing clear fluid between the cornea and the iris is weakened
Endophthalmitis – An infection in the tissue or fluid of the eye
Glaucoma – An eye disease that causes damage to the optic nerve
Cataracts – Cloudiness of the eye’s natural lens
Major loss of vision
Loss of the affected eye
When should you see a doctor?
Remember: Corneal ulcers are considered a medical emergency. If you notice any of the signs or symptoms of a corneal ulcer or descemetocele, you should seek immediate medical attention.
Management of descemetocele and corneal perforation. EyeWiki. January 2022.
Descemetocele. Survey of Ophthalmology. December 2020.
Descemet's membrane development, structure, function and regeneration. Experimental Eye Research. August 2020.
The endothelium. Morgan & Claypool Life Sciences. 2011.
Corneal ulcer. Penn Medicine. August 2020.
Descemetocele. EyeRounds. February 2008.
Management of descemetocele: Our experience and a simplified treatment algorithm. Indian Journal of Ophthalmology. May 2022.
Aqueous humor flow and function. BrightFocus Foundation. January 2022.
Corneal ulcer. Cleveland Clinic. March 2022.
What is a slit lamp?. American Academy of Ophthalmology. April 2018.
Eye anatomy. ExeterEye. Accessed September 2022.
What is endophthalmitis? American Academy of Ophthalmology. August 2022.
Glaucoma. National Eye Institute. April 2022.
Cataracts. National Eye Institute. August 2022.
Ocular adhesives: Design, chemistry, crosslinking mechanisms, and applications. Biomaterials. January 2019.
Amniotic Membrane Transplant. EyeWiki. January 2022.
About corneal transplantation. American Academy of Ophthalmology. September 2021.
Anatomy, head and neck, eye conjunctiva. StatPearls. July 2021.
Page published on Tuesday, October 18, 2022
Medically reviewed on Wednesday, October 12, 2022






