Corneal infiltrates: Causes, treatment and more
What are corneal infiltrates?
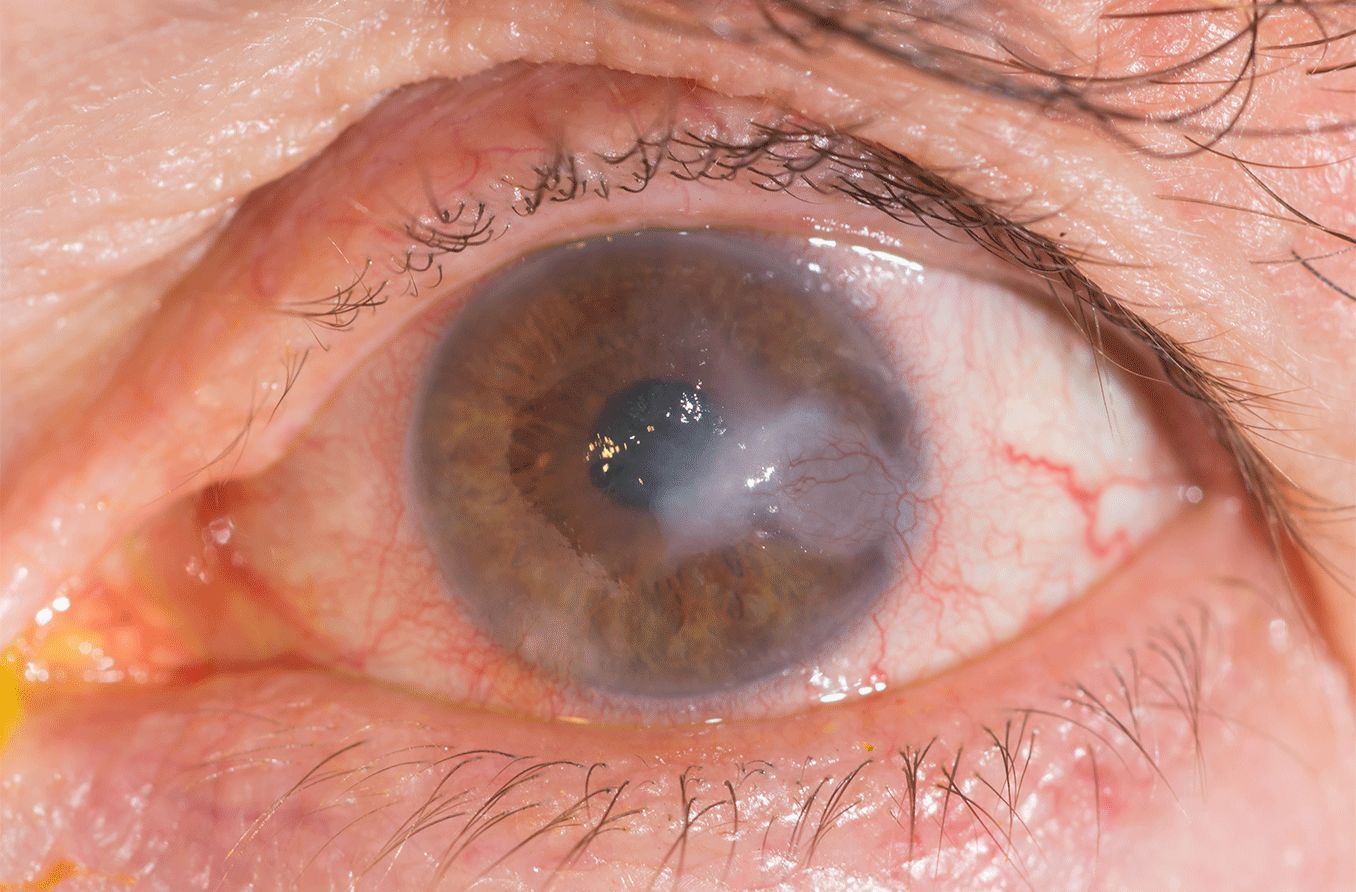
A corneal infiltrate is a single or group of inflammatory cells in the normally clear cornea. An infiltrate results from an infection, decreased oxygen supply or injury to the cornea. A corneal infiltrate is visible under high magnification as round, gray spots surrounded by areas of swelling.
Causes of corneal infiltrates
Since corneal infiltrates represent your body’s response to an infection or inflammation, there are many reasons they can form. Everything from an eye infection to wearing contact lenses for long periods of time can lead to the formation of corneal infiltrates. Some people who undergo corneal surgery can also develop corneal infiltrates.
There are two main types of corneal infiltrates: infectious and sterile. Infections in the cornea can be caused by bacteria, viruses or other agents. Corneal infiltrates that have a sterile cause are not due to infections. But they may be caused by contact lens overwear or surgery.
To determine the type and cause of corneal infiltrate you have, your eye care provider will examine your eye and take a thorough patient history.
Causes of infectious corneal infiltrates
Infectious corneal infiltrates are the most common types of corneal infiltrates. They are also often more painful than their sterile counterparts. They can lead to mucus discharge, tearing, hypopyon formation and even ulceration if left untreated.
Infectious infiltrates are, in general, more common in the central cornea. Common causes include:
Viruses – Viruses can lead to the formation of corneal infiltrates. Viruses include herpes simplex, herpes zoster and the adenoviruses that cause epidemic keratoconjunctivitis.
Bacterial keratitis – This type of corneal infection is usually due to Staphylococcus, Streptococcus and Pseudomonas bacteria. About 20-40% of bacterial keratitis cases are caused by bacteria that form in contact lenses and their cases. Your contact lenses offer an environment that’s ripe for bacterial growth and transmission. When these bacteria come in contact with your eye, they can lead to an infection that can cause corneal infiltrates to form. People who wear extended-wear contact lenses have an over 40% risk of developing bacterial keratitis.
Fungal keratitis – This type of inflammation is less common than bacterial keratitis. Fungal keratitis can occur after an injury to the eye from certain types of plants or vegetables. It may develop in immunocompromised individuals if their eyes are exposed to the fungus. Contact lens-related fungal keratitis is much less common but can also occur.
Protozoan infections – These infections are usually caused by a parasite. People who wear contact lenses in a pool, freshwater or hot tub are at higher risk. They can lead to severe pain and photophobia if left untreated.
Causes of non-infectious (sterile) corneal infiltrates
Sterile corneal infiltrates rarely lead to mucus discharge. They also tend to be less painful and don’t lead to sensitivity to light like infectious corneal infiltrates. They are, in general, more common in the peripheral cornea.
Contact lenses
By far the most common cause of sterile corneal infiltrates is wearing contact lenses. Wearing contacts can lead to the formation of infectious corneal infiltrates. This occurs when there is a transfer of bacteria. They can also lead to the formation of sterile corneal infiltrates.
Contact lens issues can result in corneal infiltrates. Issues include improper fit or material, sensitivity to solutions and infrequent lens replacement. A poor care routine and insufficient oxygen to the cornea due to overnight wear can also cause corneal infiltrates.
Staphylococcal blepharitis
This condition is typically caused by an overgrowth of a bacteria, Staphylococcus aureus. This bacteria can live on your body without making you sick. The bacteria can cause an inflammatory reaction in the cornea rather than an infection. This inflammation can lead to sterile infiltrates in the cornea.
Vernal keratoconjunctivitis
This condition is a chronic and seasonal form of severe eye allergies that can lead to sterile infiltrates. It is typically found in warmer dry climates and affects young males. [Read more about vernal conjunctivitis.]
Medical conditions
Auto-immune diseases can cause corneal infiltrates due to inflammation. Examples include rheumatoid arthritis, multiple sclerosis and lupus.
Corneal surgery
Refractive surgery such as PRK and LASIK cause trauma and inflammation in the eyes. Corneal infiltrates are thought to occur in about 1 in 300 cases. They are likely related to the use of bandage contact lenses.
Signs and symptoms of corneal infiltrates
Corneal infiltrates that are sterile tend to be smaller and more peripheral in the cornea. Infiltrates caused by infections are often found in the central cornea and are larger. These can turn into corneal ulcers if they are not promptly treated by an eye doctor.
Since corneal infiltrates occur due to a number of different causes, they can be accompanied by a variety of symptoms.
Corneal infiltrates due to infection are commonly seen with the following symptoms:
Painful eye
Discharge (type will vary depending on the cause of the infection)
Sensitivity to light
Red eyes
Corneal infiltrates with a sterile origin are commonly seen with the following symptoms:
Mild pain and irritation
Clear vision
Minimal discharge
Mild sensitivity to light
Slight red eye
How to treat corneal infiltrates
The type of treatment you receive for a corneal infiltrate will have to do with whether it’s infectious or sterile.
If your corneal infiltrate was caused by wearing contact lenses, your eye doctor may suggest wearing them less frequently. They may also recommend switching to a different brand.
Ocular steroids have proven to be especially effective in treating sterile corneal infiltrates. They do this by shortening the duration of the inflammation. These steroids are often prescribed along with antibiotics. This helps to decrease the chances of developing a secondary infection.
If your corneal infiltrate was caused by an infection, topical antibiotics, antivirals or antifungals may be prescribed. Corticosteroids may be used to decrease inflammation, discomfort or potential corneal scarring.
If you’re not experiencing pain or discomfort, it’s possible that your eye doctor may decide on no treatment. This is because many types of corneal infiltrate disappear on their own within two weeks.
When to see a doctor
If you’re experiencing pain, cloudy vision or increased sensitivity to light in one or both eyes, contact your eye doctor right away.
A comprehensive eye exam and a medical history will help the eye doctor determine the cause of your eye condition. If corneal infiltrates are present, they will determine which type of corneal infiltrate you have (sterile or infectious). Then they will develop a treatment plan if needed.
Characterizing contact lens — related corneal infiltrates: A pilot study. Journal of Cornea and External Disease. December 2016.
Intruder alert: Diagnosing corneal infiltrative disease. Review of Optometry. January 2018.
Risk factors for corneal infiltrative events during continuous wear of silicone hydrogel contact lenses. Investigative Ophthalmology & Visual Science. November 2010.
Peripheral corneal infiltrate. Columbia University Ophthalmology. Accessed October 2022.
On the spot. Review of Optometry. January 2020.
Marginal infiltrates: A mysterious malady. Review of Ophthalmology. January 2005.
Patient history key for treating corneal infiltrates. Healio Ophthalmology. January 2021.
Page published on Thursday, October 13, 2022
Page updated on Thursday, October 13, 2022






