Diabetic macular edema (DME)
What is diabetic macular edema?
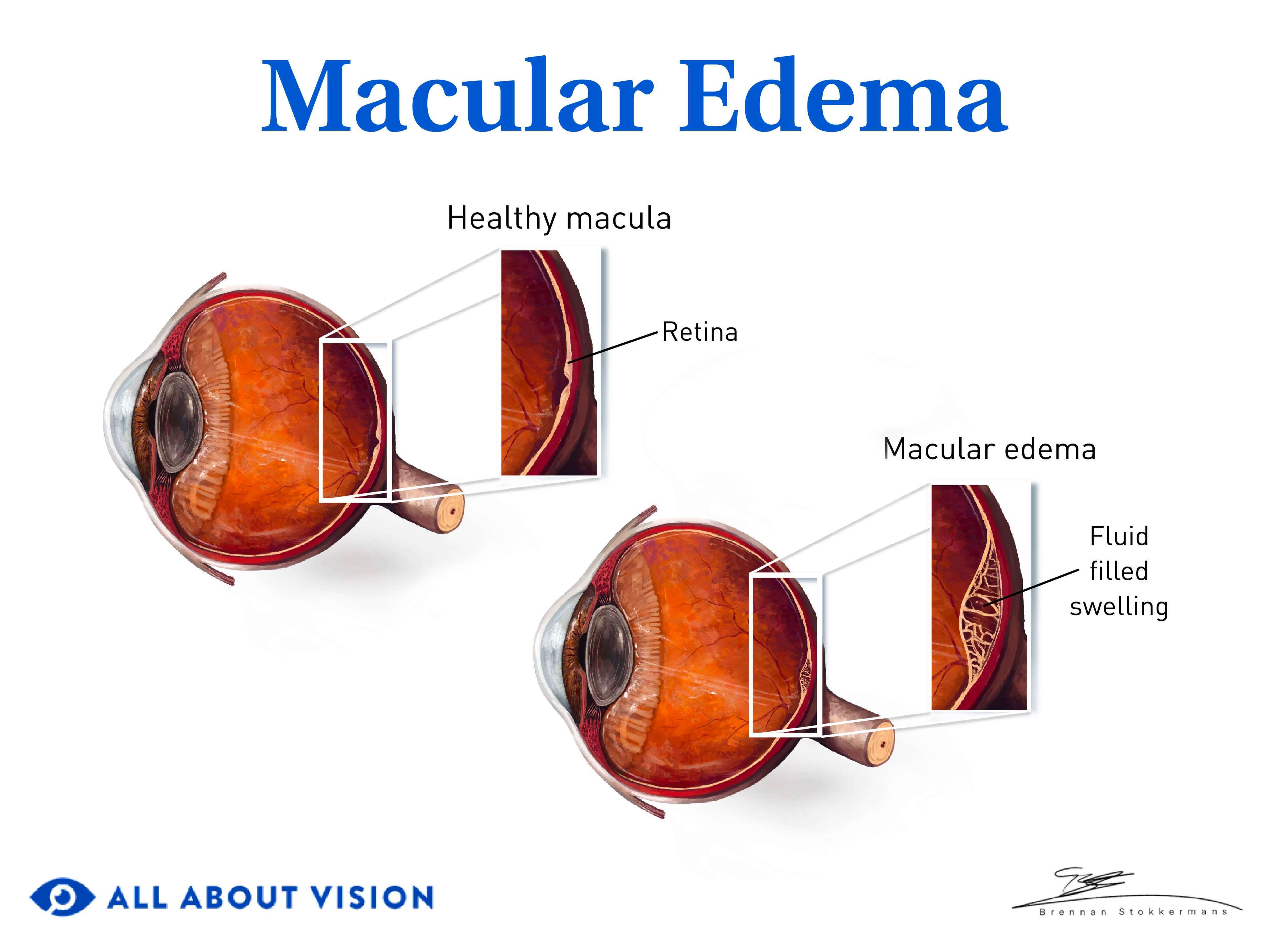
Diabetic macular edema (DME) is an eye condition that develops when excess fluid builds up in the macula, causing it to swell. This swelling may cause blurred vision and other effects that impact visual acuity. Diabetic macular edema is the primary cause of vision loss in people with diabetes.
The macula is in the center of the retina (the light-sensing membrane in the back of the eye). It is responsible for sharp central vision, which allows you to see objects in fine detail.
Macular edema is defined as fluid accumulation in the macula that causes it to thicken or swell. It may be caused by various factors, from hypertension to other eye diseases. The definition of diabetic macular edema, also spelled diabetic macular oedema, is the buildup of fluid in the macula resulting specifically from diabetes.
Some people may refer to the condition as diabetic macular retinal oedema or oedema of the eyes.
Diabetic macular edema is among the top causes of vision loss, both globally and within the United States. Worldwide, approximately 100 million individuals have signs of the condition. More than 75,000 Americans are affected by the disease annually.
SEE RELATED: Types of diabetic eye problems
Causes and symptoms
Diabetes mellitus is a chronic health condition characterized by high levels of glucose (sugar) in the blood. Insulin is a hormone in the body that helps regulate these blood sugar levels. When the body does not produce enough insulin or is insulin resistant, diabetes may result. Diabetes can affect many parts and systems of the body, including the eyes.
Diabetes-related macular edema can affect people with Type 1 or Type 2 diabetes. Even women with gestational (pregnancy-related) diabetes are at risk. While it can occur in people who have Type 1 or Type 2 diabetes, it is more common among people with Type 1. Read on to learn the causes, signs and symptoms of diabetic macular edema.
What causes diabetic macular edema?
High blood sugar levels damage cells called pericytes that seal the inside of small blood vessels. When this seal is damaged in retinal cells, the vessels can begin to leak, causing fluid to build up in the macula.
High blood sugar levels can lead to DME in other ways, as well. When blood sugar levels become too high, it can increase inflammation in the body. Inflammation also damages the blood vessels in the eye. This damage may cause them to leak blood and fluid into the retina and surrounding area. The accumulation of fluid in the eye causes the tissues to swell.
These changes cause a condition known as diabetic retinopathy (DR), which is a major factor in the development of diabetic macular edema. In fact, around 50% of those with DR also experience DME. Diabetic macular edema is also the primary cause of blindness among DR patients.
In severe cases of DR, new (abnormal) blood vessels may also develop in the retina. These blood vessels are weaker than normal vessels and may leak even more blood and fluid into the retina.
When the macula swells or thickens from fluid buildup, central vision is affected. Vision loss may occur as the condition progresses. This makes prompt care essential for preserving vision.
What are the signs of diabetic macular edema?
Changes to the retina and macula may indicate the presence of macular edema. Your eye doctor may detect signs of the condition during an eye exam or by performing other tests. Signs of diabetic macular edema may include the:
Swelling or thickening of the macula
Presence of hard exudates (fat and protein deposits) in the macula
Development of microaneurysms (bulges in blood vessels that leak blood or fluid in the eye)
Damage to capillaries (small blood vessels)
Leakage of blood vessels
Abnormal (new) blood vessel growth caused by excess vascular endothelial growth factor (VEGF)
Signs of diabetic retinopathy may also indicate the presence of diabetic macular edema. DR progresses in the following stages:
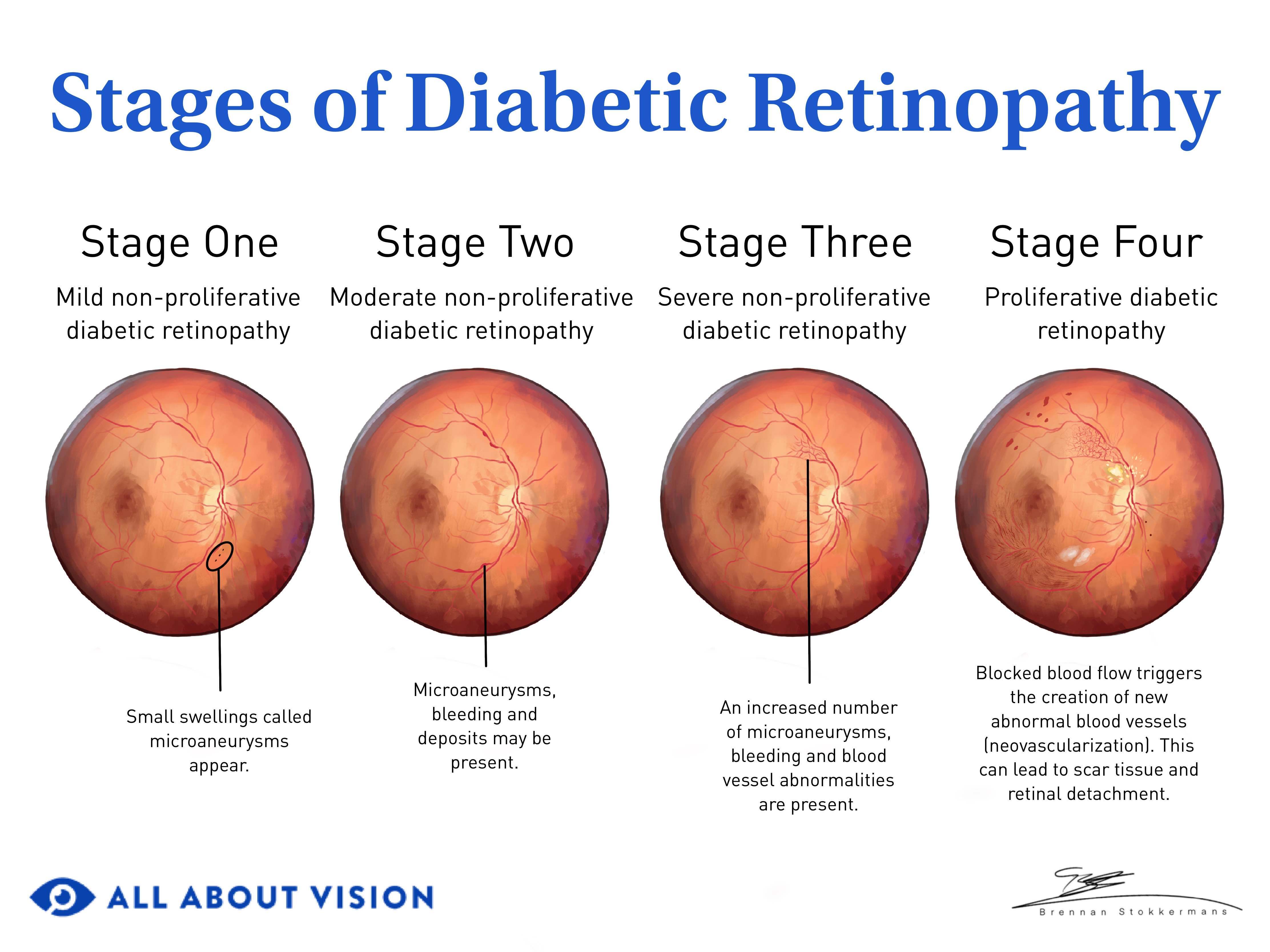
Click image to enlarge.
Mild non-proliferative diabetic retinopathy – Microaneurysms occur in the retina.
Moderate non-proliferative diabetic retinopathy – The number of microaneurysms increases, and hard exudates may develop in the retina.
Severe non-proliferative diabetic retinopathy – Microaneurysms, bleeding in the retina and other vascular changes become more widespread.
Proliferative diabetic retinopathy – Neovascularization (new abnormal blood vessel growth) occurs. This is the advanced stage of DR.
You may experience diabetic macular edema at any point in the progression of diabetic retinopathy. However, as DR advances or worsens, the incidence of DME also tends to rise.
What are the symptoms of diabetic macular edema?
Diabetes-related eye conditions can affect your vision in several ways. The symptoms of diabetic macular edema may include:
Blurry, wavy or distorted vision
Vision loss
Changes in color vision
Difficulty seeing fine details (such as when reading and driving)
Diabetic macular edema symptoms may worsen over time. Some people may experience no visual symptoms.
LEARN MORE: Blurry vision and diabetes
Risk factors
You may have a higher chance of developing macular edema if you have diabetes along with one or more of the following risk factors:
Diabetic retinopathy
Family history of the condition
Prolonged hyperglycemia (elevated blood sugar levels)
Long-term diabetes
Uncontrolled diabetes
High blood pressure
High cholesterol
Kidney disease
Sleep apnea
Pregnancy
Tobacco use
If you have diabetes or feel you may be at risk for diabetic macular edema, visit an eye doctor for an exam.
SEE RELATED: Diabetic eye disease: Are you at risk?
Types of diabetic macular edema
Over the years, doctors have used various systems to classify the types of diabetic macular edema. From a general perspective, it may be categorized into two main types:
Focal – This stage represents the presence of small areas of leakage from microaneurysms. Hard exudates may also develop.
Diffuse – Microaneurysms are also present in this stage, but the leakage is more widespread. Capillary (tiny blood vessel) damage often occurs.
In 2018, the International Council of Ophthalmology created the following guidelines for classifying DME:
Center-involved (ci-DME) – Thickening of the retina that involves the center of the macula
Non-center involved (non-ciDME) – Thickening of the retina that does not involve the macula’s center
These classification systems help doctors determine the best treatment for diabetic macular edema.
Not all types of DME require treatment. Your eye doctor may only need to monitor your condition unless it progresses to clinically significant macular edema (CSME), as defined by these classifications and other criteria.
Diagnosis, management and treatment
Given the risks diabetic macular edema poses to your vision, it is important to have it diagnosed, treated and managed as early as possible. You may need to see a retina specialist for diabetic macular edema treatment. This is an ophthalmologist who specializes in retinal diseases.
How is diabetic macular edema diagnosed?
The process of diagnosing diabetic macular edema begins with a comprehensive eye exam. Your eye doctor may also talk with you about your health history. This may include your history of diabetes and whether you control it through oral medication or insulin.
Your eye doctor may perform one or more of the following tests to determine if you have diabetic retinopathy with macular edema:
Slit lamp exam
A slit lamp exam involves the use of a magnifying microscope and focal light source. Your doctor may use this to examine your retina and other parts of your eye.
Visual acuity test
A visual acuity exam evaluates how clearly you see letters at various distances.
Amsler grid test
The Amsler grid is a type of visual field test. It is used to evaluate central vision for possible issues with the macula, such as swelling or macular degeneration.
Dilated eye exam
Your doctor will place special drops in your eyes to make your pupils wider (dilated). This allows them to see the back of the eye to examine the retina and other structures.
Ophthalmoscopy
A special device called an ophthalmoscope is used to examine various parts of the eye. Along with a light, it contains magnifying lenses and an angled mirror. These components allow your doctor to examine the retina and surrounding structures.
Stereo fundus photography
With this exam, images of a specific area of the fundus are taken from two slightly different angles. (The fundus is the back of the eye and contains the retina and other structures). Your doctor reviews the images to check the macula and screen for the presence of retinal fluid.
Optical coherence tomography (OCT)
OCT is an imaging technique that uses light waves to capture pictures of the eye. It produces cross-sectional images of your retina. These images allow your doctor to see the layers of the retina and identify any changes, such as the thickening of the tissues.
The use of OCT is important for diabetic macular edema detection and management. Your doctor may also use OCT to track the progression of the condition.
Fluorescein angiography
A special yellow dye (fluorescein) is injected into your vein. The dye travels through your blood vessels, including those in the retina. A camera is used to take pictures of your eye as the dye moves through the vessels in the retina. Your doctor then reviews the images to check for areas of vessel leakage and fluid buildup.
After diagnosing the condition, your doctor may recommend treatment based on the severity of the disease.
Advanced diagnostic tools
Advanced technology is being used to develop other ways of detecting diabetic retinopathy and diabetic macular edema. Two of these methods include artificial intelligence (AI) and teleophthalmology. Teleophthalmology involves providing ophthalmic care through digital means.
By identifying retinal changes remotely, these tools make it easier for medical providers (outside of eye care) to detect the early signs of eye conditions. This can lead to earlier diagnosis and treatment and the preservation of vision.
What are treatments for diabetic macular edema?

The recommended treatment for diabetic macular edema is generally based on disease severity. Some cases may not need treatment and are simply monitored for progression. In all cases, managing macular edema, diabetes and any related health factors is an important aspect of treating the disease.
Diabetic macular edema treatment may involve one or more of the following options:
Anti-VEGF medications
When treatment for diabetic macular edema is needed, anti-VEGF medications are usually the first option recommended.
Anti-VEGF medications are given in the form of eye injections. They work by slowing the production of VEGF. This helps reduce the leakage from the blood vessels in the retina.
It also helps reduce or prevent new, abnormal vessel development.
Eye injections are administered according to a specific schedule. This is often monthly, depending on the type of medication used. The anti-VEGF injections commonly used in diabetic macular edema treatment include:
Aflibercept (Eylea) – Aflibercept was approved by the FDA for the treatment of diabetic macular edema in 2014. It is typically given once per month for five months and then once every two months.
Bevacizumab (Avastin) – Bevacizumab has been used as an “off-label” treatment for diabetic macular edema and other eye diseases since 2005. It is usually given once every four to six weeks.
Ranibizumab (Lucentis) – Ranibizumab received FDA approval for diabetic macular edema treatment in 2012. It is typically given once per month.
Brolucizumab (Beovu) – Brolucizmuab became FDA-approved for the treatment of diabetic macular edema in 2022. It is usually given once every month for three months and then every eight to 12 weeks.
Faricimab-svoa (Vabysmo) – Faricimab has been FDA-approved for diabetic macular edema treatment since 2022. It is typically given once every month for four or six months, depending on the extent of the disease. Follow-up dosages vary according to treatment response and individual factors.
Anti-VEGF drugs are administered into the vitreous (clear, gel-like fluid in the eye). For diabetic macular edema, these injections are often given in both eyes.
Corticosteroids
Corticosteroids are medications that help decrease inflammation in the body. They may be used in the treatment of diabetic macular edema to reduce swelling in the retina, particularly when anti-VEGFs are not treating the condition effectively. Steroids may be given as intravitreal injections or in the form of an implant placed within the eye.
Steroids commonly used for diabetic macular edema treatment include:
Triamcinolone acetonide (Taioftal) – This steroid is given as an intravitreal (eye) injection. The effects of the dosage typically last up to three months. However, it may provide therapeutic effects for up to six months or longer.
Dexamethasone (Ozurdex) – Dexamethasone is FDA-approved for the treatment of diabetic macular edema. It is provided through a biodegradable implant placed in the eye. The medicinal effects of this treatment last for around three to six months.
Fluocinolone acetonide (Iluvien or Retisert) – The FDA approved this steroid for treating diabetic macular edema in those who have used corticosteroids without a notable increase in eye pressure. This treatment is delivered through an ocular implant. The implant allows for the sustained release of medication in the eye for up to three years.
Laser surgery
Laser photocoagulation was the standard of care for DME before anti-VEGFs became the first line of treatment. It is still used in some cases today but typically only in those with non-ciDME.
During the procedure, a special laser is directed at microaneurysms and areas of vessel leakage in the retina. The laser energy seals off the leak or destroys the abnormal vessels. This helps prevent further leakage and reduces macular swelling.
Traditional laser photocoagulation is a less favored treatment option. It can pose some risk to the retina and may also cause a small blind spot in the treated area. Newer laser options have been developed to reduce those risks and provide safer laser treatments.
Vitrectomy
A vitrectomy is a surgical procedure in which the vitreous fluid in the eye is removed. The vitreous cavity is then filled with another solution to help maintain the eye’s shape.
Vitrectomy is not as widely used for the treatment of diabetic macular edema as it was in the past. However, it may still be performed in some situations, such as when scar tissue pulls or tugs on the retina. This may also include cases where DME does not respond well to or recurs after anti-VEGF therapy.
Combination treatments
Diabetic macular edema treatments may be combined in some cases. Combination treatments may include:
Anti-VEGF + laser therapy
Steroid injections + laser therapy
Anti-VEGF + vitrectomy
Steroid implants + vitrectomy
Anti-VEGF + steroid implants
Combination treatments have proven more effective for certain cases of the disease.
How is diabetic macular edema managed?
Diabetic macular edema management may include various factors. Managing the condition primarily involves controlling blood sugar levels and diabetes itself. This is true whether DME requires treatment or not.
It also involves keeping your blood pressure and cholesterol (and other blood lipids) within the range recommended by your doctor. These factors are also crucial for managing diabetes-related macular edema.
Your doctor may also recommend other methods of controlling diabetes and diabetic eye conditions. These may involve:
Getting regular exercise
Losing weight (if overweight)
Eating a healthy, balanced diet
Taking diabetes medication or insulin (if needed) as prescribed
Diabetic eye exams are also critical in monitoring and managing diabetic macular edema. These may be recommended yearly or more frequently, depending on your needs.
What happens if diabetic macular edema goes untreated?
Without prompt care, diabetic edema can damage the macula and your central vision. This can affect your ability to read, drive or do other things that require detailed vision. Over time, the condition may progress, leading to permanent vision loss or blindness.
Prevention
Certain risk factors may increase your chances of developing diabetic macular edema. However, there are actions you can take to lower your risk and help prevent its onset. These actions involve:
Managing diabetes – Strict diabetes management can reduce the risk of developing DME and related conditions. This includes keeping your blood sugar levels within the target range.
Controlling blood pressure and blood lipids – Keeping your blood pressure and blood lipids (such as cholesterol) under control can lower your risk of the condition.
Getting regular eye exams – Seeing your eye doctor for annual eye exams is very important, especially if you have diabetes.
Getting eye exams during pregnancy – Women who have diabetes should get eye exams during the first trimester of pregnancy. They should also have eye exams while they are pregnant and for the first year following birth.

Following proper nutrition – Your diet can help you keep your blood sugar levels stabilized. Eating a healthy diet (such as the Mediterranean diet) may help lower the risk of diabetes-related macular edema. Proper nutrition also helps support eye health in general.
Exercising regularly – Getting regular physical activity helps lower your blood sugar levels. This, in turn, may lower your risk of diabetic macular edema.
Quitting smoking – Smoking increases the risk of developing diabetes-related eye diseases. You can help prevent the onset of the condition by avoiding the use of tobacco products.
When to call an eye doctor
If you have diabetes or notice symptoms of macular edema, it is important to see an eye doctor right away. You should also see an eye doctor if you have blurred vision or any vision changes. Seeking prompt care can help preserve your eyesight and lower your risk of vision loss.
READ NEXT: What is maculopathy?
Diabetic macular edema. EyeWiki. American Academy of Ophthalmology. November 2023.
What is macular edema? EyeSmart. American Academy of Ophthalmology. April 2023.
Diabetic macular edema: Diagnosis and management. EyeNet Magazine. American Academy of Ophthalmology. May 2021.
Anatomy, head and neck, eye fovea. StatPearls [Internet]. August 2023.
Anatomy of the eye. Kellogg Eye Center. University of Michigan Health. Accessed February 2024.
What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. April 2023.
Diabetic macular edema. StatPearls [Internet]. May 2023.
Vision loss and diabetes. National Center for Chronic Disease Prevention and Health Promotion; Diabetes. CDC. May 2024.
Pericyte loss in diseases. Cells. July 2023.
Diabetic eye problems. MedlinePlus [Internet]. December 2023.
Diabetic retinopathy pathophysiology. EyeWiki. American Academy of Ophthalmology. February 2022.
Diabetic retinopathy. Johns Hopkins Medicine. Accessed February 2024.
Diabetic retinopathy. University of Michigan Health. Accessed February 2024.
Diabetes-related macular edema: Answers to your most common questions. Health Essentials. Cleveland Clinic. September 2023.
Deep learning to detect OCT-derived diabetic macular edema from color retinal photographs. A multicenter validation study. Ophthalmology Retina. American Academy of Ophthalmology. January 2022.
Diabetic retinopathy. EyeWiki. American Academy of Ophthalmology. July 2023.
Role of microaneurysms in the pathogenesis and therapy of diabetic macular edema: A descriptive review. Medicina. February 2023.
Signs and symptoms of eye microaneurysms. EyeSmart. American Academy of Ophthalmology. May 2023.
Relationship between neovascularization of the optic disc and diabetic macular edema. Clinical Ophthalmology. April 2023.
Distorted vision (metamorphopsia). The Eyes Have It. Kellogg Eye Center. University of Michigan. Accessed February 2024.
Watchful waiting reasonable for patients with diabetic macular edema and good vision. National Eye Institute. April 2019.
Macular edema. National Eye Institute. November 2023.
Multi-ancestry GWAS analysis identifies two novel loci associated with diabetic eye disease and highlights APOL1 as a high risk locus in patients with diabetic macular edema. PLoS Genetics. August 2023.
Association between obstructive sleep apnea and diabetic macular edema in patients with type 2 diabetes. American Journal of Ophthalmology. June 2021.
Optical coherence tomography classification systems for diabetic macular edema and their associations with visual outcome and treatment responses – an updated review. Asia-Pacific Journal of Ophthalmology. June 2022.
Referring patients with DR/DME to a retina specialist. Ophthalmology Times. February 2023.
Slit-lamp biomicroscope. StatPearls [Internet]. June 2023.
Diabetes eye exams. A.D.A.M. Medical Encyclopedia [Internet]. August 2022.
Visual field test. EyeSmart. American Academy of Ophthalmology. March 2022.
What is an ophthalmoscope? Merck Manual Consumer Version. Accessed February 2024.
Fundus camera. StatPearls [Internet]. August 2023.
What is optical coherence tomography? EyeSmart. American Academy of Ophthalmology. April 2023.
Current treatments for diabetic macular edema. International Journal of Molecular Sciences. May 2023.
Tele-ophthalmology: Digital care in the digital world. Stanford Medicine. Accessed February 2024.
Current and novel therapeutic approaches for treatment of diabetic macular edema. Cells. June 2022.
Anti-VEGF treatments. EyeSmart. American Academy of Ophthalmology. July 2023.
Intravitreal injections. EyeWiki. American Academy of Ophthalmology. August 2023.
Aflibercept. EyeWiki. American Academy of Ophthalmology. January 2024.
Bevacizumab. EyeWiki. American Academy of Ophthalmology. February 2024.
Ranibizumab. EyeWiki. American Academy of Ophthalmology. October 2023.
Brolucizumab. EyeWiki. American Academy of Ophthalmology. November 2023.
Faricimab. EyeWiki. American Academy of Ophthalmology. September 2023.
Diabetic macular edema: Safe and effective treatment with intravitreal triamcinolone acetonide (Taioftal). PLoS ONE. October 2021.
Corticosteroids for diabetic macular edema. Taiwan Journal of Ophthalmology. October–December 2019.
The role of laser photocoagulation in treating diabetic macular edema in the era of intravitreal drug administration: A descriptive review. Medicina. July 2023.
Vitrectomy. Johns Hopkins Medicine. Accessed February 2024.
Vitrectomy in diabetic macular edema: A swept-source OCT angiography study. Ophthalmology Science. December 2022.
Combined use of anti-VEGF drugs before and during pars plana vitrectomy for severe proliferative diabetic retinopathy. Ophthalmology and Therapy. September 2023.
Diabetic retinopathy. National Eye Institute. February 2024.
Diabetic retinopathy preferred practice pattern. Ophthalmology. American Academy of Ophthalmology. September 2019.
Diabetes and eye disease. A.D.A.M. Medical Encyclopedia [Internet]. February 2023.
Foods to eat for diabetes-related macular edema. Health Essentials. Cleveland Clinic. September 2023.
Page published on Wednesday, August 14, 2024
Page updated on Tuesday, August 20, 2024
Medically reviewed on Wednesday, July 3, 2024






