Cranial nerve palsy – CN III, IV, VI & VII palsy
What is cranial nerve palsy?
Cranial nerve palsy occurs when one of the 12 pairs of nerves that lead from the brain to the face, head or torso loses function. A loss of function of the cranial nerves to the eyes and face can cause symptoms such as weakness, limited movement, double vision, droopy eyelid or a dilated pupil.
Cranial nerves (CN) carry signals between the brain and the rest of the body. CN III, IV and VI control the muscles that move the eyes — the extraocular muscles. Cranial nerve VII controls the muscles of facial expression. These are motor nerves, which means they carry signals to the muscles and glands of the eyes. They innervate them.

Each cranial nerve pair innervates the left and right sides of the face. In the majority of cases, one eye or side of the face is affected by cranial nerve palsy. Cranial nerves III, IV, VI and VII innervate the eye. Palsy of these cranial nerves can result in eye misalignment or strabismus.
Cranial nerve II, the optic nerve, is also involved with the eye, but damage to it is not considered a palsy. This is because it is a sensory nerve rather than a motor nerve. It is composed of more than one million nerve fibers that transmit light signals from the eye to the brain. Damage to the optic nerve — optic atrophy — can lead to blurry or dim vision, side vision loss and altered color vision.
Third cranial nerve (oculomotor)
The third cranial nerve is also known as the oculomotor nerve. Cranial nerve III controls the majority of the extraocular muscles.
Eye function
The oculomotor nerve has two major parts: nerve fibers on the inside and nerve fibers on the outside.
Inner nerve fiber function
CN III controls four muscles that move the eyeball up, down and in, and the muscle that lifts the upper eyelid. The nerve fibers that supply these muscles run on the inside of the nerve.
These muscles are the:
Superior rectus – moves the eye up.
Inferior rectus – moves the eye down.
Medial rectus – moves the eye in.
Inferior oblique – moves the eye up when the eye is looking in toward the nose.
Levator palpebrae superioris – lifts the upper eyelid.
Conditions compromising blood flow to the inner nerve fibers controlling these muscles — without compressing the outer fibers — don’t affect the pupil.
Outer nerve fiber function
The outer fibers of CN III supply two additional muscles that are part of the parasympathetic nervous system, which controls functions when the body is in a resting state.
These muscles are the:
Sphincter pupillae – located in the iris and makes the pupil smaller.
Ciliary muscle – causes the lens to change shape when focusing up close.
Conditions that compress the outer nerve fibers will affect the pupil in third cranial nerve palsy.
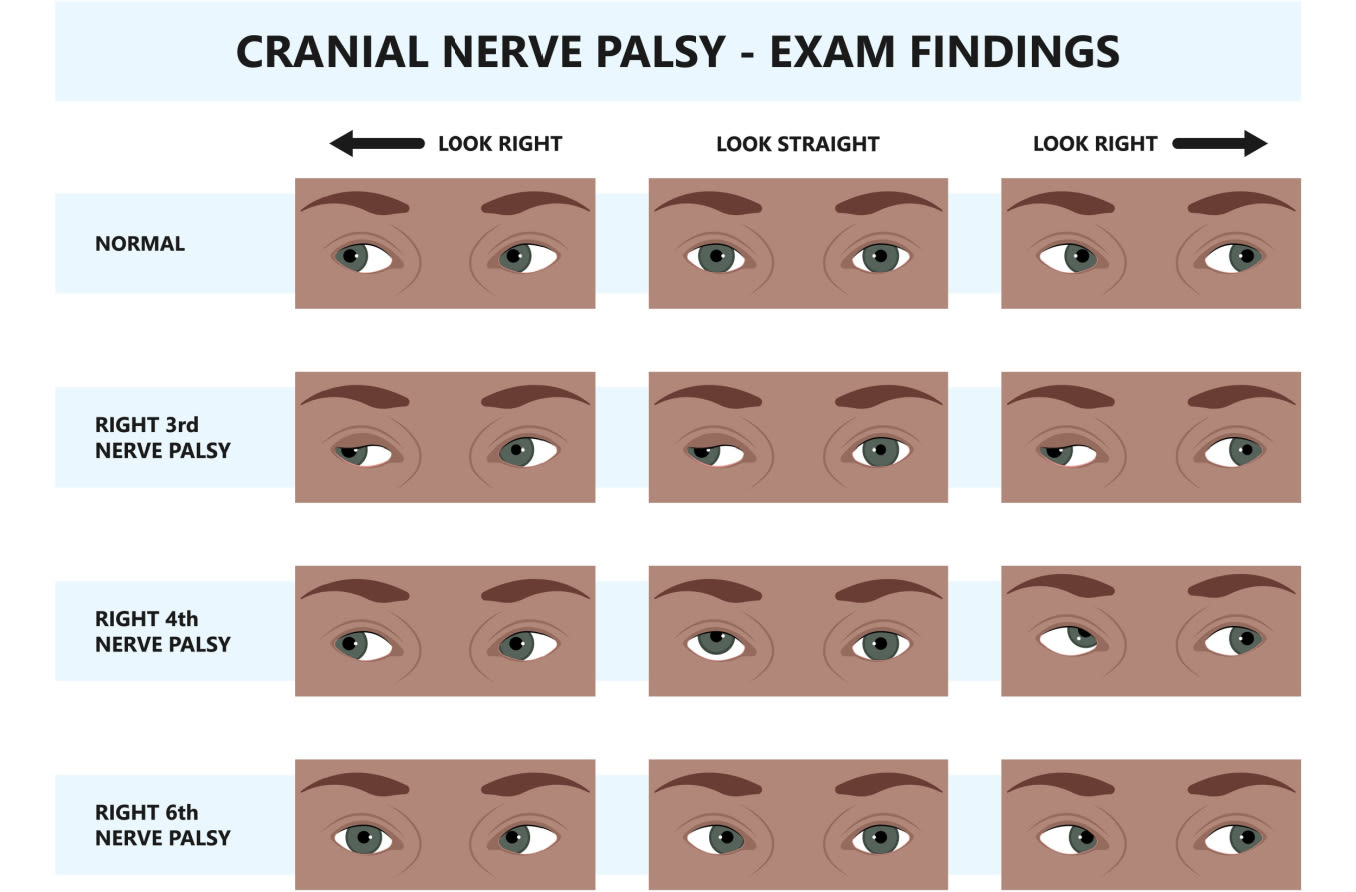
Symptoms of CN III palsy
The following are the signs and symptoms of CN III palsy:
Down-and-out gaze – This occurs because the muscles that pull the eyes in the down-and-out gaze are no longer opposed by CN III. The outward drift of the eyes is called exotropia.
Double vision – The eyes will see double (diplopia) because they no longer align. The affected eye sees an image from a down-and-out gaze, while the other eye looks straight ahead and sees a different image.
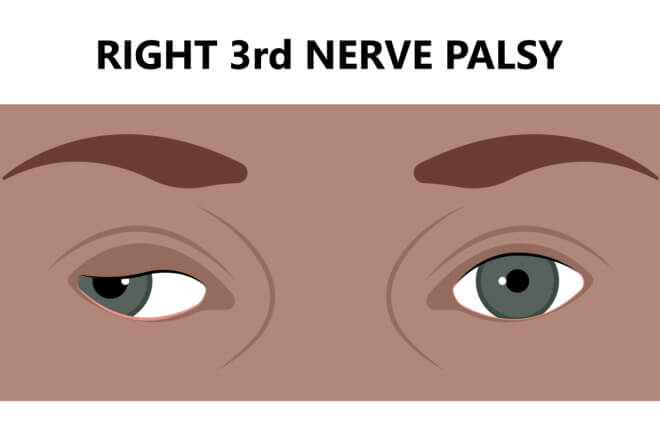
Droopy eyelid (ptosis) – The eyelid droops because the muscle that lifts the upper eyelid is controlled by CN III, which is not functioning.
Dilated pupil – This occurs because the outer fibers of CN III cannot send signals to the sphincter pupilae muscle, which makes the pupil smaller. This is sometimes called a “blown pupil.”
CN III palsy can be partial and only present with some of these signs. Depending on the underlying cause, additional symptoms, such as headache or drowsiness, may also occur.
If someone is experiencing these symptoms, particularly a blown pupil, they should seek immediate medical care as it could indicate an aneurysm — a life-threatening condition.
SEE RELATED: Synkinesis
Causes of CN III palsy
Some individuals are born with a third nerve palsy (congenital). It can also occur due to injury or disease. Whether the pupil is involved depends on the underlying cause.
Third nerve palsy with pupil involvement
Third nerve palsy involves the pupil — a “blown pupil” — when the outer fibers of CN III are compressed. This is a medical emergency.
Conditions that compress the outer fibers of CN III include:
Aneurysm.
Increased pressure in the skull that shifts brain tissue. This herniation is often due to injury, stroke, bleeding, tumor or swelling.
Meningitis that affects the brain stem (for example, due to tuberculosis).
Third nerve palsy that spares the pupil
In some conditions, the small blood vessels that supply the nerve become damaged and limit blood flow to the inner fibers. The outer fibers that innervate the pupil are spared.
This results in third nerve palsy that does not involve the pupil and is usually caused by:
Diabetes.
High blood pressure.
READ MORE: 15 ways heart disease affects eye health
Treatment of CN III palsy
Since many different conditions can lead to a third nerve palsy, treatment involves managing the underlying condition. A clinical exam and imaging, such as a CT or MRI, are needed to diagnose the cause of third cranial nerve palsy.
When the cause is not a medical emergency, an eye doctor may observe for a few months before treatment because symptoms can improve on their own. Eyeglasses with prism lenses can be prescribed to correct double vision. Surgery may be performed to align the eyes and lift the lids if symptoms persist for more than six months.
Fourth cranial nerve (trochlear)
The fourth cranial nerve is also known as the trochlear nerve. It is named after the Latin word “trochleae,” meaning pulley.
Eye function
The trochlear nerve controls the superior oblique muscle, which helps with down gaze and eye rotation when the head is tilted.
Symptoms of CN IV palsy
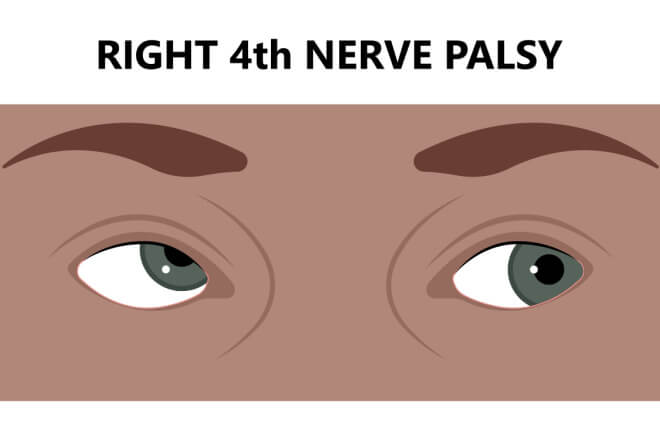
Double vision, in which objects are split vertically, is a common symptom of CN IV palsy.
Other signs and symptoms include:
Turning up of the affected eye
Inability to gaze down and inward
Head tilt to compensate for double vision
Causes of CN IV palsy
Some individuals are born with a fourth nerve palsy (congenital). It can also be acquired due to the following:
Head injury
Diabetes
Inflammation
Tumor
Idiopathic (cause unknown)
Treatment of CN IV palsy
In many cases, a fourth cranial nerve palsy becomes better on its own after several months. Since many different conditions can lead to this type of palsy, treatment involves managing the underlying condition. A clinical exam and imaging, such as a CT or MRI, are needed to diagnose the cause of fourth cranial nerve palsy.
An eye doctor may also prescribe eyeglasses with prism lenses or an eye patch to correct double vision. Vision therapy involving eye exercises is sometimes helpful. Surgery may be performed to align the eyes.
Sixth cranial nerve (abducens)
The sixth cranial nerve is also known as the abducens nerve. It is named so because it abducts the eye — pulling it away from the midline of the face.
Eye function
The abducens nerve controls the lateral rectus muscle, which moves the eye toward the ear.
Symptoms of CN VI palsy
Horizontal double vision is a common sign of CN VI palsy. Double vision occurs because the eyes no longer align.
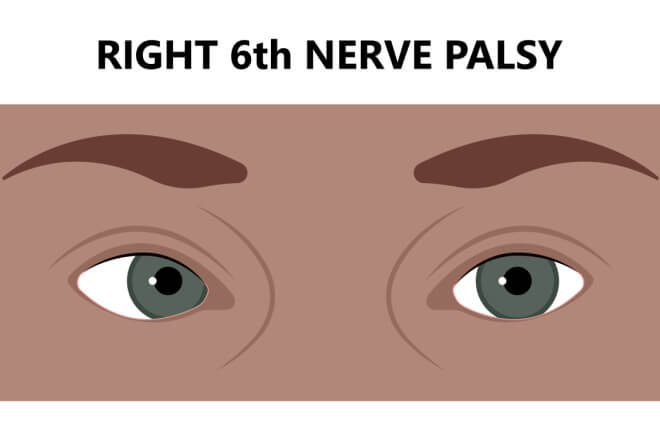
When CN VI is not working, the affected eye will drift toward the nose because the lateral rectus muscle cannot contract. An individual may have difficulty fully turning the eye outward. When only the eyes are involved, it is considered an isolated sixth nerve palsy.
Other symptoms may accompany a sixth cranial nerve palsy, including hearing issues, facial weakness or numbness, and drooping of the upper eyelid. An individual may also experience headache, nausea and vomiting, or fever.
Causes of CN VI palsy
When only the eye is affected, it can be due to head trauma or a viral infection. Damage to blood vessels from medical conditions, such as diabetes and high blood pressure, can also lead to isolated sixth nerve palsy.
Conditions that increase the pressure in the skull may cause additional signs and symptoms. The most common causes include:
Head injury
Infection
Inflammation
Stroke
Brain tumor
Aneurysm
Multiple sclerosis
Treatment of CN VI palsy
In many cases, a sixth cranial nerve palsy becomes better on its own after several months. An eye doctor can also prescribe eyeglasses with prism lenses or an eye patch to correct double vision. Sometimes a botox injection helps relieve symptoms temporarily.
Since many different conditions can lead to a sixth nerve palsy, treatment includes managing the underlying condition. A clinical exam, imaging (such as a CT or MRI), laboratory tests and/or a spinal tap may be needed to diagnose the cause. Medical therapy includes antibiotics and corticosteroids. Surgery and other treatments may be necessary.
Seventh cranial nerve (facial)
The seventh cranial nerve is also known as the facial nerve. It controls some of the movements and expressions of the face and some functions of the eye.
Eye function
CN VII allows forceful eyelid closure and normal blinking. It also innervates the lacrimal gland of the eye, which produces tears. The nerve also allows us to move the forehead and eyebrows.
Symptoms of CN VII palsy
Historically, sudden weakness and inability to move the face on one side have been thought to be due to seventh cranial nerve palsy of unknown cause, commonly known as Bell’s palsy.
More recently, seventh nerve palsy due to an unknown cause is thought to actually be due to a viral infection or an immune disorder and placed into its own category.
CN VII palsy often begins with pain behind the ears and the onset of facial symptoms within hours. The face feels numb and dragged down and contorted. Someone with facial nerve palsy will experience dry eye symptoms and find it difficult to close the eye on the affected side.
Causes of CN VII palsy
Facial nerve palsy has many underlying causes. The conditions that result in facial nerve palsy can be due to the following:
Infection
Injury
Inflammation
Tumor
Medical or surgical treatment
Unknown cause
Congenital (present at birth)
Treatment of CN VII palsy
In most cases, a seventh cranial nerve palsy becomes better on its own within several months. An eye doctor may patch the eye or recommend artificial tears or a salt solution to protect the affected eye from drying out.
Typically, oral corticosteroids are prescribed if symptoms have been present for less than two days. This medicine helps to decrease nerve swelling and can help facial movement return faster. Antiviral drugs are sometimes prescribed, but their effectiveness has not been proven.
Sometimes during the healing process, the nerve forms abnormal connections, resulting in eye-watering when the mouth waters. Because facial nerve palsy has specific symptoms, doctors can typically diagnose it fairly easily. To rule out other conditions, additional tests may be needed.
When to see a doctor
It is important to seek urgent medical care if you notice any sudden changes in vision or eye alignment or an abnormally dilated pupil. The underlying cause of some of these signs and symptoms can be a medical emergency. Earlier treatment will result in a better long-term outcome.
Cranial nerve palsy. American Association for Pediatric Ophthalmology and Strabismus. April 2022.
Neuroanatomy, cranial nerve. StatPearls. October 2022.
Optic atrophy. EyeWiki. American Academy of Ophthalmology. September 2022.
Neuroanatomy, cranial nerve 3 (oculomotor). StatPearls. March 2022.
Cranial nerve III palsy. StatPearls. July 2022.
Third cranial (oculomotor) nerve disorders. Merck Manual Professional Edition. September 2022.
Third nerve palsy. American Association for Pediatric Ophthalmology and Strabismus. March 2020.
Brain herniation. Mount Sinai. July 2022.
Anatomy, head and neck, eye superior oblique muscle. StatPearls. August 2022.
Cranial nerve 4 palsy. Texas Children’s Hospital. Accessed March 2023.
Fourth cranial (trochlear) nerve palsy. Merck Manual Professional Edition. September 2022.
Trochlear nerve. Cleveland Clinic Foundation. August 2021.
Sixth nerve palsy. Cedars-Sinai. Accessed March 2023.
Neuroanatomy, cranial nerve 6 (abducens). StatPearls. November 2022.
Sixth cranial (abducens) nerve palsy. Merck Manual Professional Edition. September 2022.
Neuroanatomy, cranial nerve 7 (facial). StatPearls. July 2022.
Facial nerve palsy. EyeWiki. American Academy of Ophthalmology. January 2023.
Facial nerve palsy. Merck Manual Professional Edition. September 2022.
Page published on Wednesday, March 8, 2023
Page updated on Tuesday, March 14, 2023






