Hemifacial spasm (face twitching)
What is a hemifacial spasm?
Hemifacial spasm is a chronic neuromuscular disorder causing painless, uncontrolled twitching on one side of the face. It begins at the eyelid and spreads toward the mouth and cheeks. In the early stages, the twitching only occurs occasionally, but in later stages, it can occur constantly.
Hemifacial spasm is usually long-lasting. Middle-aged women are most likely to have this condition, although it can occur in both men and women. This condition is most frequently seen in people with Asian heritage. A person experiencing a hemifacial spasm can appear to be having a seizure, although it is not one. This can sometimes result in awkwardness in public settings.
What causes hemifacial spasm/face twitching?
Facial twitching in hemifacial spasms is caused by abnormal activity of the facial nerve — the seventh cranial nerve.
A hemifacial spasm can result when the facial nerve is irritated, often because something is pressing against it. When pressure is applied to a nerve, it can cause it to fire spontaneously and abnormally.
When an irritated facial nerve discharges, it sends signals to different parts of the nerve along its pathway, causing spasms in different parts of the face the nerve controls.
The facial nerve is responsible for some functions and movements of the:
Eyes
Mouth
Lips
The orbicularis oculi muscle — responsible for closing the eyelid — is typically the first to be affected. Over time, the spasm progresses beyond eye twitching, and the other muscles of facial expression become involved as well.
Hemifacial spasm can be the result of one of several causes:
Idiopathic
Many cases of hemifacial spasm do not have a clear cause — they are idiopathic.
Pressure from a blood vessel
When a cause is identifiable, it is typically because another structure is pressing on the facial nerve and irritating it as it leaves the base of the brain. The source of compression is often a blood vessel, particularly a dilated artery or hardened artery. A blood vessel that has moved out of its normal position may also place pressure on the facial nerve, causing it to become irritated.
READ MORE: 15 ways heart disease affects eye health
Pressure from a tumor
A less common cause is a benign (not cancerous) head or neck tumor pressing on the nerve.
Secondary to an injury
Damage to the facial nerve can cause a secondary hemifacial spasm. This can occur when the facial nerve does not grow back normally, and nerve signals are misdirected, causing spasms on that side of the face.
Secondary to Bell’s palsy
A viral infection can cause inflammation of the facial nerve and result in weakness on one side of the face, causing Bell’s palsy. While most patients recover from the weakness, hemifacial spasm can occur months later — in some cases, even years later.
Less common causes
Some uncommon causes can also lead to a hemifacial spasm. These include:
Aneurysms
Brain tumors
Multiple sclerosis and other demyelinating diseases
READ MORE: Eye symptoms commonly seen in multiple sclerosis
Signs and symptoms
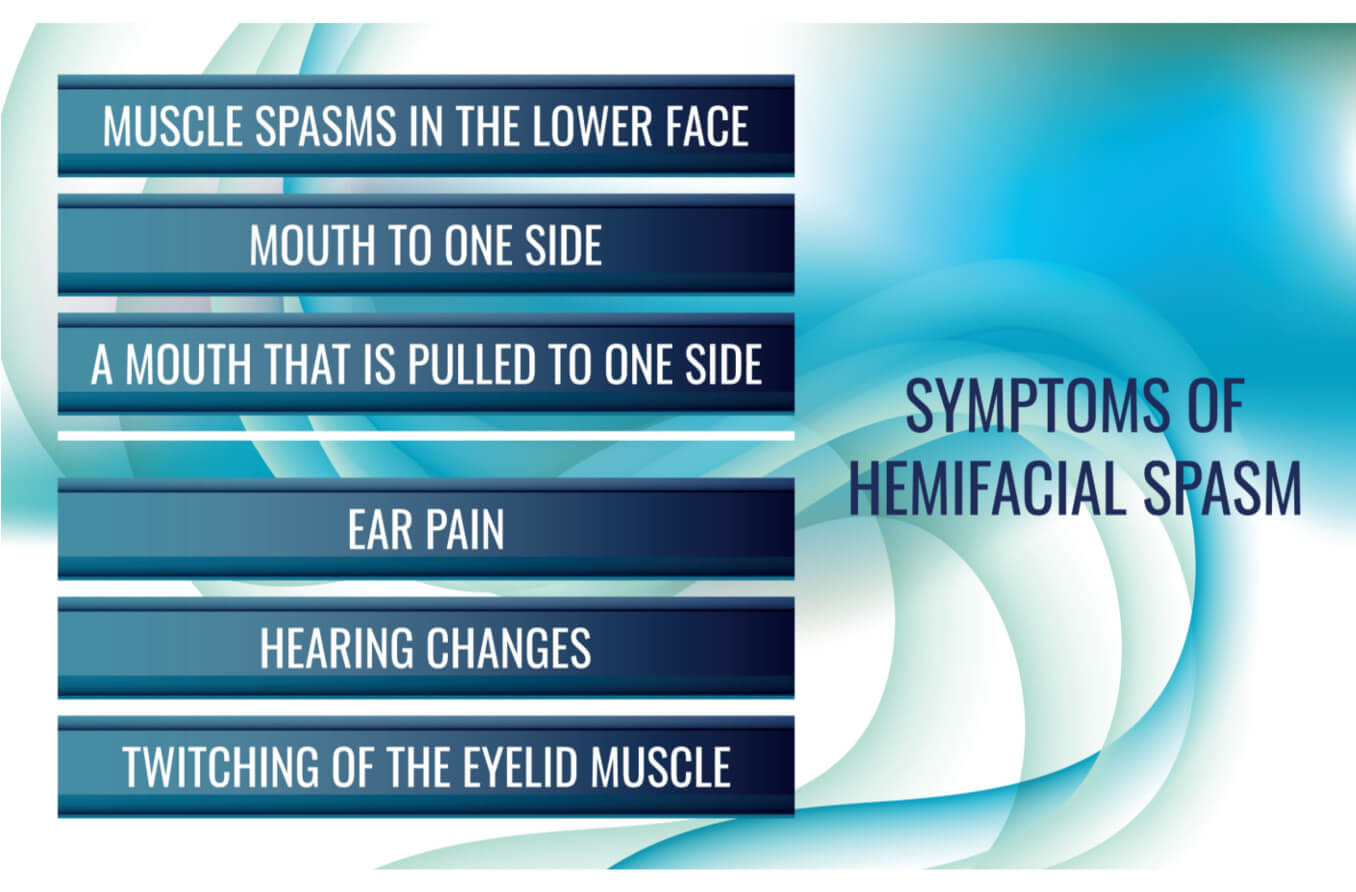
The most apparent symptom of a hemifacial spasm is uncontrollable and painless twitching on one side of the face, often pulling it to that side. The symptoms often begin near the eye and become more severe. Over time, the face may twitch continuously, involving the cheeks and mouth. The facial nerve does not receive pain stimuli, which is why the spasms are not painful.
A patient with hemifacial spasm may experience other symptoms in addition to facial twitching, including:
Fatigue
Facial tic
Skin rash
Nausea
Balance issues
Hearing loss or ear pain
Vision issues
Some people with hemifacial spasm will have mild symptoms with periods when they are free of symptoms. Certain factors can increase the frequency and severity of hemifacial spasms, such as:
Specific facial expressions
Specific head postures
Stress
Anxiety
Fatigue
Painful tic convulsif syndrome
Painful tic convulsif syndrome (PTCS) is a rare syndrome in which hemifacial spasm occurs at the same time as a condition called trigeminal neuralgia. This is caused by abnormal discharge of the trigeminal nerve or fifth cranial nerve.
This disorder causes sudden, chronic facial pain and hemifacial spasms because the facial and trigeminal nerves are both involved.
Diagnosis
A person experiencing hemifacial spasm symptoms will need to be evaluated by a neurologist. Magnetic resonance imaging (MRI) may be ordered to rule out tumors or other issues that can cause symptoms similar to a hemifacial spasm. This imaging test can also detect whether a blood vessel is pressing on the facial nerve and causing the spasm.
A neurologist may also order a test for or perform the following:
Eye and vision evaluation
Muscle strength and reflex evaluation
Electromyography (a test that measures the electrical activity of the muscles)
CT scan (a test that takes many X-ray images from different angles around your body)
Angiography (a test that performs an X-ray of the blood vessels using contrast dye)
Treatment, management and prognosis
Most cases of a hemifacial spasm require treatment before they get better. Several types of treatments exist, including antiseizure drugs, Botulinum toxin injections and surgery.
Oral Medication
Hemifacial spasms can be treated with medication, although this option has not been shown to be very effective and can result in many side effects.
Anticonvulsant medications that can be used to treat this condition include:
Carbamazepine (Tegretol®)
Clonazepam (Klonopin®)
Phenytoin (Dilantin®)
Gabapentin (Neurontin®)
Baclofen (Lioresal®)
These medications can cause side effects that can range from mild to severe, such as:
Sleepiness
Nausea
Balance issues
Skin irritation
Injections
Botulinum toxin injections — such as Botox® — are an in-office procedure and often the first treatment option for most patients with hemifacial spasm. A small needle is used to inject botulinum toxin into the muscles of the face. This treatment works by weakening the muscles temporarily so that the twitching stops.
It takes about one week for the injection to work, and the effects last up to 3-4 months, so the injection needs to be repeated. There is a risk of developing resistance, and side effects can occur, including:
Irritation in and around the eye
Dry eye
Drooping eyelids
Incomplete eyelid closure
Double vision
Facial weakness (temporary)
This option has a good success rate, with 80% to 95% of patients seeing improvement.
READ MORE: Botox injections and side effects
Surgery
The surgery for hemifacial spasm depends on the underlying cause. Microvascular decompression is performed if a hemifacial spasm is due to an artery pressing on the nerve.
This surgery requires general anesthesia and is performed by a neurosurgeon. An incision is made behind the ear. The blood vessel pressing on the nerve is moved away, and padding is placed between the artery and nerve to remove the pressure.
The benefits and risks of surgical treatment will vary with each individual. This is typically an effective treatment — with 90% of patients seeing improvement.
But there are potential risks involved, including:
Brain hemorrhage
Stroke
Paralysis or weakness of the facial muscles
Decrease or loss of hearing
Infection
There is also a chance that the spasm will come back even after surgery.
Conditions related to hemifacial spasms
Although many cases of hemifacial are considered idiopathic (unknown origin), some conditions increase the chances of developing a hemifacial spasm.
These include:
Cranial nerve seven injury
Injury to the face
Atherosclerosis (narrowing and hardening of arteries due to buildup of cholesterol and fats)
Bell’s palsy
Family history
READ MORE: Why healthy blood pressure is important for healthy eyes
Coping with hemifacial spasm
Hemifacial spasm is usually a chronic condition. In addition to treatment, it is helpful to have coping strategies to minimize symptoms associated with it.
These include:
Decreasing caffeine intake
Getting plenty of rest and avoiding fatigue
Decreasing stress
Managing anxiety
Speak to your doctor about clinical trials in your area that may be available and could offer potential new treatments.
In addition, the following organizations can assist individuals and caregivers of people living with hemifacial spasm:
Benign Essential Blepharospasm Research Foundation Phone: 409-832-0788
National Organization for Rare Disorders (NORD) Phone: 800-999-6673
A caring team of doctors and healthcare professionals, along with a supportive network of family and friends, are important resources for those living with hemifacial spasm.
READ MORE: Glossary of eye care terms
Hemifacial spasm. RWJ Barnabas Health. Accessed March 2023.
Neuroanatomy, cranial nerve 7 (facial). StatPearls. July 2022.
Hemifacial spasm. EyeWiki. American Academy of Ophthalmology. September 2022.
Hemifacial spasm. Baylor Medicine. 2021.
Hemifacial spasm. UTHealth Houston Neurosciences. Accessed March 2023.
Hemifacial spasm. Lillian S. Wells Department of Neurosurgery at the University of Florida College of Medicine. Accessed March 2023.
Painful tic convulsif syndrome. EyeWiki. American Academy of Ophthalmology. October 2022.
Trigeminal neuralgia. National Institute of Neurological Disorders and Stroke. March 2023.
Hemifacial spasm. Bascom Palmer Eye Institute. University of Miami Health System. Accessed March 2023.
Hemifacial spasm (face twitching): Treatment, symptoms & causes. Cleveland Clinic. April 2021.
Page published on Tuesday, April 4, 2023
Page updated on Tuesday, April 11, 2023






