Best disease
What is Best disease?
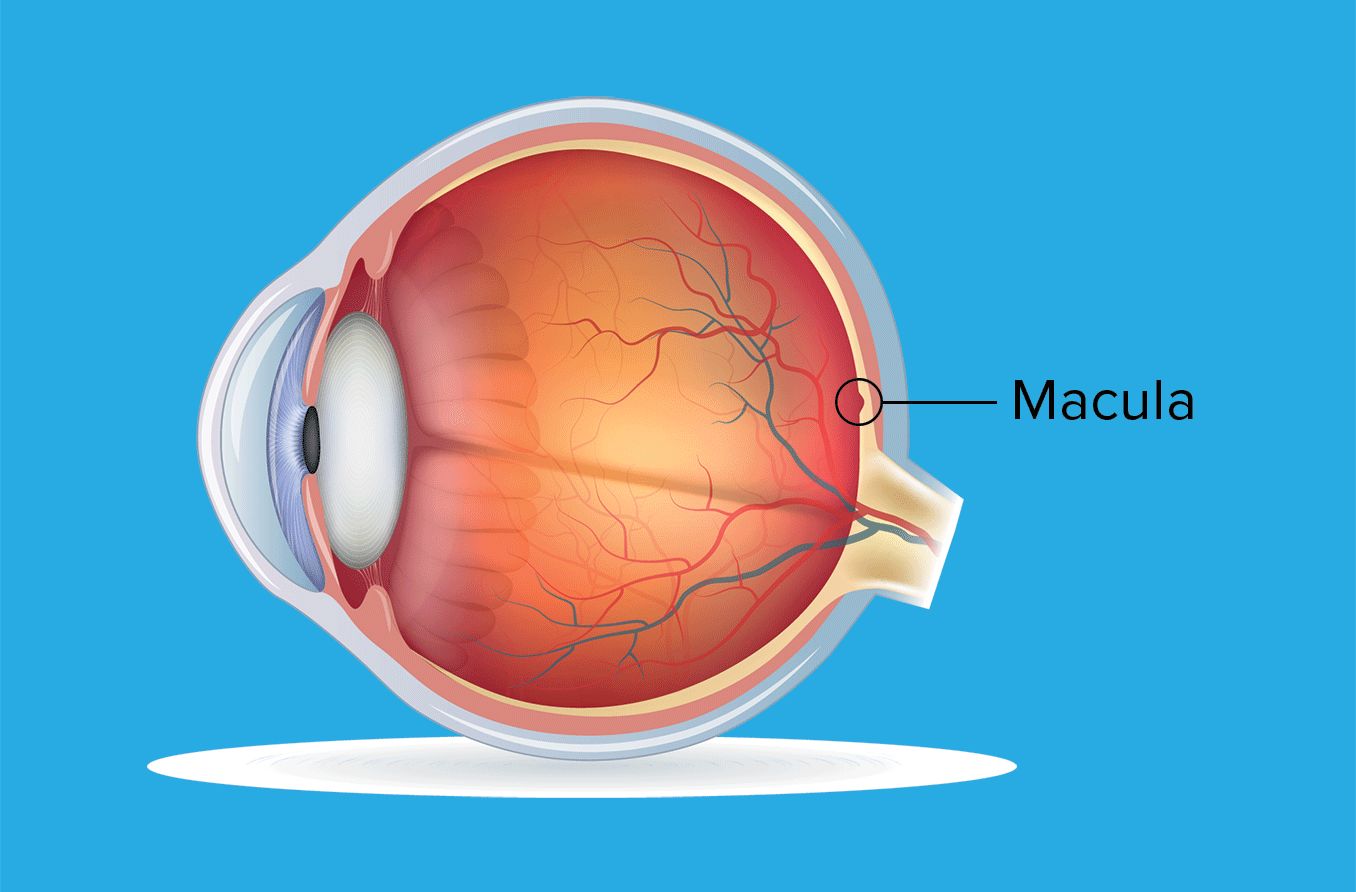
Best disease is a condition that causes damage to an area of the retina — the layer of tissue at the back of the eye — the macula. The macula supports central vision, the part of vision that allows individuals to clearly see details, colors and shapes.
This condition, also called vitelliform macular dystrophy, is hereditary. However, its impact on vision doesn’t usually occur until later in the individual’s life.
Best disease is named for Dr. Friedrich Best who gave a detailed analysis of the condition in 1905.
What causes Best disease?
Best disease is in the retinal/macular dystrophy family — a group of conditions caused by genetic mutations that impact the eye.
Bestrophinopathies are a subgroup of this family. This subgroup contains diseases caused by a mutation on the BEST1 gene. There are more than 250 potential mutations that can impact this gene.
Best disease is the most common hereditary condition that damages the macula.
Genetic inheritance
Humans are born with two sets of chromosomes — one set from each biological parent. Inside these chromosomes are all of their genes, which contain the “blueprints” for the body’s development.
Some genes are dominant, meaning they overrule their matching gene in the second chromosome. Others are recessive and can be overruled. In order for a recessive trait to be observable, the individual must have two recessive genes for it.
Best disease is an autosomal dominant gene. This means that, of an individual’s two copies of the BEST1 gene, a mutation in only one copy will result in the disease. When that individual has children, if their partner has two normal BEST1 genes, there is a 50% chance their offspring will inherit a mutated gene.
Because the mutation that causes Best disease is dominant, any individual with a copy of the mutation will develop the condition.
Macular damage
The layer of tissue at the back of the eye is called the retina. It takes the light that enters the eye and turns it into nerve signals, which are sent to the brain through the optic nerve. This is what allows us to see images.
The macula is the center of the retina. It is what allows us to see images and details that are directly in front of us. This means that it is responsible for helping with:
Reading text
Facial recognition
Color identification
Noticing small movements
When the macula is damaged, an individual can still see, but their vision typically has a blurry area in the center.
For individuals with Best disease, the macula develops lesions — abnormal spots of tissue. These lesions usually appear in both eyes (bilaterally) in similar locations.
What are the signs of Best disease?
Best disease typically occurs in five stages:
Stage 1 – The macula’s appearance is healthy and vision is unimpaired.
Stage 2 – The vitelliform stage usually occurs between the ages of 3 and 15. A lesion that looks like an egg yolk develops on the macula. Vision may be slightly impaired.
Stage 3 – The pseudohypopyon stage usually occurs during the teenage years. Some of the lesion’s matter can cause a cyst under the retina. A cyst is a pocket of tissue that may be filled with fluid, air or pus. Vision may still be only slightly impaired.
Stage 4 – The vitelliruptive stage occurs when the lesion begins to break apart. The broken lesion often looks like scrambled eggs. Vision may worsen, leading to difficulty reading small print or giving a wavy appearance to straight lines.
Stage 5 – The atrophic stage occurs after the lesion’s matter begins to disappear. Scarring and damage to the retina remains, more seriously impacting vision.
Around 20% of affected individuals will experience a sixth stage. This stage is called the choroidal neovascularization (CNV) stage. When the eye creates new blood vessels to try to repair the damaged macula, the vessels of those with CNV will leak blood. This can cause scar tissue to build up and further impair vision.
It is possible to have Best disease and not experience any vision impairment. In many cases, the fourth and fifth stages — which are most likely to affect visual clarity — do not develop until the individual is in their 40s or older. The level of impact to sight varies based on the individual. There is no pain associated with Best disease.
How is Best disease treated?
There are no current treatments for Best disease. However, researchers are looking into gene therapy as a way to help stop, and potentially reverse, the damage. This would involve replacing the mutated BEST1 gene with a normal BEST1 gene. This research is still in the early stages.
Genetic testing
There is genetic testing available to check for Best disease. This can help determine the likelihood of passing the disease to a child. It can also help confirm the diagnosis of Best disease.
Making the most of your vision
Because Best disease only impacts part of an individual’s vision, there are things that can be done to help compensate. Using bright lights and bold colors can help make things easier to distinguish. Increasing the size of texts and images can also help.
There are also low vision specialists who may be able to provide more resources to help with daily living.
When should you see a doctor?
Because Best disease may not impact vision until later in an individual’s life, annual eye exams are helpful to keep track of any changes to the macula. If your vision becomes blurry or you find it difficult to distinguish small details, it is important to seek the help of an eye doctor.
Best disease. Foundation Fighting Blindness. Access October 2022.
Best disease and bestrophinopathies. EyeWiki. May 2022.
Central vision. New York Presbyterian. January 2022.
Best disease (Best vitelliform macular dystrophy). Royal National Institute of Blind People. September 2022.
Genes and genetics explained. Better Health Channel. September 2019.
Retina. Cleveland Clinic. April 2022.
Macula. Cleveland Clinic. May 2022.
Lesion. National Cancer Institute. Accessed October 2022.
Cyst. National Cancer Institute. Accessed October 2022.
Page published on Thursday, October 27, 2022
Page updated on Monday, October 31, 2022
Medically reviewed on Saturday, October 15, 2022






