Corneal erosion: Causes, symptoms and treatment

What are corneal erosions?
Corneal erosion occurs when the outermost corneal layer, the epithelium, does not adhere properly to the underlying layers. As a result, it can be torn off. This may happen as soon as the eyes are opened after sleeping, resulting in sudden onset of pain, blur, tearing and light sensitivity.
How does corneal erosion occur?
Corneal erosion occurs when the epithelium, the outer layer of the cornea’s five layers, does not adhere properly to its underlying layers. As a result it can shear off.
The cornea is the clear, dome-shaped outer layer of the eye. It provides a protective barrier that prevents particles, bacteria and viruses from entering. A corneal erosion is best understood by becoming familiar with the five layers of the cornea:
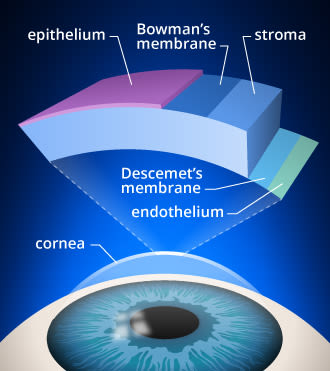
Layers of the cornea. Corneal cross-linking strengthens bonds in the stroma of the cornea, which is the layer from which tissue is removed during LASIK surgery.
Epithelium – Outermost, smooth layer of cells that absorb nutrients and oxygen from tears. It is rich in nerve endings, making it pain-sensitive. This is why corneal erosions are very painful. The epithelium is attached by protein fibers to an underlying basement membrane that anchors it to the rest of the corneal layers.
Bowman’s layer – Transparent protective layer under the epithelium. It is made of collagen and can scar as it heals.
Stroma – Middle layer that provides 90% of the cornea’s thickness. Made mostly of collagen and water, which give it structure and elasticity.
Descemet’s membrane – Protective layer of collagen fibers.
Endothelium – A single layer of cells that pump excess water out of the stroma.
Injury and disease can break down the protein fibers that bind the epithelium layer to its basement membrane. When this occurs, the risk of corneal erosion increases.
Corneal erosion often occurs upon waking. This is because there is decreased oxygen to the cornea when the eyelids are closed. As a result, the epithelial layer of the cornea can swell overnight and stick to the inside of the eyelid, shearing off when the eyes open. When the epithelium is suddenly torn away, intense pain and blurry vision result.
A corneal erosion is not only extremely painful, it also breaks down the cornea’s first line of defense. This leads to an increased risk of infection, inflammation and further injury.
SEE RELATED: Corneal deposits
What causes corneal erosion?
Corneal erosion can be caused by a number of underlying causes. But, the majority of corneal erosion cases are due to injury or a group of conditions called corneal dystrophies.
Corneal injury
Corneal injury is the most common underlying cause of corneal erosion. It is estimated that one-half to two-thirds of corneal erosion cases are due to trauma to the cornea.
Often the injury is from a tree branch, a paper cut or a finger that pokes the eye. A recurrence of corneal erosion is seen in 5% to 25% of cases of corneal injury.
Corneal dystrophy
Corneal dystrophies are a group of inherited corneal conditions that are slow-progressing. They result in progressive vision loss and other symptoms such as recurrent corneal erosions.
Corneal dystrophies are linked to about 20% to 30% of cases.
Additional causes
These conditions have also been found to increase the risk of corneal erosion:
Aggressive eye rubbing
Contact lenses that do not fit well or are poorly cared for
Diabetes mellitus
Corneal degeneration such as band keratopathy
What are symptoms of corneal erosion?
Corneal erosion can occur suddenly and cause mild to severe pain that can last from hours to several days. This is due to the high concentration of nerve receptors in the cornea. People often feel as if there is something in their eye.
Symptoms of corneal erosion include:
Usually, corneal erosions occur in one eye, but they can occur in both eyes in people with corneal dystrophies.
What is recurrent erosion syndrome?
When an individual repeatedly experiences corneal erosion, it is referred to as recurrent erosion syndrome. It is often seen in adults aged 30 to 80 years, the most common ages being between 30 and 40 years. Women are slightly more likely to experience corneal erosion.
Recurrent corneal erosions can create a weak area in which the epithelial layer no longer adheres firmly. As a result, even minor injuries can cause corneal erosion. In fact, recurrent erosion can occur many months or years later.
Recurrent erosion syndrome is often the result of an injury to the eye. But, it can also be due to corneal disease, in particular, corneal dystrophies. This group of conditions damages the layers of the cornea, making it more vulnerable to recurrent corneal erosions.
Epithelial basement membrane dystrophy (EBMD) is a corneal condition that can increase the risk of corneal erosion. It is the underlying cause of about one-fifth to one-third of recurrent corneal erosions. This condition causes an abnormal folding of the epithelium. It is also known as “map-dot-fingerprint dystrophy” because of its appearance.
Additional dystrophies that also increase the risk of recurrent erosion syndrome are:
Reis- Buckler dystrophy – This dystrophy causes blurry vision or double vision in one eye due to scarring and clouding of Bowman’s membrane. By 20 years of age, decreased vision and foreign body sensation are common. It is also known as granular corneal dystrophy type III.
Macular dystrophy – This dystrophy begins to cloud the cornea after age 3 and during the first decade. Eye irritation along with visual acuity loss are early symptoms. By age 20 or 30, vision loss may be severe.
Lattice dystrophy – This dystrophy causes the cornea to become cloudy, decreasing vision. It is due to abnormal overlapping protein fibers in the stroma (giving the appearance of a lattice).
Granular dystrophy – This dystrophy is due to deposits of abnormal material in the stroma. It causes clouding of the cornea during the first decade. By age 20 or 30, vision loss may be severe.
Fuchs endothelial corneal dystrophy – This is the most common dystrophy. It causes progressive damage to the endothelium, which is responsible for pumping fluid out of the stroma, preventing swelling and corneal clouding. Eventually, Fuchs’ dystrophy may require corneal transplant surgery or a procedure that transplants healthy endothelial cells on the cornea.
SEE RELATED: Corneal disease: A guide to conditions and treatments
How do you treat corneal erosion?
Treatment of corneal erosion is dependent on the underlying cause. An eye doctor that suspects corneal erosion will ask whether you have had an injury to the cornea in the past. The doctor will also look for signs of underlying eye conditions that increase the risk of corneal erosion.
When an eye doctor sees a patient with corneal erosion, they may place a numbing drop to temporarily relieve the pain so that they can take a closer look at the eye. An eye drop with dye may also be used to detect the erosion. Once they complete a full evaluation, an eye doctor, may prescribe:
Antibiotic drops to ensure that the eye does not develop an infection
Oral or topical pain medication
Dilating drops to control pain
Debridement, which creates a uniform surface to speed up healing and decrease pain
Bandage contact lens that provides comfort and helps the healing process
Preservative-free lubricating drops
Eye patch to prevent further injury
In order to decrease the risk of future corneal erosions, an eye doctor may prescribe some preventive therapies:
Overnight ointments
Solutions that decrease swelling of the cornea (such as sodium chloride 5%)
Punctal plugs to treat dry eye syndrome
In cases of severe recurrent corneal erosion, surgical treatment may be necessary. This includes:
Superficial keratectomy – a laser treatment that removes central epithelium to create a uniform surface
Anterior stromal puncture – a treatment that helps to bind together the layers of the cornea
Diamond Burr Polishing – a laser treatment that removes the central epithelium and then ablates the cornea to create a uniform surface
In addition to receiving proper treatment for corneal erosion, it is important not to rub your eyes. Eye rubbing can cause the condition to worsen.
If you have contact lenses, follow your eye doctor’s guidance on when you can resume routine contact lens wear.
Can you go blind from recurrent corneal erosion?
Recurrent corneal erosion does not typically lead to blindness. In fact, it has an excellent prognosis. It is important to see an eye doctor if you notice symptoms that indicate you may be experiencing recurrent corneal erosion.
Although the epithelial layer of the cornea heals fairly quickly, the detached epithelial layer in a corneal erosion may take a long time to firmly bind to the basement layer again. Early diagnosis and proper treatment can decrease the risk of recurrent corneal erosion and long-term complications. Routine exams with your eye doctor play an important role in the management of recurrent corneal erosion.
READ NEXT: What Is a corneal descemetocele?
Corneal abrasion and erosion. American Academy of Ophthalmology. September 2021.
Recurrent corneal erosion: a comprehensive review. Clinical Ophthalmology. February 2019.
Anatomy of cornea and ocular surface. Indian Journal of Ophthalmology. February 2018.
Recurrent corneal erosion. “Cornea” in Kanski’s Clinical Ophthalmology. 2020.
Recurrent corneal erosions. Canadian Association of Optometrists. Accessed April 2022.
The OD’s guide to managing recurrent corneal erosion. Review of Optometry. January 2017.
What are corneal dystrophies? American Academy of Ophthalmology. EyeWiki. January 2022.
Corneal erosions or abrasions (scratched dye). Kellogg Eye Center Michigan Medicine. Accessed April 2022.
Recurrent corneal erosion. American Academy of Ophthalmology. EyeWiki. January 2022.
Corneal dystrophies. National Organization for Rare Disorders. Accessed April 2022.
Two cases of Reis-Bücklers corneal dystrophy (granular corneal dystrophy type III) caused by spontaneous mutations in the TGFBI gene. Journal of the American Medical Association. April 2006.
Corneal stromal dystrophies. American Academy of Ophthalmology. EyeWiki. October 2021.
What is Fuchs’ dystrophy? American Academy of Ophthalmology. EyeWiki. September 2021.
Pathogenesis, clinical features and management of recurrent corneal erosions. Eye. July 2005.
Page published on Wednesday, June 8, 2022






