Dry eye treatment: How to soothe irritated eyes
How to relieve dry eyes
The best way to treat dry eyes is to find out what’s causing them. There are three main layers to a healthy tear film: water, oil and mucin. A problem with one or more of these tear components can cause temporary dryness or chronic dryness, called dry eye disease (DED).
To determine which part of your tears is causing issues, an eye doctor will need to perform a complete eye exam and dry eye evaluation. Based on how each eye’s surface looks, as well as this dry eye testing, your eye doctor will be able to recommend treatment options.
Some options they may recommend include artificial tears, other types of eye drops, eyelid treatments or specific vitamins and supplements. They may also suggest different therapies you can do at home. Some cases of DED may need prescription medication or surgery to effectively treat the problem.
Click photo to enlarge.
Treating symptoms of dry eyes
If your dry eye symptoms only last a short period of time, you may be able to treat them from the comfort of your home. Frequent or persistent dryness may need prescription treatment from an eye doctor.
Over-the-counter artificial tears, ointments and eye drops
There are many types of lubricating eye drops (also called artificial tears) that you can buy and use without a prescription. These eye drops can treat mild, temporary dryness.
Lubricating eye drops are made with similar elements that your natural tears contain. When applied, the drops work with your tear film to provide comfort, hydration and protection for your eyes.
Some eye drops contain preservatives that help prevent bacteria and other microorganisms from forming in the bottles after they’re opened. Preservatives are not usually harmful to the eye when used fewer than four times per day.

Artificial tears usually are the first step in dry eye treatment.
However, eye doctors often recommend using preservative-free artificial tears to avoid potential irritation or allergies. The packaging should specify whether the product is preservative-free.
It’s important to know that eye drops are not a one-size-fits-all solution. Different types of eye drops address different sources of dry eye. This depends on what part of your tear film is lacking. Some people may require a mixture of two or more artificial tears to treat DED.
If artificial tears don’t seem to do the trick, you may find relief with lubricating eye gels or ointments. These have a thicker consistency than artificial tears, which helps them stay in your eyes longer.
Because they’re thicker, ointments or gels may cause temporary blurred vision. For this reason, many users prefer to apply them before they go to sleep for the night.
SEE RELATED: What are artificial tears used for?
Prescription medications
Severe or chronic DED may need more than what an over-the-counter eye drop can provide. In this case, your eye doctor can prescribe medicated eye drops as dry eye treatment.
Restasis
Restasis, also available generically as cyclosporine eye drops, does more than lubricate the surface of your eyes. It includes an agent that reduces inflammation associated with dry eye syndrome and helps your body produce more natural tears.
But it's important to know that the therapeutic effect of Restasis is not immediate. You must use the drops daily for at least 90 days (about three months) to get the full benefits of this dry eye treatment. Restasis therapy was shown to help the eye make more tears and heal dry eye signs and symptoms for at least two years.
The dosage recommendation for Restasis is one drop in each eye, twice per day, 12 hours apart. Some people experience burning eyes and redness during the first few weeks of use.
CEQUA
CEQUA is another anti-inflammatory eye drop, similar to Restasis. Both eye drops work to reduce inflammation that leads to dry eye symptoms and help you produce more tears naturally.
Unlike Restasis, CEQUA contains about double the dose of cyclosporine. It uses a type of technology that allows for a higher concentration of the medicine to be used in the eye. The consistencies of the eye drop solutions are also different. CEQUA is a water-based solution, while Restasis has more of an oily consistency.
For best results, which may take a few months to notice, apply one eye drop in each eye two times per day.
Xiidra
Xiidra (ZYE-druh) is another prescription eye drop for dry eye treatment. Like Restasis, Xiidra helps reduce the inflammation associated with DED.
The most common side effects of Xiidra reported in studies were eye irritation, altered taste sensation and reduced visual acuity, which occurred in 5% to 25% of participants.
The recommended dosage for Xiidra, like Restasis, is one drop in each eye twice per day. Ideally, the drops should be administered around 12 hours apart.
NOV03
NOV03 (100% perfluorohexyloctane) is a new eye drop for DED that targets symptoms caused by meibomian gland dysfunction (MGD). NOV03 claims to target excessive tear evaporation to help the eyes stay hydrated.
The drops are made from a non-steroidal formula that does not contain water or preservatives. While the FDA has accepted the New Drug Application filing for NOV03, the eye drops won’t be available for public use until June 2023.
Steroid eye drops
Inflammation has been recognized as a significant cause of DED. It frequently causes redness and burning associated with dry eye disease.
Artificial tears don’t usually address these inflammatory changes. Your doctor may recommend steroid eye drops to better manage the underlying inflammation associated with dry eyes.
Steroid eye drops like loteprednol etabonate ophthalmic suspension 0.25% (Eysuvis) are used short-term to quickly manage symptoms. They are often used in addition to artificial tears and Restasis or Xiidra. This cocktail of eye drops combines the short-term solution with the long-term dry eye treatment strategies.
Steroid eye drops (especially if used for long periods) have the potential to cause side effects. It's important to make your eye doctor aware of your full medical history before starting steroid eye drops.
Lacrisert
Lacrisert (Bausch + Lomb) is a sterile, slow-release lubricant. It is placed under the lower eyelid where the inner eyelid meets the eyeball.
It is a solid insert composed of a preservative-free lubricating agent that slowly liquefies over time. This provides an all-day moistening effect.
Lacrisert is recommended for patients with moderate to severe DED symptoms — especially if artificial tears alone are unsuccessful. A single Lacrisert should be applied once a day for all day relief.
Punctal plugs
Both the upper and lower eyelids contain a punctum (the opening of the tear duct). The punctum allows the tears to drain away from the eye through the lacrimal duct into the back of the nose. Punctal plugs, also called punctum or lacrimal plugs, are inserted into the opening of the punctum to help maintain a better tear film.
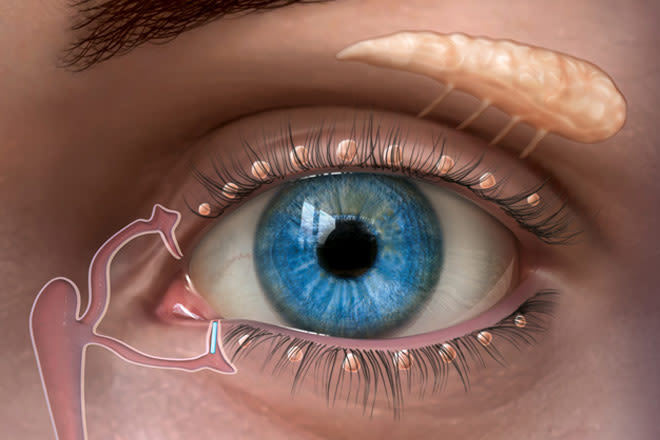
A punctal plug inserted in the tear duct of the lower eyelid to keep the eye’s tear film from draining away too quickly. Image: Oasis Medical, Inc.
Since about two thirds of the tears drain through the lower punctum, this is the one that is generally treated. In this way, the eye is able to retain more of its own tears.
Punctal plugs are biocompatible and about the size of a grain of salt. They can be inserted into the eyelid in the outpatient clinic during a dry eye evaluation. The process does not hurt, and it is usually impossible to feel the punctal plug in the eyelid afterward.
Tyrvaya
Tyrvaya (teer-VI-uh) is a prescription nasal spray that can help treat symptoms of chronic dry eye syndrome. The spray works through the nerve endings inside your nose to activate tear film production.
This should allow users to create more of their own natural tears rather than relying on artificial tears. The most common side effects are sneezing, coughing and irritation in the nose and throat.
For the best results, Tyrvaya should be sprayed once into each nostril twice per day. The medication should just touch the inside of the nostril and not be inhaled or squirted up into the nose.
Be sure to follow your eye doctor’s directions about which eye drops to use and how often you use them. Using a different brand or multiple brands of artificial tears will make it difficult to assess the success of the dry eye treatment your doctor recommended.
Nutrition for dry eyes
Dry eye treatment consists not only of what you put into the eyes, but also of what you put in your body. Incorporating certain vitamins, supplements and foods into your diet can reduce eye dryness.
Vitamins and supplements
For a long time, omega-3 fatty acids were considered the best nutritional supplements to reduce or treat dry eye. This is because omega-3s are anti-inflammatory in nature.
However, recent studies have challenged this belief. One study examined eye dryness of participants who took omega-3 supplements daily compared to those who took olive oil instead. Results showed that both omega-3 supplements and olive oil helped reduce DED.
Since olive oil contains no omega-3s and still reduced DED, this study has raised questions about the helpfulness of omega-3s. But many doctors still recommend trying them to see if they work for you. If you notice an improvement after a month, keep taking them. If not, you can stop taking them.
It’s important to note that omega-3s aren’t a fit for everyone. For example, people who are on blood thinners should avoid omega-3s due to an increased risk of bleeding. Talk to your doctor before adding any new medicines or supplements to your regimen.
Other vitamins and supplements that may improve or treat dry eyes include:
Vitamin A – can help protect the cornea by forming a barrier against bacteria
Vitamin B12 – can help repair the nerve layer of the cornea, which may reduce eye pain and burning
Vitamin D – can reduce inflammation and improve the quality of tears produced
Foods
There is evidence that the best foods for dry eye treatment are those that are rich in omega-3 fatty acids and the vitamins listed above. Superior sources of omega-3s and Vitamins A, B12 and D include:
Cold-water fatty fish including salmon, tuna, sardines, mackerel and herring
Plant oils such as canola oil, soybean oil and flaxseed oil
Fortified foods, including certain brands of infant formula, milk, yogurt, eggs, juices and soy beverages
Seeds and nuts such as walnuts, chia seeds and flaxseed
Leafy green vegetables such as kale, broccoli and spinach
Orange and yellow produce including carrots, squash, cantaloupe, pumpkin, mango and sweet potatoes
Red produce such as tomatoes and red bell peppers
Liver or cod liver oil
Red meat
Poultry
Cheese
Orange juice fortified with Vitamin D
Fortified breakfast cereals
Dairy and plant milk fortified with Vitamin D
The best way to modify your diet to help treat dry eyes is to replace high-sugar and processed foods with many of the eye-healthy foods listed above. Sugary and processed foods tend to increase inflammation that contributes to dry eyes.
SEE RELATED: How better nutrition can improve your vision
Warm compress
Dryness can occur when the eyelid glands that release oil-based tear film become stagnant. These glands, called the meibomian glands, may benefit from warm compresses.
The warmth and humidity of the compress can help loosen clogged or stagnant oil from the glands. Warm compresses also stimulate meibum production, which can soothe irritated eyes.
To do this, wet a clean washcloth with very warm (not hot) water. Wring out any excess water, then gently press the washcloth against closed eyelids.
It’s important for the eyelids to get consistent warmth for at least five to 10 minutes. Washcloths don’t stay warm this long, so you need to rewarm them about every two minutes.
Store-bought options are often designed to stay warm longer. These include products such as Brudermask and Thermalon Dry Eye Compresses. The best way to prepare at-home warm compresses is with the washcloth “bundle method.”
Some things to consider when using a warm compress on the eyes:
Only place warm compresses over the eyes, not hot. Excessive heat can scald or burn the delicate skin on and around the eyelids.
Use a new, clean washcloth every time you do a warm compress. This helps prevent the spread of bacteria and potential infection.
Warm compresses may need to be applied daily for chronic dry eye treatment. However, overuse can cause irritation, especially when a wet cloth is used. Ask your doctor for recommendations on how often and how long you should use warm compresses.
Eye massage
An eyelid massage can help release the oil that was loosened with the compress. This can also promote new oil production. However, you should always massage the eyelids gently, especially after a warm compress. The corneas are even more susceptible to distortion while they are warm.
After washing your hands with soap and water, use your fingers to softly massage the upper and lower eyelids. Massage downward on the upper eyelid, and massage upward on the lower eyelid. Do this starting at the inner corner of the eye and moving outward toward the ear.
It’s best to massage each eyelid for about 30 seconds while keeping the eyes closed. Repeat five to 10 times on each eye.
Eyelid heating and massage treatments
Various treatments are available to help dry eyes caused by meibomian gland dysfunction. Some of these treatments are done using thermal pulsation systems, which combine the best features of warm compress therapy and meibomian gland expression. Other systems deliver heat therapy and rely on the doctor to massage the eyelid.
Eyelid heating and massage systems go by different names depending on the manufacturer. LipiFlow is developed by Johnson & Johnson, iLux by Alcon, TearCare by Sight Sciences and MiBo Thermoflo by MiBo Medical Group. However, the treatment they provide is generally the same.
A device fits over the eyelids and applies precisely controlled heat to the lids. This softens hardened meibum trapped in the meibomian glands. At the same time, the pulsation system (or the eye doctor) applies pulsed pressure to the eyelids. This opens and expresses the clogged glands, restoring the balance of oils in the tear film.
While the duration of each system varies, LipiFlow and iLux treatments take approximately 12 minutes per eye. Patients often notice an improvement in symptoms within two weeks of treatment. However, it can take a few months for improvements to become apparent. Results of the LipiFlow and iLux procedures were shown to last three months to a year or longer.
Potential side effects from LipiFlow dry eye treatment include corneal abrasion, eye pain, swollen eyelids and eyelid irritation or inflammation. Other side effects include chalazia, transient blurred vision, itching and red eyes. The eyes may also feel dry for a day or so after the treatment. LipiFlow removes the oil from the meibomian gland, so the oily layer of the tear film needs time to restore itself.
LipiFlow and iLux are not usually covered by health insurance. Costs can vary from one practitioner to another, but LipiFlow costs around $900 per session, and iLux is between $600 and $700 per session.
Lifestyle changes
There are many lifestyle choices that could cause eye dryness without you realizing it. Adjusting these choices can help reduce or eliminate your symptoms.
Personal circumstances that may cause or worsen dry eyes include:
Smoking or being around smoke
Living in an extremely cold, dry or windy climate
Spending long periods of time staring at a screen
Being dehydrated
Taking certain medications
Lacking adequate sleep each night (7 to 8 hours)
While some of these things are out of your control, making small changes where you can may improve your dry eyes.
SEE RELATED: How to find the best eye drops for your symptoms
Treatments for underlying causes of dry eye
Besides lifestyle choices, there could be several underlying causes for your dry eye problems. Underlying causes can range from contact lens wear to certain medical conditions or medications.
It’s also possible for other eye-related problems to cause dryness. In this case, an eye exam can lead to proper treatment.
Contact lenses
Technically, wearing contact lenses does not cause DED. But it can make the condition worse. Studies estimate that half of contact lens wearers complain of eye dryness and discomfort at the end of the day. Additionally, 25% to 30% of wearers stop using contact lenses due to the dryness and discomfort they experienced when wearing them.
Experts believe that the irritation felt by certain contact lens wearers is due to having a weak or thin tear film. When you add contact lenses to the mix, it emphasizes the tear film problem and creates discomfort.
Lubricating eye drops can soothe the irritation felt when wearing contact lenses. It’s not recommended to apply most eye drops while wearing contacts. But certain formulas, like Refresh Relieva for Contacts and Blink Contacts lubricating eye drops, are safe to use while wearing contacts.
There are also specific contact lenses for dry eyes that may reduce grittiness and irritation. Scleral contact lenses, which are larger than typical contacts, rest over the white parts of the eye. This tends to be more comfortable for users — especially for those with extreme dry eye.
Medical conditions
Underlying medical conditions can cause inflammation, leading to DED. The most common conditions related to dry eyes include:
If you’ve been diagnosed with one or more of these conditions, talk to your doctor about dry eye treatment options. Other biological changes that can cause DED include aging, pregnancy and menopause.
SEE RELATED: Risk factors that can affect women’s vision
Check your medications
Specific medicines taken can cause your eyes to become gritty and irritated. Taking the following categories of medications may cause or worsen dry eyes:
Antihistamines and decongestants (Antazoline, Brompheniramine, Carbinoxamine, Pyrilamine)
Beta blockers (Propranolol, Oxprenolol, Metoprolol)
Pain relievers (Morphine)
Antidepressants (Amitriptyline, Desipramine, Imipramine, Protriptyline, Nortriptyline)
Anxiety medications (Xanax, Valium, Klonopin, Ativan)
Anti-nausea medications (Trifluoperazine, Thiethylperazine, Tetrahydrocannabinol, Scopolamine)
Gastrointestinal (GI) medications (Atropine, Methscopolamine)
Antipsychotic medications (Acetophenazine, Carphenazine, Chlorpromazine, Fluphenazine, Methotrimeprazine, Mesoridazine)
Medications used to treat Parkinson’s disease (Ethopropazine)
Acne medications (Accutane)
Hormone treatments (Birth control pills, hormone replacement therapy, medical fertility (IVF))
Chemotherapy medicines
If you feel your dry eye has worsened since starting a particular medicine, discuss this with your doctor. They may be able to suggest an equally effective alternative that won’t cause dry eyes.
Consider your screen time
Spending time in front of a screen, whether it be a smartphone, tablet or computer, can cause the eyes to become dry, irritated and fatigued. This is a condition known as digital eye strain or computer vision syndrome.
The main reason screen time leads to DED is because we blink less when focusing on a screen. Blinking spreads tear film across the surface of the eyes, which keeps them hydrated.
Without computer use, people blink an average of 18.4 times per minute. When focusing on a digital screen, that number drops to 3.6 blinks per minute. Blinking only three times per minute is not nearly enough to keep the eyes clear and hydrated.
When using a screen, it’s important to blink frequently and to take regular breaks. Eye care experts recommend the “20-20-20 rule.”
The rule encourages screen users to take a break every 20 minutes. During the break, focus on an object at least 20 feet away for at least 20 seconds. You can also close the eyes for a few seconds to allow the eyes to rest.
See an eye doctor
Problems within the eye itself may also cause eye dryness. Regular eye exams can help your eye doctor detect, treat and manage these conditions. Addressing any underlying conditions can ultimately help to treat dry eye.
Three common eye conditions that can cause dry eyes include meibomian gland dysfunction, blepharitis and lagophthalmos.
Meibomian gland dysfunction
The meibomian glands are small glands in the eyelids that produce the oil component of tear film. When these glands become clogged or inflamed, it can reduce the amount of oil (called meibum) in your tears. This is a common condition called meibomian gland dysfunction (MGD).
The oil layer of tears keeps the water layer from evaporating, which helps lock in moisture. When the oil layer is lacking, the water layer evaporates, leaving the eyes feeling dry.
Treatment for MGD can consist of at-home therapies, like warm compresses and eyelid massages. There are also in-office therapies that use machines to help meibomian gland function. If you think you have MGD, talk to your eye doctor about treatment recommendations.
Blepharitis
Blepharitis is a condition that affects the eyelids, causing them to become swollen, itchy and red. It often occurs due to excess bacteria on the eyelids or when oil glands become irritated.
Dry eyes are a complication of blepharitis that happens when oil and/or flakes from the eyelid build up in your tear film. This buildup can cause the eyes to feel dry.
Blepharitis is often treatable with frequent eyelid cleansing. Some studies also suggest using tea tree oil or hypochlorous acid to aid in dry eye symptoms. Lotilaner ophthalmic solution, 0.25% is an eye drop that was shown in clinical trials to successfully treat demodex blepharitis and may be available by prescription in 2023.
Over-the-counter eye drops and antibiotics can also be helpful when dealing with blepharitis. Keep in mind that treatment for underlying conditions, such as rosacea or dandruff, may also be needed.
Lagophthalmos and floppy eyelid syndrome
Lagophthalmos is a condition in which a person cannot completely close the eyelids. This may occur when blinking or sleeping (nocturnal lagophthalmos).
Floppy eyelid syndrome is caused by a softening of the eyelids that allows them to come open during sleep. This exposure dries out the eyes and leaves them vulnerable to rubbing on the pillow.
As mentioned earlier, blinking is important for maintaining healthy eyes and tear film. When the eyes cannot close completely, or they come open during sleep, the tear film becomes unstable and evaporates faster than normal.
Serious problems with the cornea can occur if left untreated. Complications include keratopathy, corneal ulcers and corneal protrusion. Treatment for lagophthalmos may include artificial tears, eye ointment or gel, eyelid taping at nighttime and moisture chamber glasses. Several surgical options are also available to treat severe cases.
Before trying any treatment for dry eye, get professional insight from an eye doctor. They can assess your symptoms and suggest the best possible dry eye treatment for you.
READ MORE: Corneal erosion
Dry eye. American Optometric Association. Accessed January 2023.
Lubricating eye drops for dry eyes. American Academy of Ophthalmology. EyeSmart. February 2022.
Restasis (eye drops) uses, dosage, side effects. Drugs.com. May 2022.
Practical guidance for the use of cyclosporine ophthalmic solutions in the management of dry eye disease. Clinical Ophthalmology. July 2019.
Xiidra: uses, dosage, side effects & warnings. Drugs.com. October 2022.
Xiidra side effects. Drugs.com. November 2022.
FDA accepts NDA of NOV03 for DED associated with MGD. Optometry Times. September 2022.
Rethinking dry eye disease with acute steroid treatment. Ophthalmology Times. December 2021.
Lacrisert (hydroxypropyl cellulose) basics, side effects, reviews & more. GoodRX. November 2021.
Tyrvaya (varenicline solution) nasal spray. Tyrvaya. Accessed January 2023.
New study finds fish oil omega-3s EPA and DHA work differently on chronic inflammation. Tufts Now. December 2020.
The Dry Eye Assessment and Management (DREAM) extension study - A randomized clinical trial of withdrawal of supplementation with omega-3 fatty acid in patients with dry eye disease. The Ocular Surface. January 2020
The latest thinking on dry eye treatments. Harvard Health Publishing. October 2022.
The role of nutrition and nutritional supplements in ocular surface diseases. Nutrients. March 2020.
Omega-3 fatty acids. National Institutes of Health. July 2022.
Vitamin A: The nutrition source. Harvard T.H. Chan School of Public Health. Accessed January 2023.
Vitamin B12: The nutrition source. Harvard T.H. Chan School of Public Health. Accessed January 2023.
Vitamin D: The nutrition source. Harvard T.H. Chan School of Public Health. Accessed January 2023.
Self-help for dry eye syndrome. News-Medical. December 2022.
Dry eye therapy: Keeping it simple. Review of Optometry. November 2018.
Efficacy and safety evaluation of a single thermal pulsation system treatment (Lipiflow®) on meibomian gland dysfunction: a randomized controlled clinical trial. International Ophthalmology. September 2022.
12 devices for treating dry eyes. American Academy of Ophthalmology. EyeSmart. November 2020.
Systane iLux. MyAlcon. Accessed January 2023.
Dry eye. National Eye Institute. April 2022.
Scleral contact lenses might be the best solution you’ve never heard of for dry eye and more. University of Utah Health. August 2022.
Dry eye. Johns Hopkins Medicine. Accessed January 2023.
Dry eye. Penn Medicine. Accessed January 2023.
Ocular manifestations of isotretinoin. American Academy of Ophthalmology. EyeWiki. August 2022
Ocular implications of medical fertility and hormonal treatment. American Academy of Ophthalmology. EyeWiki. Accessed January 2023.
8 cancer treatment-related eye changes and how to manage them. MD Anderson Cancer Center. June 2021.
Increased screen time and dry eye: Another complication of COVID-19. Eye & Contact Lens: Science & Clinical Practice. August 2021.
The 20-20-20 rule. Canadian Association of Optometrists. November 2022.
Comprehending, catching and correcting MGD. Review of Optometry. March 2021.
Blepharitis. National Eye Institute. August 2020.
The use of tea tree oil in treating blepharitis and meibomian gland dysfunction. Oman Journal of Ophthalmology. January 2018.
Hypochlorous acid can be the novel option for the meibomian gland dysfunction dry eye through ultrasonic atomization. Disease Markers. January 2022.
Beating the mighty Demodex mites. Ophthalmology Times. March 2022.
Lagophthalmos. StatPearls [Internet]. July 2022.
Floppy eyelid syndrome: a comprehensive review.The Ocular Surface. January 2020.
Page published on Saturday, April 18, 2020
Page updated on Tuesday, February 28, 2023
Medically reviewed on Friday, February 3, 2023