Ischemic optic neuropathy (ION)

What is ischemic optic neuropathy?
Ischemic optic neuropathy (ION) is a condition in which blood flow to the optic nerve is interrupted, which can lead to a loss of vision. ION is considered a type of eye stroke. An injury of the optic nerve due to ION is usually permanent.
The optic nerve transmits visual images from the eye to the brain. Without proper blood flow, the nerve does not receive important nutrients and oxygen. This can damage the nerve and lead to sudden blurriness and vision loss.
Types of ION
There are two types of ischemic optic neuropathy:
Posterior ischemic optic neuropathy (PION) – Blood flow to the back portion of the optic nerve – the part closest to the brain – is blocked or reduced. This is rare.
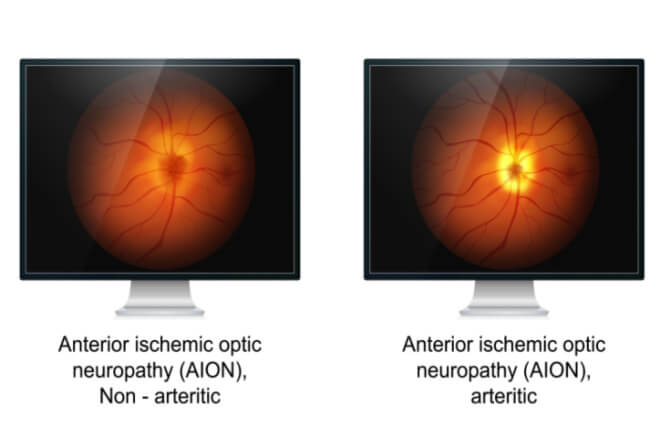
Anterior ischemic optic neuropathy (AION) presents blocked or reduced blood flow to the front portion of the optic nerve.
Anterior ischemic optic neuropathy (AION) – Blood flow to the front portion of the optic nerve – the part that attaches to the eyeball – is blocked or reduced. This type of ION has two different forms known as arteritic and nonarteritic.
Arteritic is caused by a condition called temporal arteritis (also called giant-cell arteritis – GCA). It causes inflammation of the arteries that provide blood to the optic nerve. This condition is called arteritic anterior ischemic optic neuropathy (A-AION). GCA can cause severe vision loss and even death. This is because it also affects other arteries in our body – including those of the brain and around our heart. It can lead to a brain stroke or heart attack. In the case of GCA, the optic nerve is usually completely damaged, causing rapid blindness of the eye. Without immediate treatment, the other eye is very likely to become affected. This often happens within days to weeks.
Nonarteritic is called nonarteritic anterior ischemic optic neuropathy (NA-AION). NA-AION is caused by low blood circulation in the arteries that provide blood to the optic nerve. This form is associated with vascular disease and is less likely to cause severe vision loss. The other eye is usually not affected.
Symptoms of ischemic optic neuropathy
In A-AION, vision loss is often preceded by the systemic symptoms of GCA. These include:
Pain in the temples or neck
Pain and aches in the upper arm or leg muscles
Pain or tingling in the scalp
Pain while chewing
Fever
Fatigue
Unexplained weight loss
Reduced appetite
Vision loss is painless and may only last for a few minutes. This type of temporary vision loss is called a transient ischemic attack (TIA) or amaurosis fugax. It occurs in one out of three patients with A-AION and is usually followed by permanent vision loss within a few days.
Two out of three patients with A-AION are not warned by a TIA and experience sudden, severe vision loss in one eye. Unless treated, A-AION in one eye is generally followed by the other eye within days to weeks.
NA-AION can cause painless and abrupt vision loss as well. But it is much less likely to occur in the other eye and does not require immediate treatment. Vision loss from NA-AION is often present without warning when someone wakes up.
SEE RELATED: Optic neuritis and neuropathy: Symptoms, causes, treatments
What causes ischemic optic neuropathy?
ION is caused by reduced or blocked blood flow to the optic nerve. In many cases, this lack of blood flow is associated with underlying conditions
Conditions include the following:
Temporal arteritis (giant-cell arteritis)
Hypertension (high blood pressure)
Hypercholesterolemia (high cholesterol)
Sometimes, ION can also occur after spinal or cardiac surgery. This can be as a result of low blood pressure, fluid balance or anemia that occurs during the procedure.
Risk factors of ischemic optic neuropathy
Arteritic anterior ION is overwhelmingly found in people over 55. It’s also up to three times more likely to affect women than men. Half of all patients with temporal arteritis have a rheumatological condition called polymyalgia rheumatica (PMR). Patients with PMR have muscle aches and stiffness of the shoulder and hip muscles.
Nonarteritic anterior ION is also likely to affect people 50 years and older. Although anyone can have it, at any age. Both women and men have the same chances of developing this type of ION.
To have an optic nerve that is smaller or is completely filled with nerve fibers puts one at an increased risk for NA-AION. The optic nerve is like a cable that can be partially or completely filled with nerve tissue.
When someone is born without any space in the middle of the nerve, it is also called a crowded optic disc. Whether you have a crowded optic disc can be measured by your eye doctor during a routine eye exam.
The following can also increase the chances of developing NA-AION:
Smoking cigarettes
Clogged arteries
Anemia
Vasculitis (inflammation in the blood vessels)
Low blood pressure
SEE RELATED: How smoking harms your eyes
How is ischemic optic neuropathy diagnosed?
The first step in diagnosing ischemic optic neuropathy is an eye exam to check for potential signs of ION. During the exam, your ophthalmologist will dilate your pupils. This will allow them to see any swelling in the blood vessels located in the back of the eye and in the optic nerve.
Your peripheral vision and the pressure of the fluid in your eyes may also be tested. You may have an optical coherence tomography scan of the optic nerve.
Blood tests are also performed to check for temporal arteritis, a condition that is often associated with ION. There are instances in which the blood tests do not provide a clear answer. In these cases, a biopsy of the temporal artery, on the side of the temple, may need to be done to accurately make the diagnosis.
Ischemic optic neuropathy treatment
Any underlying conditions that are considered a risk factor for ION should be treated appropriately to help prevent ION from developing. In the case of A-AION, there are almost always warning symptoms that should prompt an immediate visit to the eye doctor or the emergency room.
Temporal arteritis is treated with steroids such as prednisone. This helps reduce swelling of the arteries and prevents A-AION from worsening. It also greatly reduces the risk that the other eye goes blind and the risk of heart attack and brain stroke.
When there is a suspicion of GCA, the doctor may decide to start steroid pills even before the results of the blood tests have come back.
Unfortunately, vision loss caused by ION can’t be recovered. But the above treatments can keep vision loss from progressing. Tools such as magnifiers and other low vision aids can be useful for those who have lost their vision.
READ MORE: Stroke Awareness Month
What is ischemic optic neuropathy? Barrow Neurological Institute. Accessed December 2022.
What is ischemic optic neuropathy? American Academy of Ophthalmology. May 2022.
Eye stroke — Penn Ophthalmology. Penn Medicine. Accessed December 2022.
Diagnosing and managing ischemic optic neuropathy. Review of Ophthalmology. October 2010.
Polymyalgia rheumatica. Mayo Clinic. June 2022.
Cup-disc ratio and ischemic optic neuropathy. Archives of Ophthalmology. August 1985.
Strategies to prevent ischemic optic neuropathy following major spine surgery: A narrative review. Journal of Clinical Anesthesia. December 2017.
Cardiovascular disease in large vessel vasculitis: Risks, controversies and management strategies. Rheumatic Disease Clinics of North America. February 2023.
Risk factors for non-arteritic anterior ischemic optic neuropathy: A large scale meta-analysis. Frontiers in Medicine. October 2021.
Anterior ischaemic optic neuropathy: Differentiation of arteritic from non-arteritic type and its management. Eye. January 1990.
Amaurosis fugax in ocular vascular occlusive disorders: prevalence and pathogeneses. Retina. January 2014.
Page published on Wednesday, January 11, 2023
Page updated on Tuesday, January 17, 2023
Medically reviewed on Sunday, December 4, 2022






