Posterior vitreous detachment
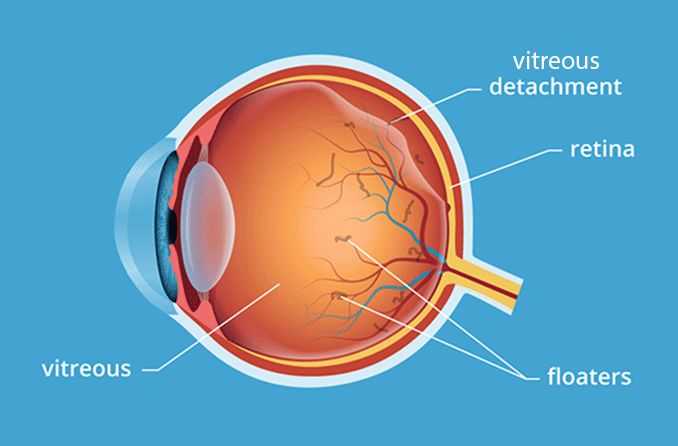
Posterior vitreous detachment is separation of the normally clear, gel-like fluid (vitreous humor) that fills the back of the eye from its normal attachments to the retina. Though vitreous detachment is considered a normal aging change, it sometimes can lead to serious eye problems.
Conditions and problems associated with posterior vitreous detachment include:
Vitreous detachment symptoms
The primary symptoms of posterior vitreous detachment are eye floaters and flashes of light. These symptoms typically occur suddenly and can persist for days.
In most cases, floaters and flashes associated with vitreous detachment occur in older adults. But it’s possible for them to occur at any age.
Eye floaters
The vitreous is a clear substance within the eye that gives it its shape — like water in a water balloon. Though it is mostly water, the vitreous also contains tiny fibers of a protein called collagen, which gives it a jelly-like consistency. Early in life, the collagen fibers in the vitreous are arranged in a tidy, organized fashion, making them essentially invisible.
As we age, the gel-like vitreous begins to liquify. This causes collagen fibers in the vitreous to clump together in an unordered fashion and become opaque. The opaque clumps cast shadows on the retina when light enters the eye, and our brain interprets these shadows as floaters.
While research has yet to give a definite reason behind why the vitreous liquefies, it’s confirmed that it results in the appearance of floaters.
Eye flashes
The vitreous has more collagen fibers where it attaches directly to the retina, making this part of the vitreous “thicker” than the central portion.
When the center of the vitreous liquefies with age, the thicker portion in the periphery begins to pull away from its attachment to the retina, resulting in a posterior vitreous detachment.
As the vitreous tugs on the retina, it triggers flashes or streaks of light in your peripheral vision. These flashes often are the first symptoms of a posterior vitreous detachment (PVD).
Though a few flashes and floaters from a vitreous detachment usually are no cause for alarm, if you notice the number of floaters or the frequency of flashes increasing, you should see an eye doctor promptly.
Only an eye doctor can make sure these vitreous detachment symptoms are not indications of a more serious condition — such as a retinal tear or detachment of the retina.
SEE RELATED: Types of retinal detachment
Causes of posterior vitreous detachment
In most cases, posterior vitreous detachment is caused by normal aging changes in the eye.
With time, the vitreous contracts or shrinks, and also becomes less like a gel and more like a liquid (a process called vitreous syneresis). When this occurs, the vitreous and collagen fibers within it, pull away from and eventually detach from the retina.
Other causes of PVD include:
Nearsightedness (especially high myopia)
Inflammation of the retina
SEE RELATED: Is it normal for young people with myopia to have eye floaters?
Diagnosis
Posterior vitreous detachment is diagnosed through a comprehensive eye exam. In order to see the retina more clearly, your eye doctor will use special eye drops to dilate your pupils. Using a microscope to look at the front of your eyes, your doctor will be able to check for signs of vitreous detachment, as well as signs of other eye conditions.
Some cases of PVD may be mild enough to go without treatment. However, if there are signs of more serious retina problems, they may need to be treated immediately. Whatever the case, it is important to have vitreous detachment reevaluated during each regular eye exam to make sure no further problems have occurred.
Vitreous detachment treatment
Posterior vitreous detachment typically does not require extensive treatment, and floaters or flashes that occur with PVD fade or become less noticeable over time. It is important, however, to have regular eye exams in case another condition has developed.
Severe floaters may be recommended to be treated with a laser procedure called laser vitreolysis. This is an in-office procedure that involves an ophthalmologist aiming a laser at large floaters in the eye (through the pupil) to break them up.
Laser vitreolysis is recommended for patients whose floaters are large and far away from the retina.
If a serious eye condition has developed due to vitreous detachment, such as a retinal tear, retinal detachment or macular hole, a specific treatment will be needed for whichever particular condition has been diagnosed.
Does posterior vitreous detachment affect vision?
According to the American Society of Retina Specialists, if posterior vitreous detachment occurs gently, gradually and uniformly, symptoms like floaters and flashes are typically mild. However, it is possible for the vitreous to pull too hard on the retina and create a retinal hole or retinal detachment.
Retinal detachment occurs when a piece of the retina is lifted or pulled from its attachment to the back of the eye. It’s possible for this to take place after a PVD, which is why a visit to the eye doctor is recommended when frequent flashes of light occur in your vision.
Columbia University’s Department of Ophthalmology compares it to a stamp being peeled off an envelope. There are times when the stamp is removed cleanly, and other times when pieces of the envelope are pulled off with the stamp.
Posterior vitreous detachment usually is a common occurrence that does not threaten your sight. But a retinal detachment is a medical emergency that can jeopardize your vision if treatment isn’t administered quickly.
It’s important when you start seeing symptoms of PVD, to make an appointment with your eye doctor as soon as possible. They can take a look at the vitreous, as well as the retina, to determine whether the risk of retinal damage is present.
READ MORE: Detached retina symptoms and warning signs
Page published on Tuesday, October 27, 2020






