A guide to causes and treatment of corneal neovascularization
What is vascularization of the cornea?
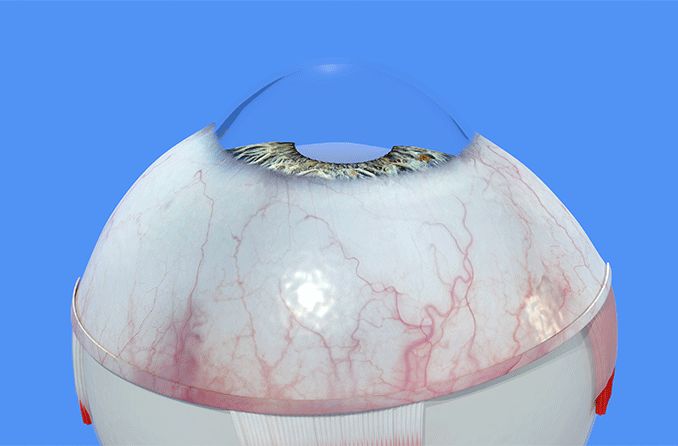
The cornea is the only part of the body that is not vascular (does not have blood vessels), providing a clear path for light to enter. However, reduced oxygen, inflammation, infection or trauma can cause formation of blood vessels in the cornea, which may lead to sight-threatening complications.
Growth of blood vessels in the cornea (corneal vascularization) may lead to permanent vision impairment. This sight-threatening condition affects 1.4 million people each year. One study reported that about 1 in 10 people affected by corneal neovascularization suffer loss of vision.
Why does the cornea need to be avascular?
Corneal neovascularization [Image credit: Permission granted by © 2022 American Academy of Ophthalmology]
Avascular means “without blood vessels.” The cornea receives oxygen that is diffused through the tears, rather than from blood vessels. This allows light rays to enter the eye without obstruction.
This is critical because the cornea provides most of the focusing power of the eye. It does this by bending light rays as they enter the eye so that they are focused on the retina to provide a sharp, clear image.
Vascularization of the cornea can damage the clear corneal tissue, leading to clouding or haziness of vision. Blood vessels can block and bend light entering the eyes and decrease visual acuity.
What are the main symptoms of corneal neovascularization?
Corneal neovascularization does not always have apparent symptoms, especially when it is mild or in early stages. A contact lens wearer might find that their lenses are causing slight discomfort. They may also notice hazy vision or decreased visual acuity.
Blood vessels that have grown into the cornea are usually more fragile and delicate than normal blood vessels. Due to this, they rupture more easily and can cause bleeding — resulting in decreased vision, or even corneal scarring.
An eye doctor will be able to detect corneal neovascularization by looking at the cornea under high magnification.
Where in the eye does corneal neovascularization occur?
In addition to bending light rays as they enter the eye, the cornea also serves as a protective barrier. The cornea has five layers that provide structure and prevent germs and particles from entering the eye.
The five layers of the cornea are:
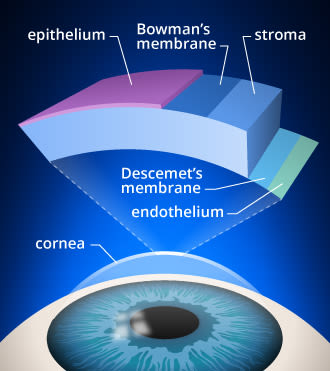
Layers of the cornea. Corneal cross-linking strengthens bonds in the stroma of the cornea, which is the layer from which tissue is removed during LASIK surgery.
Epithelium – Smooth outer layer. It serves as a barrier and absorbs nutrients and oxygen from tears. It heals rapidly but is rich in nerve endings, making it very pain-sensitive.
Bowman’s layer – Transparent protective layer made of collagen. It can scar as it heals.
Stroma – Middle layer made of water and collagen. It provides 90% of the cornea’s thickness and gives it structure and elasticity. In order to maintain clear vision, the stroma must remain transparent.
Descemet’s membrane – Protective layer of collagen fibers. This membrane recovers well from injury.
Endothelium – A single layer of cells that pump excess water out of the stroma. It keeps the stroma from absorbing too much (which would cause corneal edema and haziness).
Decreased oxygen levels, inflammation, infection or trauma can stimulate abnormal blood vessels to grow in the cornea. Corneal neovascularization (CNV) can occur in different layers of the cornea depending on the underlying cause and severity.
Blood vessel growth begins at the limbus, the border between the clear cornea and white sclera. It then progresses toward the center of the cornea. The growth may extend into the superficial layers of the cornea such as the epithelium. It may also extend into deeper layers, like the stroma, resulting in decreased visual acuity.
Three types of neovascularization are typically seen:
Superficial neovascularization – growth of blood vessels between epithelium and Bowman’s layer, also known as corneal pannus
Stromal neovascularization – growth of blood vessels in the stroma
Deep neovascularization – growth of blood vessels between stroma and Descemet's membrane
What causes corneal neovascularization?
There are five primary causes of corneal neovascularization. These include:
Contact lens wear
Corneal neovascularization is relatively common in soft contact lens wearers. Contact lenses can cause irritation to the cornea and reduce the amount of oxygen that reaches it. It is estimated that about 10% to 30% of corneal neovascularization cases are associated with contact lens wear.
Soft contact lenses are larger and cover more of the cornea. Due to this, they are a more common cause of CNV than rigid contact lenses, which tend to be smaller and cover less of the cornea.
Neovascularization from contact lenses is typically only found in the superficial layers of the cornea, such as the epithelium. The concern is that the blood vessels will grow deeper into the stromal layer of the cornea, although this is rare. Sleeping in contact lenses increases the risk of corneal neovascularization.
Causes of neovascularization from contact lens wear include:
Tight or decentered soft contact lenses that restrict oxygen delivery to the cornea
Damaged lens or lens with heavy deposits that cause injury to the corneal epithelium
Sensitivity to contact lens solutions
Contact lens overwear – wearing lenses for longer durations than recommended
Management depends on the cause and severity of blood vessel ingrowth and includes:
Contact lens refitting
Switching to higher water content contact lenses
Switching to lenses with higher oxygen permeability
Switching from extended wear contact lenses to daily wear
Discontinuation of contact lens wear
Use of preservative-free lens care products
Inflammation
Corneal neovascularization may be caused by inflammation due to a number of conditions.
Inflammatory conditions that may cause corneal neovascularization include:
Superior limbic keratoconjunctivitis
Atopic conjunctivitis
Graft versus host disease
Ocular pemphigoid
Trauma
Trauma can be the result of a mechanical injury to the cornea. Thermal or acidic burns may cause superficial corneal neovascularization (in the area of the epithelial layer). Corneal trauma can also be due to alkali burns — which can permeate the stroma and cause neovascularization.
Corneal infections
Neovascularization can occur even one day after corneal infection with herpes simplex virus (HSV). The vascularization can continue for two to three weeks after infection.
There are a number of corneal infections that can lead to neovascularization. These include:
Viral – Herpes simplex, herpes zoster
Bacterial – Chlamydia, Syphilis, Pseudomonas
Fungal – Candida, Aspergillus, Fusarium
Parasitic infections
Corneal degeneration
Corneal degeneration refers to deterioration of the corneal tissue that results from one of a number of corneal diseases. Corneal degeneration often occurs only in one eye and begins on the edges of the cornea. Degenerations may result in corneal deposits, thinning or neovascularization.
READ MORE: Corneal disease: A guide to conditions and treatments
Can corneal neovascularization be treated?
Management is often specific to the cause and severity of the neovascularization. Vascularization due to contact lens wear is typically managed by strategies that improve the fit of the contact lens and the amount of oxygen available to the cornea. Underlying corneal conditions will need to be addressed.
Treatments
Typical medical treatment may include steroid drops applied directly to the eye. This can be done in addition to the anti-VEGF medication bevacizumab, which aims to prevent new blood vessel formation. However, these treatments have a number of side effects. Steroid drops can increase risk of glaucoma and increase vulnerability to infections. Anti-VEGF treatment may inhibit wound healing and nerve regeneration.
In some cases, medical therapy is not effective. Laser and surgical procedures are often the next step in treating corneal neovascularization. Surgical options include:
Laser ablation
Cautery
There are cases of neovascularization in which medical or surgical treatments prove unsuccessful. Corneal transplantation is currently the only treatment that yields consistently successful results.
Treatments in development
Treatment of corneal neovascularization is an area of active research. Some therapies in development are topical PEDF therapy, PDGF receptor inhibitors and topical aganirsen.
Routine eye exams
Corneal neovascularization is commonly caused by contact lens wear. It can also be caused by inflammation or an underlying ocular condition. A comprehensive eye exam is important in maintaining healthy eyes. Routine exams will help to ensure your eye doctor is able to monitor your eyes for the development of abnormal blood vessels in your cornea.
Eye exams are especially important if you wear contact lenses. They are also critical if you have an underlying eye condition that is associated with corneal neovascularization.
READ MORE: Corneal dystrophy: Conditions and symptoms
Corneal neovascularization: updates on pathophysiology, investigations & management. Romanian Journal of Ophthalmology. January 2019.
Anatomy of cornea and ocular surface. Indian Journal of Ophthalmology. February 2018.
Corneal neovascularization. EyeWiki. American Academy of Ophthalmology. March 2022.
Clinical correlates of common corneal neovascular diseases: A literature review. International Journal of Ophthalmology. November 2014.
Contact lens-induced neovascularization. Contact Lens Spectrum. April 1996.
Corneal neovascularization. Kellogg Eye Center University of Michigan. March 2015.
Corneal neovascularization. Columbia Ophthalmology. Accessed February 2022.
Handling contact lens complications. Review of Ophthalmology. September 2004.
Pathogenesis of herpes stromal keratitis – A focus on corneal neovascularization. Progress in Retinal and Eye Research. March 2013.
Clinical causes of CNV. National Center for Biotechnology Information. Accessed February 2022.
Treatment of corneal neovascularization. American Academy of Ophthalmology. October 2013.
Therapeutic approaches for corneal neovascularization. Eye and Vision. December 2017.
Page published on Thursday, April 7, 2022






