Pseudoexfoliation syndrome and pseudoexfoliation glaucoma: Causes, symptoms and treatment
What is pseudoexfoliation syndrome?
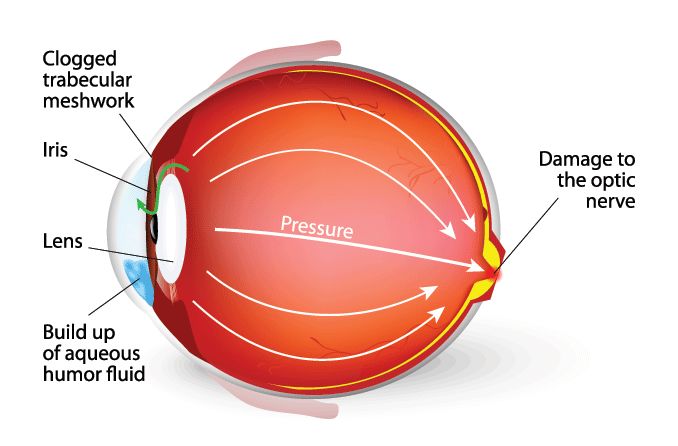
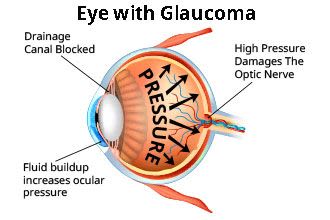
Pseudoexfoliation syndrome is when tiny clumps of protein fibers form in and around the body, including in the front of the eye. These clumps, that look like dandruff flakes, can clog the eye’s drainage area and raise eye pressure, eventually leading to glaucoma, cataracts and possible vision loss.
While they are only harmful in the eyes, the flakes can also build up in the lungs, skin, heart and kidneys. Pseudoexfoliation syndrome (also called PXF, PXE or PEF) involves these parts of the eye:
Aqueous humor. The clear, watery fluid in the front of the eye that provides the eye with nourishment, removes waste, and maintains normal eye shape and pressure
Ciliary body. Holds the natural lens in place behind the pupil, enables accommodation of the eyes and produces aqueous fluid
Cornea. The clear outer part at the front of the eye that focuses the light allowed in by the pupil
Iris. The colored part of the eye that adjusts the size of the pupil to control how much light reaches the back of the eye
Lens. The clear part of the eye behind the iris that allows the eye to focus on objects close up and far away
Pupil. The opening at the center of the iris that lets light enter the eye
Trabecular meshwork. Porous, spongy tissue within the drainage angle of the eye; fluid exits the eye here
Pseudoexfoliation [Image credit: Permission granted by © 2022 American Academy of Ophthalmology]
Here’s how pseudoexfoliation occurs within the eye:
As your pupil contracts and expands, the iris may brush over and against the lens.
This brushing can rub very small flakes off of the lens.
These flakes collect mostly in the front of the eye: on the lens, along the edges of the pupil, between the cornea and iris, and in the trabecular meshwork.
What is pseudoexfoliation glaucoma?
Pseudoexfoliation glaucoma happens when the dandruff-like flakes caused by pseudoexfoliation syndrome clog the trabecular meshwork, raising the eye pressure and damaging the optic nerve.
Pseudoexfoliation glaucoma is a form of secondary glaucoma, which means it results from another (existing) condition. In fact, pseudoexfoliation syndrome (PXF) is the most common cause of secondary open-angle glaucoma. PFX has also been linked to higher rates of chronic angle-closure glaucoma.
When compared with primary open-angle glaucoma (POAG), patients with pseudoexfoliative glaucoma tend to experience:
Earlier presentation of the condition (and more ocular damage at time of diagnosis)
Higher intraocular pressure (IOP) with greater fluctuation, making IOP harder to control
Greater visual field loss
More damage to the optic nerve
Faster progression of the disease
Having pseudoexfoliation syndrome is not a guarantee that you will develop pseudoexfoliative glaucoma, but it is a major risk factor. It’s estimated that 40% to 50% of patients who have PXF will eventually have glaucoma.
What causes pseudoexfoliation?
While the exact cause of pseudoexfoliation syndrome is unknown, certain risk factors can make a person more likely to develop the condition.
Non-environmental risk factors for developing PXF include:
Family history. Having a relative with the condition and/or having a twin makes it more likely that you will be diagnosed with PFX.
Genetic predisposition. People with mutations in the LOXL1 gene are at a higher risk for developing both PFX and PFX-related glaucoma. However, it’s a common mutation and most people who have it don’t get pseudoexfoliation.
Race. Having Northern European ancestry, specifically Scandinavian descent, increases your chances of developing PXF.
Age. People who are 70 or older are at a higher risk. PXF is rarely diagnosed in people under 50.
Environmental risk factors for developing pseudoexfoliation syndrome include:
Sunlight. Excess exposure to sunlight (UV radiation) — as can happen with those who work outside or spend a lot of time outdoors over the course of their lifetime — can lead to a higher risk of getting PXF.
Location. The number of PXF cases increases the farther north people live in the world. More cases also tend to occur in places that are colder year-round, such as Iceland, Sweden and Norway.
Diet. Not getting enough folate (vitamin B9) and drinking too much caffeinated coffee (more than three cups a day) have been found to increase a person’s risk of getting pseudoexfoliation syndrome.
Additionally, PXF is more common in women than men.
More research is needed to learn how genetic and environmental factors affect a person’s chances of developing pseudoexfoliation syndrome and/or pseudoexfoliation glaucoma.
What are the symptoms of pseudoexfoliation?
Pseudoexfoliation syndrome does not have any noticeable symptoms. During a comprehensive eye exam, your eye doctor should be able to see any PXF-related protein build-up on the lens, around the pupil and elsewhere inside the eye.
Pseudoexfoliative glaucoma can develop when the PXF build-up clogs the trabecular meshwork. This clogging of the system can:
Increase the intraocular pressure
Damage the optic nerve
These are all signs your eye doctor should check for in your annual exams. However, once glaucoma reaches an advanced stage, it can lead to permanent vision loss, one of the few noticeable yet painless symptoms of the condition.
Pseudoexfoliation and cataracts
Pseudoexfoliation syndrome makes a person more likely to develop cataracts, and can make existing cataracts worse. A cataract is a clouding of the eye's lens that makes it difficult to see clearly and comfortably.
PXF also makes cataract surgery more difficult. When the flakes build up on the ciliary zonules that hold the eye’s lens in place, the zonules get weaker and can cause complications during surgery.
How is pseudoexfoliation treated?
Because PXF itself doesn’t cause damage (rather, it sets the stage for other conditions), its progress is monitored rather than treated directly. Once diagnosed, you should see your eye doctor at least once a year to check the health of your eyes and assess your current risk of developing pseudoexfoliative glaucoma and other eye conditions. The earlier glaucoma is detected, the better your chances of preserving your vision.
How is pseudoexfoliation glaucoma treated?
The first step to treating any form of glaucoma, including pseudoexfoliation glaucoma, is to lower your eye pressure. This helps prevent further damage to the optic nerve.
Treatment may include:
Eye drops. Doctors commonly prescribe eye drops to normalize eye pressure, reduce the amount of fluid produced in the eye and/or help fluid flow out of the eye more easily.
Laser surgery. Laser trabeculoplasty is a surgical procedure used to treat PFX glaucoma when eye drops don’t lower the IOP enough (or if they cause significant side effects). Laser treatment also helps drain more fluid from the eye.
Filtering surgery. When eye drops and laser surgery don’t work, a patient may need filtering surgery, also called incisional surgery. A new tiny drainage hole is made in the eye to allow fluid to flow out. This helps lower IOP and prevents or reduces damage to the optic nerve.
If you’re at higher risk for developing pseudoexfoliation syndrome or pseudoexfoliative glaucoma, or you’ve already been diagnosed, make sure to see your eye doctor at least once a year for a comprehensive eye exam so they can monitor you for any signs of disease (or progression).
Pseudoexfoliation (PXE) syndrome and pseudoexfoliation glaucoma. BrightFocus Foundation. July 2021.
What is pseudoexfoliation syndrome? American Academy of Ophthalmology. March 2021.
Ophthalmologists explore causes, consequences of pseudoexfoliation syndrome. Healio. June 2016.
What is exfoliative glaucoma? Glaucoma Research Foundation. June 2021.
Pseudoexfoliation syndrome. Kellogg Eye Center University of Michigan Health System. November 2014.
Is pseudoexfoliation syndrome inherited? A review of genetic and nongenetic factors and a new observation. Ophthalmic Genetics. June 1998.
Glaucoma genetics in 2009. Glaucoma Today. May/June 2009.
Pseudoexfoliation risk and symptoms. American Academy of Ophthalmology. March 2021.
Diagnosis and management of pseudoexfoliation glaucoma. American Academy of Ophthalmology. June 2006.
Pseudoexfoliation syndrome, a systemic disorder with ocular manifestations. Human Genomics. October 2012.
Exfoliation syndrome: a disease with an environmental component. Current Opinion in Ophthalmology. March 2015.
The relationship between caffeine and coffee consumption and exfoliation glaucoma or glaucoma suspect: a prospective study in two cohorts. Investigative Ophthalmology and Visual Science. September 2012.
Is pseudoexfoliation syndrome inherited? A review of genetic and nongenetic factors and a new observation.Ophthalmic Genetics. December 1998.
Pseudoexfoliation syndrome. American Academy of Ophthalmology. January 2022.
Selective laser trabeculoplasty: 10 commonly asked questions. Glaucoma Research Foundation. October 2020.
Incisional surgery. Glaucoma Research Foundation. January 2017.
Page published on Friday, April 8, 2022
Medically reviewed on Tuesday, March 15, 2022






