Idiopathic intracranial hypertension (IIH): Symptoms, causes, diagnosis and treatment
What is idiopathic intracranial hypertension?
Idiopathic intracranial hypertension (IIH) is a condition in which fluid around the brain doesn’t drain properly. This leads to a build-up in pressure, which can cause vision problems due to added force on the optic nerve.
IIH is also sometimes called pseudotumor cerebri or benign intracranial hypertension.
What are the symptoms of idiopathic intracranial hypertension?
There are several symptoms associated with idiopathic intracranial hypertension. The most common is a painful headache that is present after waking up. It typically gets worse when bending over, straining or coughing, and it cannot be relieved with medication.
In contrast, headaches caused by muscle strain and stress are usually worse later in the day. And migraine headaches tend to get better with sleep.
Other symptoms of IIH may include:
Dizziness and nausea
Vomiting
Neck and back stiffness
Difficulty walking
Tinnitus (ringing in the ears) that often follows a rhythmic pattern (pulsatile)
Forgetfulness
Depression
Vision changes
Idiopathic intracranial hypertension can cause papilledema — or optic disc swelling. The optic disc is where the optic nerve attaches to the back of the eye. The optic nerve is what connects the eye to the brain. It takes signals from the eye to the brain so the brain can interpret them into images.
IIH’s damage to the optic nerve can lead to:
Dim, blurry or dull vision
Short periods of complete vision loss often associated with straining, coughing or bending over
Papilledema can take anywhere from a few hours to a few weeks to develop, based on the speed of pressure build-up. If the pressure continues to build, this may result in optic atrophy or death of the nerve fibers. This typically leads to permanent vision loss.
What causes idiopathic intracranial hypertension?
IIH’s name breaks down the main components of the disease. Idiopathic is a term that refers to conditions with unknown causes. Intracranial is the space inside the skull. And hypertension is the medical term for high fluid pressure.
Idiopathic intracranial hypertension is caused by a build-up of cerebro-spinal fluid (CSF). CSF surrounds the brain and spinal cord, providing protection from injury. The exact process of production, flow, drainage and reabsorption that CSF cycles through is not fully understood.
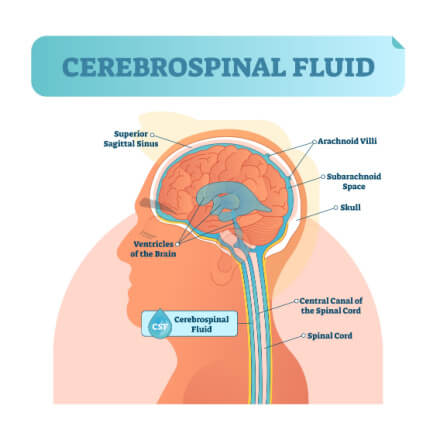
Idiopathic intracranial hypertension is caused by a build-up of cerebro-spinal fluid (CSF).
When CSF does not properly drain, it builds up. This build-up is what causes the increased pressure that leads to IIH.
Individuals of any age or gender can develop idiopathic intracranial hypertension. However, for adults, it is most common in females of child-bearing age, particularly those who suffer from obesity. Adult males who develop IIH also tend to be overweight. IIH that develops in pre-pubescent individuals does not show a higher incidence in females or any link to weight.
It is important to distinguish between primary and secondary intracranial hypertension. IIH is the primary version, which develops without any known cause.
Secondary intracranial hypertension has an identifiable cause. Some of these causes include:
Birth control
Antibiotics
Chemotherapy
Steroids
Acne medications
Sleep apnea
Systemic diseases like lupus, leukemia, kidney failure, meningitis and dural venous sinus thrombosis
How is idiopathic intracranial hypertension diagnosed?
Diagnosing idiopathic intracranial hypertension often involves ruling out other conditions. Tumors, infections and inflammation all cause similar symptoms to IIH. A condition in which the bottom of the brain bulges through the opening at the base of the skull — called a Chiari Malformation — will need to be ruled out as well.
If the patient sees an eye doctor first, they will likely check the patient’s visual field. The visual field is the total range the patient can see while looking at a fixed point. This is to look for potential peripheral vision loss, a common issue with IIH.
The eye doctor may also dilate the patient’s eyes in order to examine the inside of the eye more closely. Dilation involves eye drops that widen — or dilate — the pupil. This lets more light into the eye, allowing the physician to check for optic nerve swelling.
To confirm if IIH is behind any of these optic concerns, a doctor will also likely perform an MRI or CT scan followed by a spinal tap.
Computed tomography (CT) and magnetic resonance imaging (MRI) scans can rule out a tumor or other mass in the brain. Both scans, while performed differently, allow the physician to view the interior of the head. If these scans come back normal, a spinal tap will be done.
A spinal tap — also called a lumbar puncture — can help the physician gauge the pressure of the patient’s CSF. To perform the spinal tap, the doctor will insert a needle between two vertebrae in the spinal cord.
This allows the doctor to measure the pressure of the patient’s CSF and draw a sample for testing. If the spinal tap shows high CSF pressure, a diagnosis of intracranial hypertension can be confirmed.
How is idiopathic intracranial hypertension treated?
Treatment for idiopathic intracranial hypertension depends on the severity of the condition. A spinal tap performed as part of the diagnostics may temporarily reduce the pressure of the CSF and provide some relief from symptoms.
But further treatment is often necessary for long-term results. For overweight patients, weight loss can also help improve symptoms.
In milder cases, the doctor may prescribe the glaucoma medication acetazolamide. This medication helps reduce CSF production. It may be combined with topiramate, which helps with headaches and weight loss. Diuretics (water pills) may also be prescribed to help flush out excess fluid.
Some patients may develop more severe or rapid progression of symptoms. In these cases, surgery may be necessary. For those with papilledema, optic nerve sheath fenestration is preferred. To perform this procedure, the surgeon creates a window in the sheath (outer cover) of the optic nerve, reducing pressure on the nerve.
For other patients with IIH, the doctor might recommend a CSF shunt to reduce intracranial pressure. A shunt is a tube placed in the brain or spine to help redirect CSF to another part of the body. The CSF can then be reabsorbed.
When should you see a doctor?
It is important to see an eye doctor if you notice any changes to your vision, even if those changes are temporary. Double vision or decreased peripheral vision may be signs of IIH. Sudden, painful headaches, accompanied by nausea and vomiting, may also indicate IIH. Seek immediate medical attention if any of these symptoms arise.
What is idiopathic intracranial hypertension? American Academy of Ophthalmology. October 2022.
Idiopathic intracranial hypertension. Cedars-Sinai. Accessed February 2023.
Pseudotumor cerebri (idiopathic intracranial hypertension). EyeWiki. September 2022.
Idiopathic intracranial hypertension. National Organization for Rare Disorders. January 2020.
Cerebrospinal fluid dynamics and intracranial pressure elevation in neurological diseases. Fluids and Barriers of the CNS. April 2019.
Optic nerve. Cleveland Clinic. January 2022.
Papilledema. EyeWiki. American Academy of Ophthalmology. April 2021.
Visual field. MedlinePlus. March 2021.
Get a dilated eye exam. National Eye Institute. May 2021.
Lumbar puncture (spinal tap). Mayo Clinic. April 2022.
CT scan versus MRI versus X-ray: What type of imaging do I need? Johns Hopkins Medicine. Accessed February 2023.
Shunt procedure. Johns Hopkins Medicine. Accessed February 2023.
Optic nerve decompression. StatPearls. August 2022.
Page published on Wednesday, March 1, 2023
Page updated on Tuesday, March 7, 2023
Medically reviewed on Saturday, January 14, 2023






