Macular edema: Symptoms, causes, diagnosis and treatment
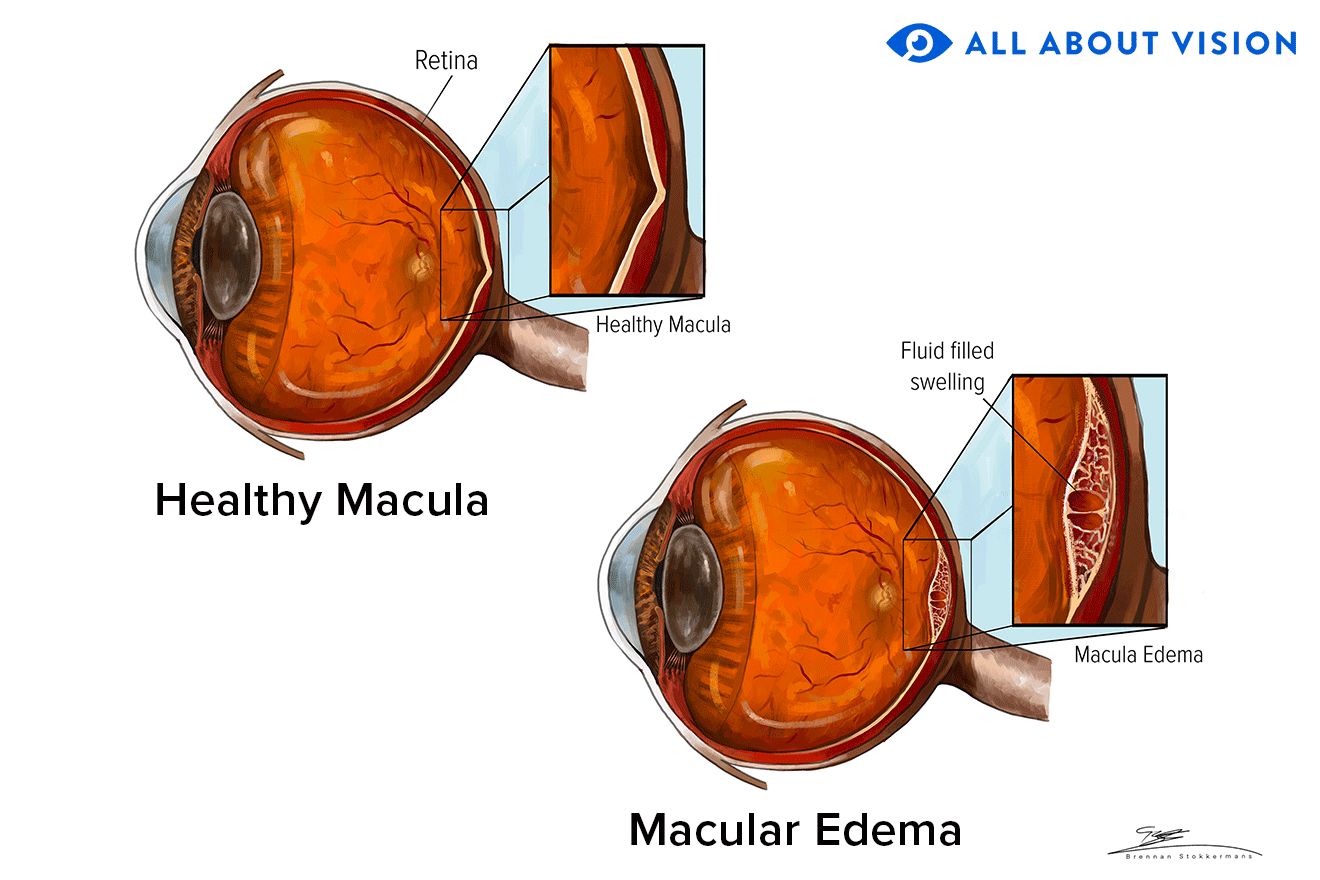
What is macular edema?
Macular edema is when the retina (the layer of light-sensitive cells that line the inside of the eye) develops a central fluid blister. The macula is the part of the retina that provides your “straight ahead” or central vision, allowing you to see colors and small objects.
There are many causes of macular edema. If not treated, it can leave a permanent blind spot in the center of our vision.
Symptoms of macular edema
Macular edema causes vision to be distorted and blurred. It can also make objects appear bigger or smaller, change their color and make them appear dull. In severe cases, central vision is completely blocked out. If it occurs in one eye, the other eye may take over, and the edema is only detected when the good eye is covered.
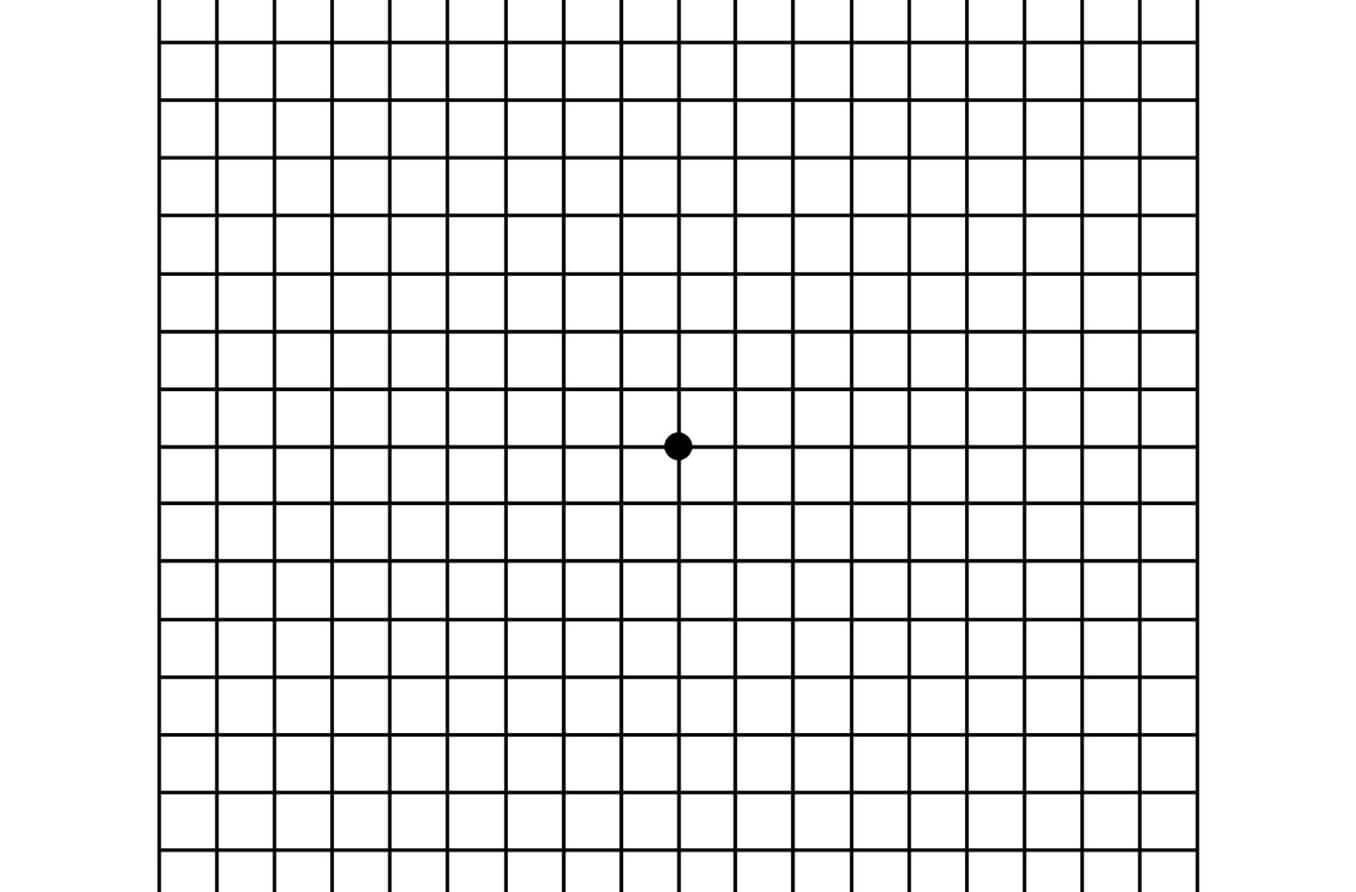
An easy at-home test to detect macular edema is to cover one eye at a time and look at blinds in the windows or the kitchen backsplash — anything with lines in it — making sure that the lines are not wavy or faded in the center. Looking at an Amsler grid is another test that can be viewed on a computer or printed out and viewed once a day.
Causes of macular edema
Macular edema is often caused by leakage of fluid from damaged or abnormal blood vessels in the retina. It can also be caused by leakage of fluid from the layer underneath the retina (the choroid), from the optic nerve (the connection from the eye to the brain), or the gelatinous contents of the eye (the vitreous humor).
Damaged retinal blood vessels in the retina
Certain conditions such as diabetes can damage the lining inside small blood vessels — capillaries — and result in leakage of blood and plasma into the macula.
In other cases, retinal blood vessels can form an outpouching called an aneurysm. Small aneurysms — microaneurysms — are formed when capillaries are damaged from conditions such as diabetes or hypertension. Large aneurysms — macroaneurysms — are generally caused by hypertension. Both types of aneurysms can cause fluid to leak into the macula.
An eye stroke caused by the blockage of a retinal vein can cause blood to back up in the retina and fluid to accumulate in the macula.
Blood vessels that are injured due to inflammation, infection, trauma or exposure to intense light can also cause the macula to become swollen.
SEE RELATED: Diabetes and eyesight: symptoms, treatments and eye exams
Abnormal blood vessels
New blood vessels can grow into the retina from the choroid. This process is called choroidal neovascularization (CNV). CNV can be caused by age-related macular degeneration (AMD), by some infections — such as the fungus Histoplasma — as well as by inflammation, scars, and tumors of the retina and the choroid.
Intraretinal microvascular abnormalities (IRMAs) are small blood vessels in the retina that have adapted to poor circulation by becoming bigger. These are often seen in patients with diabetic retinopathy and increase the risk for macular edema.
There are some diseases of the retina that only affect some people. One example is Coats’ disease. This disease affects young men and causes leaky blood vessels to grow in the retina.
Other diseases that can cause macular edema in a similar way include Sturge-Weber, Von Hippel-Lindau and Wyburn-Mason Syndrome, as well as Idiopathic Juxtafoveal Telangiectasia.
Leakage that comes from the choroid
The choroid contains many blood vessels. A layer at the bottom of the retina — the retinal pigment epithelium (RPE) — keeps fluid out. In a condition called central serous chorioretinopathy, the RPE layer becomes leaky, causing macular edema. This condition will often go away by itself without treatment.
Leakage that comes from the optic nerve.
Very high blood pressure — when the systolic pressure is over 180 or the diastolic over 120 — may cause the optic nerve to leak fluid into the retina. This fluid tends to drain toward the macula in a pattern called a macula star.
Some people have a defect in the optic nerve called an optic disc pit. This may cause fluid to leak into the retina.
Inflammation and a stroke of the optic nerve usually cause swelling of the nerve and the area around it. When enough fluid accumulates, it can settle into the macula.
Pulling on the macula
In up to one-quarter of all people, a clear membrane forms on top of the macula. The membrane — called an epiretinal membrane (ERM) — is often caused by inflammation, age, diabetes or surgery. The ERM can pull on the retina and cause edema.
In other cases, the jelly in the eye — called the vitreous — warps the macula causing edema. This is called vitreomacular traction syndrome (VMTS).
Types of macular edema
There are a few types of macular edema, all of which can be identified and treated by your eye doctor.
Diabetic macular edema (DME)
Fluid builds up due to leaky blood vessels. This type of edema can start outside of the center of the macula before there are any symptoms. This is one reason it is important for anyone with diabetes to regularly be seen by an eye doctor.
Conditions such as a retinal vein occlusion can cause edema that appears very similar to DME and respond to the same treatments.
Cystoid macular edema (CME)
This type of edema is always in the middle of the macula and builds up in small fluid pockets — cysts — that are picked up with special tests done in the eye clinic.
Central serous chorioretinopathy (CSC)
CSC appears in the center of the retina as dome-shaped swelling. It usually does not cause significant vision loss but will cause a lot of distortion, often distorting objects in a “pincushion” fashion.
Macula star
This describes the appearance of dense fluid — exudate — in a star pattern in the center of the macula. This type of macular edema is caused by fluid coming from somewhere at the edge of the macula, such as the optic nerve, or abnormal leaky blood vessels as is the case of macro-aneurysm or Coats’ disease. The thickest part of the star always points toward the source of the fluid.
Risk factors
There are a number of factors that can increase the risk of developing macular edema. These include:
Diabetes
High blood sugar increases the risk of DME, affecting 28% of type 2 and 12% of type 1 diabetics. A measure of the average blood sugar level is the glycosylated hemoglobin A1C (HbA1c) test, which is normal at 5.5%.
Studies have shown that, for an increase by 1% of the HbA1c, the risk of developing macular edema goes up by 1/8.
High blood pressure
Blood pressure is elevated when the systolic measurement is over 120 mm and the diastolic over 80 mm. The higher these two measurements, the higher the risk of hypertensive retinopathy, retinal macroaneurysms, branch retinal vein occlusions and other conditions that cause macular edema.
A systolic over 180 mm or a diastolic over 120 mm is a medical emergency and requires admission to the hospital. At this level of blood pressure, the optic nerve starts to leak fluid causing a macula star.
Stress
Chronic stress is a known cause of high blood pressure. It is also thought to be a cause of central serous chorioretinopathy (CSC).
Surgery
A cause of cystoid macular edema (CME). Pulling on the retina by the vitreous gel, intense light exposure of the macula and the mechanical manipulation of the eye during surgery all increase the risk of edema.
Macular edema after cataract surgery is called Irvine-Gass Syndrome.
Inflammation and infection
Several auto-immune diseases such as sarcoidosis and HLA-B27 diseases, as well as infections of the retina and choroid such as toxoplasmosis.
Age
Several conditions that cause macular edema become more common with age, including wet age-related macular degeneration — a severe cause of macular edema.
Injury
Blunt injury directly to the eye creates a shockwave that can create temporary edema. This type of edema is called Berlin’s edema or commotio retinae. Injury can cause inflammation which results in CME.
Inherited diseases
Retinitis pigmentosa is an inherited disease that causes night blindness and tunnel vision due to a breakdown of retinal cells. It is a cause of CME as well.
Cancer and radiation
Cancer tumors underneath the retina can cause leakage of fluid into the retina. Radiation — usually applied for the treatment of cancer of the head — can damage the retina.
Toxicity
Niacin (Vitamin B3) can cause CME even at lower doses.
Medications
CME: Fingolimod (Gilenya, Novartis Pharmaceutical Corporation) — a medication for multiple sclerosis; epinephrine — used for allergic reactions and in some eyedrops; latanoprost — a glaucoma medication; and others can cause CME.
CSC: Taking prednisone or other steroids increases the risk of CSC.
Macular edema diagnosis
Several tests allow a very accurate diagnosis of the severity and type of macular edema.
Amsler grid
This test involves looking at a grid pattern — usually on a piece of paper — with one eye at a time, to test whether any of the lines are distorted, fuzzy or missing altogether.
Dilated fundus exam (DFE)
A dilated fundus exam allows the eye doctor to look directly at the macula. When macular edema is caused by small amounts of clear fluid, a DFE may not be sensitive enough. However, when thicker fluid — exudate — is present, a DFE will pick it up.
Optical coherence tomography (OCT)
OCT uses light waves to image the layers of the retina and part of the choroid. Edema appears as dark pockets in the retina on this scan.
Fundus fluorescein angiography (FFA)
After injecting a small amount of fluorescein dye into the bloodstream pictures are taken of the retina with a special camera for about 10 minutes. The movement of fluoresceine through the blood vessels in the retina and choroid is then analyzed. This test is very accurate in distinguishing between the different types of macular edema and in finding the cause of the edema.
Macular edema treatment
Treatment can be different for DME, CME and CSC, but several of the same techniques are used for all types of macular edema.
Tight blood sugar and blood pressure control
In the case of DME and macular edema caused by hypertension, prevention as well as reversing the damage can be attained by tightly controlling the following:
Blood sugar levels
Blood pressure
Cholesterol levels
Discontinue the medication or supplement
In many cases, macular edema can be reversed just by stopping the supplements (Niacin) or medications (steroids, Gilenya, latanoprost, epinephrine) that are the cause.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs are taken as eye drops to treat CME and are prescribed after surgery to prevent the start of CME.
Corticosteroids
Steroids are taken as drops, pills and injections on the outside of or into the eye for CME, DME and edema caused by vein occlusions.
Dexamethasone (Ozurdex®) is an FDA-approved medication that is injected into the eye.
Anti-VEGF treatments
Vascular endothelial growth factor (VEGF) is produced by the retina when it is injured. VEGF causes blood vessels to become leaky, causing retinal edema. Two medications are injected into the eye to counteract VEGF:
Aflibercept (Eylea®) is FDA-approved and well-tested.
Bevacizumab (Avastin®) is not FDA approved but is well tested and felt to be safe to use. Medications that are not FDA-approved can still be used by doctors. This is called “off-label use” and is common practice.
Laser treatment
Retinal photocoagulation is when a laser is used to seal off the area where fluid is leaking into the retina.
Vitrectomy and membrane peel
VMTS and ERMs may require surgical removal of the offending tissue.
Vitrectomy is when the vitreous gel is removed from the eye and replaced by a salt solution. Sometimes a gas bubble is placed inside the eye to keep the retina from detaching.
Membrane peel is when the clear cells that formed an extra layer on top of the macula, are surgically removed.
When should I see a doctor?
If you’ve been diagnosed with diabetes or high blood pressure, it is important to have regular comprehensive eye exams to monitor for any eye complications. If you have symptoms of distortion or blurred vision in one or both eyes, it is important to see an eye doctor right away to rule out macular edema or other diseases.
Dietary and lifestyle changes and good blood sugar pressure management are essential parts of protecting your long-term eye health.
Macular edema. StatPearls. October 2022.
Retinal macroaneurysm. StatPearls. November 2022.
What are choroidal neovascular membranes? American Academy of Ophthalmology. September 2022.
What is central serous chorioretinopathy? American Academy of Ophthalmology. September 2022.
Optic ischemia. StatPearls. July 2022.
Vitreomacular traction syndrome. EyeWiki. American Academy of Ophthalmology. October 2022.
Neuroretinitis. EyeWiki. American Academy of Ophthalmology. August 2018.
Commotio retinae. EyeWiki. American Academy of Ophthalmology. October 2022.
Drug Induced maculopathy. EyeWiki. American Academy of Ophthalmology. November 2022.
Fingolimod-associated maculopathy. EyeWiki. American Academy of Ophthalmology. January 2023.
Optical coherence tomography angiography. StatPearls. September 2022.
Fluorescein angiography. StatPearls. November 2022.
Pseudophakic cystoid macular edema (Irvine-Gass syndrome). EyeWiki. American Academy of Ophthalmology. December 2022.
What is vitrectomy? American Academy of Ophthalmology. September 2022.
Page published on Tuesday, March 7, 2023
Page updated on Tuesday, March 14, 2023