Papilledema (optic nerve swelling)
When a doctor diagnoses papilledema, or optic nerve swelling, it means fluid is pressing on the nerves that transmit visual information to the brain. Papilledema can affect your vision but it also might mean something’s going wrong deep inside your brain.
This raises a number of questions:
How serious is papilledema?
What are the symptoms and causes of papilledema?
Does optic nerve swelling cause blindness?
How does a doctor diagnose and treat the condition?
But first, the basics:
What is papilledema?
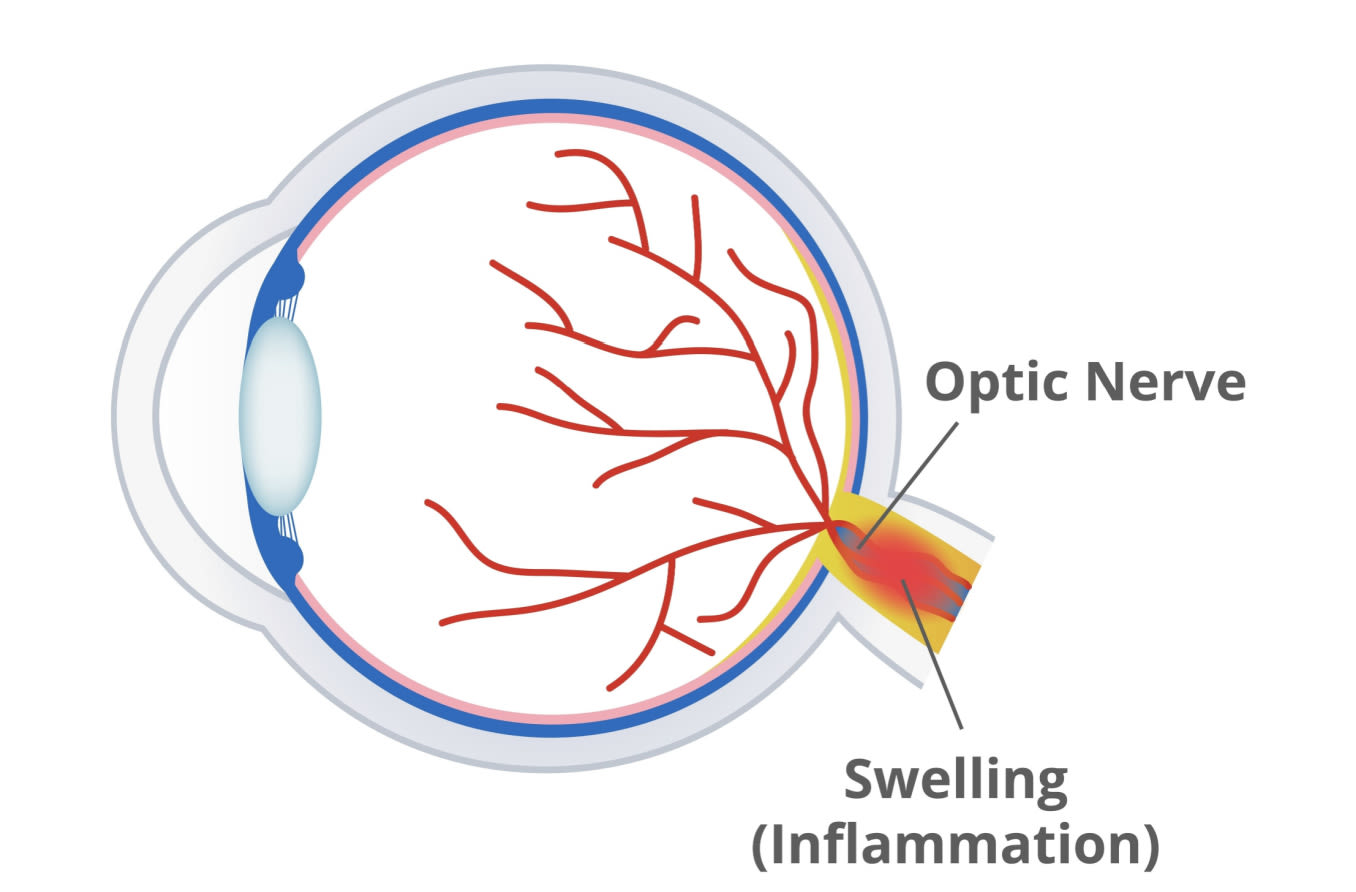
The word papilledema has two parts: “papill” refers to the optic disc, which connects the eye to the optic nerve; and “edema,” which refers to swelling caused by excess fluids in body tissue.
Thus, papilledema (pronounced PAH-pil uh-deema) is an excess of fluid that causes swelling of the optical disc.
Though excess fluid can cause swelling in many areas along the optic nerve, papilledema means the swelling is happening specifically at the optical disc. Because swollen optic nerves contribute directly to papilledema, it’s useful to talk about both issues together.
How serious is optic nerve swelling?
Each of your eyes connects to an optic nerve made up of fibers that need to stay at about the same size all the time to do their job correctly. Issues occur when swelling from fluids (edema) changes the size of these nerves, which isn’t supposed to happen. But just how bad is it?
Doctors know papilledema can point to all sorts of problems, so they look for it along with other symptoms related to eyesight and the brain. It could be something as trivial as a headache or as frightening as a brain tumor.
Thus, papilledema is not a disease; it’s a symptom (or condition) that can point to other problems and/or help a doctor confirm a diagnosis. It’s not necessarily bad or good — it’s a clue that should not be ignored.
How does papilledema work?
Let’s start with the basics of human vision: In the eyeball, light-sensitive nerves in the retina transmit visual information to the brain. The brain’s vision center translates these signals into images that let you see and understand the world around you.
The key visual pathway is the optic nerve, which runs from the optic disc at the rear of the eyeball to the visual cortex on the back side of the brain. The visual cortex has two parts: the left cortex, which processes visual information for your right eye; and the right cortex, which pairs with your left eye.
The two optic nerves pass through the middle of the brain, which can be a bit tricky for vision because the brain floats in a fluid that protects it from bashing into the hard shell of the skull (or cranium). This fluid also surrounds and protects the optic nerves.
When fluid levels in the brain rise, they can put the squeeze on everything, including the optic nerves, because there’s only so much room inside your cranium.
And anything that changes the size of tissue or the volume of fluids inside the skull can press on the optic nerves. This pressure causes a kind of swelling of the optic disc — that section at the back of the eye where visual signals must pass to reach the optic nerve.
With papilledema, excess liquids in the skull or spine (technically known as cerebrospinal fluid) interfere with the optic disc’s ability to transmit visual information. Extra fluid also suggests changes in the brain that could mean something as serious as a brain tumor.
That’s why it’s wise to pay close attention to the symptoms of papilledema.
Papilledema symptoms
The most common symptoms of papilledema include:
Nausea and vomiting. Pressure on your optic nerves can trip up your sense of balance and make you sick to your stomach, possibly even causing you to throw up.
Hearing changes. Ringing sounds or mechanical noises may point to papilledema.
Headaches. Changes in brain fluid levels may cause physical pain.
Vision changes. Optic nerve swelling may lead to double vision or blurred eyesight. Some people feel like their vision is going gray or black for a short time, and standing up too fast or coughing might cause temporary blackouts.
Only around 25% of people with severe papilledema experience vision problems, highlighting the reality that optic nerve issues don’t have to degrade vision to suggest problems in the brain.
Does papilledema cause blindness?
Papilledema can lead to blindness if left untreated for a long time. This underscores the importance of getting treatment for papilledema-related problems as soon as possible, before they lead to permanent damage.
Papilledema causes
Papilledema is commonly caused by:
Head trauma. Impacts on the skull can press on brain tissues, causing optic nerve swelling at the optic disc.
Brain tumors. A tumor growing in the brain can press on nearby nerves and tissues.
Brain bleeding. A stroke or some other damage to blood vessels can change the fluid volume of the skull.
Infection. Bacteria (such as from Lyme disease), viruses and other pathogens can cause swelling and increase cerebrospinal fluid. Encephalitis and meningitis are two of the more well-known infections.
High blood pressure. Occasionally, elevated blood pressure (hypertension) adds to the pressure inside the brain.
Idiopathic intracranial hypertension (IIH). This form of optic nerve swelling is what doctors call idiopathic, which means science does not really understand the cause — it just acknowledges the effects. IIH may occur in young women because of hormonal changes, but the science is not totally clear on all of its causes.
How do doctors diagnose papilledema?
Eye doctors use a tool called an ophthalmoscope to peer inside the eyeball and check for signs of a swollen optic nerve. When they look at the optic nerve disc, it may show abnormalities caused by higher-than-normal liquid pressure inside the cranium.
Once an eye doctor sees evidence of optic nerve swelling, they start analyzing your symptoms to figure out what to do next. You may have to get an MRI to see if a neurological problem, such as a brain tumor, is the culprit.
This analysis sets the stage for treating papilledema.
Papilledema treatment
As with many conditions, determining papilledema treatment — specifically, how to reduce liquid pressure on the optic disc — depends on the underlying cause. If there’s a brain tumor, surgery may be required to ease the pressure and/or install a shunt to reroute fluid away from the optic nerves.
If the problem is idiopathic intracranial hypertension, doctors may prescribe medication such as acetazolamide (Diamox) to decrease production of cerebrospinal fluids, or opt for a therapeutic spinal tap (lumbar puncture) to drain excess cerebrospinal fluids. If a person’s weight or medications are thought to be contributing factors, a doctor may recommend that a patient lose weight or stop taking any problematic medications.
In rare cases, and after other treatment options have failed, surgery may be recommended if an IIH patient’s vision is severely threatened. A procedure called optic nerve sheath fenestration (ONSF) may be considered, but there’s some controversy about whether ONSF is the best choice.
If an infection is causing the papilledema, then doctors will likely prescribe medications such as antibiotics or antivirals.
Optic neuritis vs. papilledema
Optic neuritis, another condition that may afflict the optic nerve, is caused by optic nerve inflammation rather than fluid pressure. It has more direct impact on vision than papilledema typically does, with symptoms including pain, vision loss in a single eye, and loss of color vision and field of vision.
Optic neuritis may be a precursor to multiple sclerosis (MS). Because optic neuritis is so much different than papilledema, it’s crucial to get the proper diagnosis and the right treatment.
Always take the risks of papilledema seriously
Papilledema means fluid pressure is disrupting the function of your optic disc, the key junction between the retina and the brain’s vision processing centers. These malfunctions might not cause problems with your vision, but they could point to a severe problem like a brain tumor.
If you’re experiencing symptoms outlined above, or if you notice any dramatic changes in your vision, contact your eye doctor as soon as possible to find out what’s going on.
READ NEXT: Drusen in the eye: An overview
Page published on Thursday, January 14, 2021






