Phthisis bulbi
What is phthisis bulbi (end-stage eye condition)?
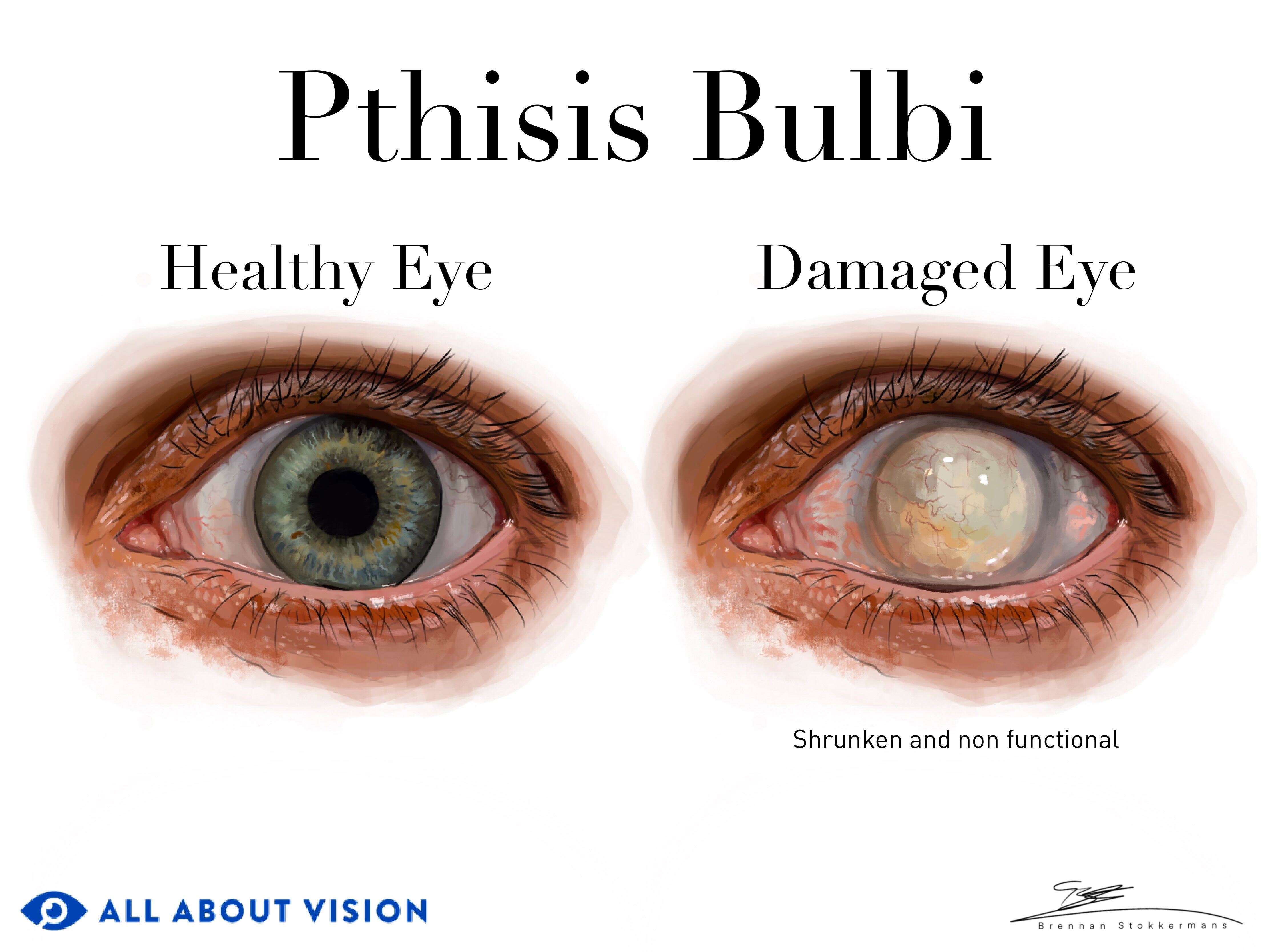
Phthisis bulbi occurs when damage to the eye causes it to completely stop working. The affected eye will typically become smaller and more square in shape. It may also look sunken in or take on a cloudy appearance.
Phthisis bulbi results in the permanent loss of vision and motor control in the eye, but sometimes vision loss from a disease causes phthisis bulbi.
The name of the condition comes from the Greek word for “shrinkage,” which is phthiein. It is also referred to as “end-stage eye.”
Causes of eye shrinking
Eye shrinkage is one of the most notable signs of phthisis bulbi. This shrinkage is largely due to three primary factors:
Low intraocular pressure
Intraocular pressure refers to the amount of force aqueous humor is exerting inside the eye. Aqueous humor is a clear liquid that nourishes the eye and helps maintain its shape. It enters and exits the front of the eye in equal amounts to keep eye pressure consistent.
A healthy level of intraocular pressure is critical for maintaining the eye’s health and its ability to function. When intraocular pressure is too low, a condition called hypotony can develop. Hypotony can alter the levels of oxygen and nutrients feeding the eye, leading to shrinkage.
Disruption of the blood-eye barrier
The blood-ocular barrier helps prevent blood plasma from entering the aqueous humor. Plasma is the liquid foundation that carries blood cells throughout the body. One of its main solid components is protein. The aqueous humor typically contains no proteins, which helps keep a clear pathway for light through the vision system.
The blood-ocular barrier helps keep the proteins in plasma out of the aqueous humor. If this barrier becomes disrupted and proteins enter the aqueous, damage to the eye may occur. This could also lead to eye shrinkage.
Intraocular inflammation
Another major component of eye shrinkage is inflammation. Inflammation is a process in which the body sends cells to attack something it sees as a threat (like bacteria, a virus or an autoimmune disease). Long-term inflammation in the eye can cause scarring and the growth of fibrous tissue (fibrosis). These factors may lead to damage that results in phthisis bulbi.
Other causes
A number of other issues can lead to phthisis bulbi, including:
Physical trauma to the eye
Infection
Birth defects
Radiation therapy
Chronic retinal detachment
Sickle cell disease
Persistent hyperplastic primary vitreous (a congenital condition where the eye forms improperly as the fetus develops)
The inflammation associated with certain autoimmune disorders can also trigger phthisis bulbi.
Most cases of phthisis bulbi occur in those between 65-85 years of age. This could be because people in this age group are more likely to have health concerns that can lead to eye damage. When the condition occurs in younger individuals, it may stem from birth defects or physical trauma. Regardless of the root cause, phthisis bulbi can impact individuals of any age.
SEE RELATED: Osteo-Odonto Keratoprosthesis Surgery (OOKP)
Symptoms of an end-stage eye
Phthisis bulbi can present with a variety of symptoms, including eye irritation, eye pain and vision loss. Other symptoms may include:
Photophobia (light sensitivity)
Some patients may be asymptomatic or have no noticeable symptoms.
Clinical signs
There are certain physical signs a physician can use to help diagnose phthisis bulbi. Along with shrinkage, the eye often develops a thickened sclera (the white of the eye). It is also common for dystrophic calcification to occur in parts of the eye. This refers to a process in which calcium builds up in damaged or dead tissue.
Ossification in the eye, or the formation of bone, is another possible sign of phthisis bulbi. This means that bone is forming in a place where it shouldn’t be, which can cause functionality issues.
Other clinical signs may include:
Swelling
Strabismus (crossed or misaligned eyes)
Cataracts
Droopy eyelid (a secondary effect from the shrunken eye, allowing the upper lid to drop lower)
Diagnosis
A diagnosis of phthisis bulbi is typically determined through an eye exam. Your eye doctor will examine your entire eye, inside and out. If they discover signs like damage or scarring, they may order an MRI or a CT scan for a closer look.
Treatment options for phthisis bulbi
During the early stages of phthisis bulbi, a topical steroid or cycloplegic eye drops may help with relieving symptoms. However, this will not prevent eventual vision loss.
Once an eye has developed phthisis bulbi, the damage is usually permanent. Unfortunately, there are no treatments that can bring vision back. However, enucleation (removal of the eye) or the implantation of a prosthetic eye are potential ways to address its effects. Neither option will enable vision, but they can be helpful for pain relief and cosmetic purposes.
SEE RELATED: Eye implants: Bionic eyes, lenses and prosthetic eyes
Preventing eye deflation
Prevention for phthisis bulbi is focused on effective treatment for potential underlying causes. If you are aware of an autoimmune disorder, injury or other condition that can lead to end-stage eye, it is critical to maintain regular eye exams. An eye doctor can monitor inflammation, scarring, intraocular pressure and other factors that may indicate signs of phthisis bulbi.
If you are involved in a sport or other activity that can lead to physical trauma, make sure to wear appropriate eye protection. This may help lower the risk of developing the condition.
When to see an eye doctor
If you begin to notice any pain, blurred vision, light sensitivity or other vision changes, seek advice from an eye doctor right away. This is especially important if you have any underlying conditions or previous eye injuries that can lead to phthisis bulbi. Maintaining annual eye exams is also important for your overall eye health.
READ NEXT: Rare eye diseases: What causes them and how are they treated?
Phthisis bulbi (end-stage eye). Cleveland Clinic. August 2022.
Phthisis bulbi. EyeWiki. American Academy of Ophthalmology. October 2023.
Intraocular pressure. StatPearls [Internet]. July 2022.
Aqueous humor & vitreous humor. Cleveland Clinic. December 2022.
Dynamics of the aqueous humor. Chapter 9: Aqueous humor, iris, and ciliary body. In Basic and Clinical Science Course, Section 02: Fundamentals and Principles of Ophthalmology. 2020 – 2021.
Physiology, blood plasma. StatPearls [Internet]. April 2023.
Phthisis bulbi. Global Radiology CME. April 2021.
Inflammation. Cleveland Clinic. December 2023.
Dystrophic calcification of the lower leg in a patient with chronic lower extremity venous insufficiency and diabetes mellitus: A case report and literature review. Advances in Skin & Wound Care. January 2023.
Embryology, bone ossification. StatPearls [Internet]. May 2023.
Heterotopic ossification. StatPearls [Internet]. July 2023.
Page published on Thursday, April 25, 2024
Page updated on Tuesday, April 30, 2024
Medically reviewed on Monday, April 22, 2024






