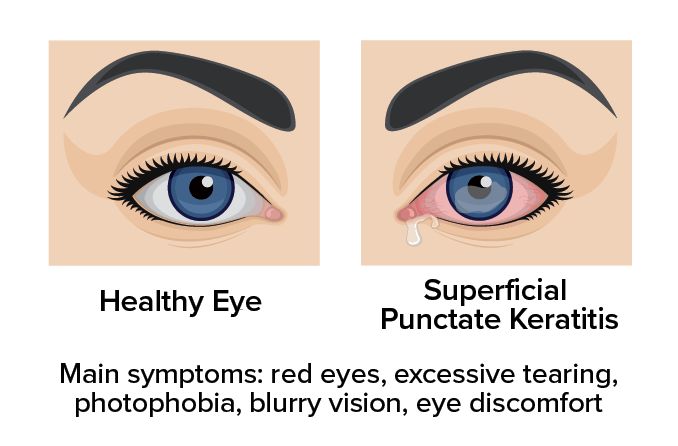
Superficial punctate keratitis: Symptoms, causes and treatment
What is superficial punctate keratitis?
Superficial punctate keratitis (SPK) is damage to the cells of the cornea’s outer layer. SPK can be visualized by staining the eye with a dye and looking under high magnification and a bright light. It is caused by many conditions and results in discomfort, redness and watery eyes.
What are the symptoms of superficial punctate keratitis?
A variety of conditions can cause superficial punctate keratitis. As a result, symptoms of SPK vary somewhat depending on the underlying cause.
The development of superficial punctate keratitis can lead to symptoms that include:
Punctate keratitis [Image credit: Permission granted by © 2022 American Academy of Ophthalmology]
Eye discomfort
A sensation of something in the eye
Slightly blurry vision
What causes superficial punctate keratitis?
Infection, inflammation or injury are common causes of superficial punctate keratitis.
During an eye exam, an eye doctor will place a dye such as fluorescein or a Rose Bengal stain on the cornea. This will allow them to see SPK, which will stain as tiny dots or coalesced areas on the damaged corneal surface. They use an instrument called a slit lamp to look at the cornea under high magnification and bright light.
The location and size of SPK vary depending on the underlying condition. The SPK will be graded depending on the severity. It is typically graded on a 0 to 4 corneal staining scale, with 4 being the most severe.
An eye doctor will consider an individual’s symptoms, eye exam findings and medical history when diagnosing the cause of SPK. Common causes of superficial punctate keratitis include:
Dry eye syndrome
When someone has dry eye syndrome, their tear film is not stable, leading to an unhealthy and damaged cornea. SPK is one of the most common findings in someone with dry eye syndrome.
Symptoms of dry eye include a burning sensation, a feeling that something is in the eye, blurry vision, and watery or red eyes.
Blepharitis
Inflammation of the eyelids is called blepharitis. It is caused by bacteria (usually Staphylococcus aureus) on the skin or clogged oil-producing glands in the eyelid.
This inflammation can lead to an abnormal tear film and damage the cornea’s outer layer. Symptoms are similar to dry eye but include itchy eyes, crusting and swollen eyelids.
Viral infection
A common viral infection of the eye is called epidemic keratoconjunctivitis (EKC), also known as “pink eye.” It is very contagious and caused by the same group of viruses responsible for the common cold.
This, and other viral infections, disrupt the cornea and lead to the development of SPK. In addition to redness, symptoms include light sensitivity, irritation, tearing and watery discharge.
Bacterial infection
A bacterial infection can injure the cornea and result in SPK. In some cases, the eyes may be sensitive to normal bacterial byproducts and respond with inflammation, damaging the cornea.
Bacterial keratitis is commonly caused by Staphylococcus aureus. And it is typically seen in blepharitis. It is also commonly caused by Pseudomonas aeruginosa and is usually contact lens related. Symptoms include pain, thick discharge, redness, blur, light sensitivity and tearing.
Allergic reaction eye drops or solutions
Preservatives found in eye drops and contact lens solutions can cause an allergic reaction in some people. Thiomersal is one such preservative that some people are sensitive to.
An allergy to an eye drop/solution ingredient can cause the surface layer of the cornea to break down and develop SPK. Common symptoms of an allergic reaction are burning, itching and tearing.
Contact lens issues
Contact lenses that do not fit properly, specifically if the lens is too tight, can damage the corneal surface. Proteins deposited on the contact lens over time can also lead to SPK development.
Other contact lens issues that can lead to the development of SPK are overwear, drying of the contact lens and decreased oxygen to the cornea.
Recurrent corneal erosion
Recurrent corneal erosion is the result of the cornea’s outer layer separating from the rest of the cornea. It typically occurs overnight and upon opening the eyes in the morning.
Injury or certain diseases can result in the development of this painful condition. The repeated erosions cause superficial punctate keratitis.
Chemical burn to the eye
Acid or alkali splashed into the eye is a medical emergency and requires immediate treatment. Severe damage to the eye’s surface can occur, leading to vision loss. Alkali agents penetrate the eye’s tissues more quickly than acids.
Severe SPK can immediately develop from chemical burns to the cornea. A chemical injury is a true eye emergency, and medical care should be sought immediately.
UV light exposure
UV light exposure is also called photokeratitis or ultraviolet keratitis. This painful condition results from unprotected or prolonged exposure to UV radiation.
Similar to sunburn on the skin, UV radiation can damage the cornea’s surface layer, resulting in SPK in both eyes. Pain and blurry vision typically develop within six to 12 hours of exposure.
Incomplete lid closure
Lagophthalmos is when the eyelids do not close properly. Improper lid closure can cause the cornea to become exposed and damaged. This typically leads to the development of SPK on the lower cornea where the exposure occurs. Discomfort, irritation and red eyes are common symptoms.
Irritation from eyelashes
Eyelashes can become misdirected and ingrown and rub against the cornea. This is known as trichiasis and can occur due to eyelid inflammation or another condition. The repeated mechanical injury causes SPK and can worsen over time, eventually leading to abrasions or ulcers.
READ MORE: 15 keratopathies: Causes, symptoms and treatment
What is Thygeson superficial punctate keratitis?
Thygeson superficial punctate keratitis (TSPK) is a rare disease named after Phillips Thygeson. He first described the condition in 1950. It is a chronic condition that causes the development of SPK and round-shaped gray spots in the corneas of both eyes.
The disease develops slowly and does not present with many early symptoms. It is seen mainly in individuals in their 20s and 30s and has a higher incidence in females. The underlying cause of TSPK remains unknown.
What are the types of keratitis?
Keratitis is inflammation of the cornea. When a patient has symptoms associated with SPK, an eye doctor will stain the cornea with a dye and look under high magnification with a slit lamp.
The exam may reveal the following types of keratitis:
Superficial punctate keratitis (SPK) – tiny, scattered points of damage to the cornea’s outer surface layer (epithelium).
Punctate epithelial keratitis (PEK) – small spots of damaged tissue that are located within the epithelium.
Punctate epithelial erosions (PEE) – small areas of missing epithelium.
Subepithelial infiltrates (SEI) – small spots that are located underneath the epithelium.
How is superficial punctate keratitis treated?
The treatment of SPK varies depending on what caused it. An eye doctor will determine the underlying cause based on clinical findings, symptoms, and medical history.
Once a diagnosis is made, the doctor will prescribe the appropriate course of treatment. Most cases of SPK recover fully with treatment of the underlying condition.
Dry eye syndrome. Dry eye syndrome is usually treated with artificial tears and ointment at night. For more severe cases, an eye doctor may recommend prescription eye drops such as cyclosporine or lifitegrast that increase tear production. Punctal plugs that help to keep tears on your eyes may also be recommended.
Blepharitis. Blepharitis is often treated with warm compresses and lid scrubs. Artificial tears and antibiotics may also be recommended.
Viral infections. Viral infections such as EKC usually clear up without treatment. Artificial tears can provide relief from some symptoms.
Bacterial infections. Bacterial infections are treated with antibiotic drops or treatments. It is important to finish the full course of treatment to prevent the infection from recurring.
Allergic reactions and inflammatory conditions. These conditions are treated by removing the agent that is causing the allergy. Antihistamines and other eye drops that treat allergies may be prescribed. In severe cases, a short course of corticosteroid drops may be needed to treat a severe reaction.
Contact lens-related SPK. This is usually treated by discontinuing contact lens wear and treatment with artificial tears, or steroid and antibiotic drops. Once the SPK has healed, the individual can be refit for contact lenses.
Recurrent corneal erosion. Recurrent corneal erosion treatment is often case-by-case. Artificial tears and ointments are the most common treatments. Antibiotics, pain relievers or bandage contact lenses may be prescribed as well.
Chemical burns. A chemical burn should be flushed promptly with water for at least 20 minutes and treated as a medical emergency.
UV light exposure-related SPK. UV keratitis is treated with artificial tears, ointment and oral pain medication. The cornea will commonly heal within one to three days.
Incomplete lid closure and irritation from eyelashes. This will require treatment to resolve the underlying condition. In addition, artificial tears and ointment at night are recommended to help heal the damaged cornea.
SEE RELATED: Neurotrophic keratitis
When should I see a doctor?
The American Optometric Association recommends that adults have an eye exam at least every two years. People over 65 should have their eyes examined yearly because they are at higher risk for certain eye diseases.
If you have superficial punctate keratitis symptoms such as discomfort, redness, light sensitivity or blurry vision, you should contact an eye doctor. A comprehensive eye exam is required to determine the cause of these eye symptoms.
Cornea: Guide your way through SPK. Optometric Management. December 2018.
Superficial punctate keratitis: a diagnostic dilemma. Oman Journal of Ophthalmology. February 2021.
Superficial punctate keratitis. Merck Manuals Professional Edition. August 2022.
Automated grading system for evaluation of superficial punctate keratitis associated with dry eye. Investigative Ophthalmology and Visual Science. April 2015.
When dry eye compromises corneal integrity. Review of Optometry. November 2017.
Blepharitis: blink and you’ll miss it. Ophthalmology Management. December 2008.
What Is blepharitis? American Academy of Ophthalmology. August 2022.
Epidemic keratoconjunctivitis. EyeWiki. American Academy of Ophthalmology. May 2022.
A closer look at corneal inflammation. Review of Cornea and Contact Lenses. November 2012.
Contact lens-related microbial keratitis: How have epidemiology and genetics helped us with pathogenesis and prophylaxis? Eye. December 2011.
Basics of bacterial keratitis. Centers for Disease Control and Prevention. February 2022.
Review paper adverse events in allergy sufferers wearing contact lenses. Advances in Dermatology and Allergology. June 2015.
Recurrent corneal erosions. Wills Eye Hospital. Accessed August 2022.
Chemical (alkali and acid) injury of the conjunctiva and cornea. EyeWiki. American Academy of Ophthalmology. January 2022.
Corneal subbasal nerve recovery in an acute case of ultraviolet keratitis treated with autologous serum eye drops. Journal of Ophthalmology. February 2018.
Trichiasis. EyeWiki. American Academy of Ophthalmology. June 2022.
Thygeson superficial punctate keratitis. EyeWiki. American Academy of Ophthalmology. January 2022.
Dry eye. National Eye Institute. April 2022.
Conjunctivitis (pink eye). American Optometric Association. Accessed August 2022.
Allergic conjunctivitis. Journal of the American Association for Pediatric Ophthalmology and Strabismus. April 2020.
Managing-contact-lens associated-red-eye. Review of Cornea and Contact Lenses. December 2021.
Treatment of recurrent corneal erosions. EyeNet Magazine. American Academy of Ophthalmology. March 2013.
Photokeratitis. EyeWiki. American Academy of Ophthalmology. February 2022.
Comprehensive eye exams. American Optometric Association. Accessed August 2022.
Page published on Tuesday, August 30, 2022






