How Lyme disease affects the eyes
Lyme disease overview
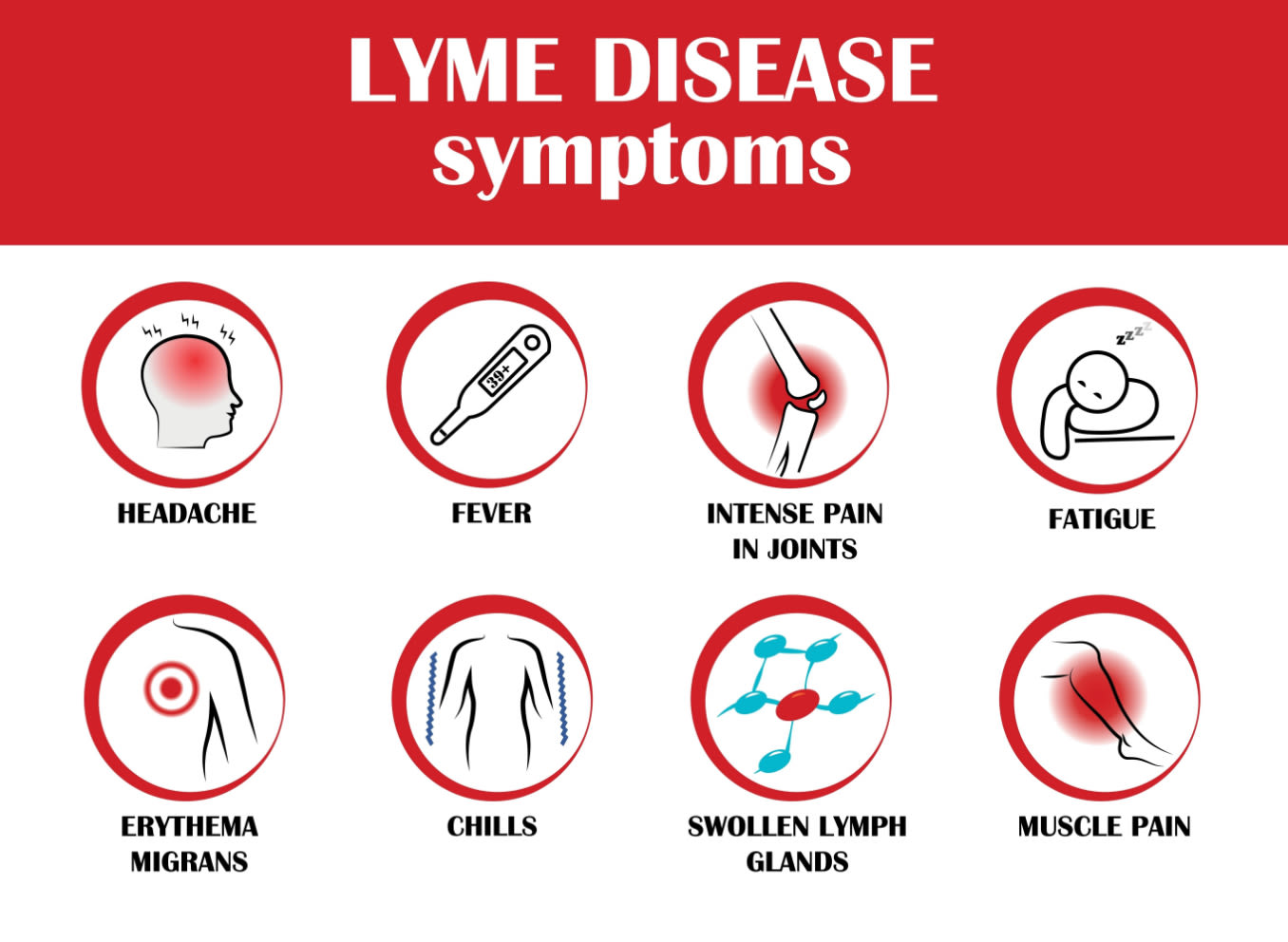
Lyme disease is a bacterial infection that is spread by ticks. It is most easily recognized by a bull’s-eye-like rash on the body. Lyme disease can cause a variety of symptoms, such as joint pain, fever and fatigue. It can also cause eye-related issues, such as conjunctivitis and uveitis.
Early treatment is important to prevent long-term effects. There are three main stages of Lyme disease that evolve from one to the next:
Stage one
This stage is considered early localized Lyme disease. It lasts for one to four weeks. The most common sign is a bull’s-eye rash, called erythema migrans, that can be up to 12 inches in size and feel warm to the touch. Erythema migrans appears at the location of the tick bite.
Patients may also experience flu-like symptoms, such as a fever, headache, and body and joint aches. Patients can also have a stiff neck, tiredness, mild inflammation of the conjunctiva (including redness and tearing) and swollen glands.
Stage two
This stage is called early disseminated Lyme disease. It lasts for one to four months. Signs and symptoms include malaise (feeling unwell), muscle pain, headaches and rashes on other areas of the body.
Patients may also experience Bell’s palsy, neuropathy, heart problems, eye pain and double vision.
Stage three
This stage is called late Lyme disease. It is also called persistent late disseminated Lyme disease. It can last for four months or even years after contracting the disease. Symptoms include arthritis (especially in the knee) and muscle issues.
Patients can also experience brain fog, brain damage or nerve damage.
Eye-related symptoms and complications
There are a variety of eye-related symptoms, conditions and complications that occur in the different stages of Lyme disease.
Stage one eye issues
Follicular conjunctivitis — A type of conjunctivitis in which small immune patches, called follicles, appear in the conjunctiva. This can cause watery eyes, light sensitivity and eye pain.
Episcleritis — A condition that causes inflammation of the episcleral tissue of the eye. Symptoms include patchy eye redness, light sensitivity and discomfort.
Stage two eye issues
Uveitis — A disease that usually affects the uvea (iris, ciliary body and choroid). It can cause eye redness, pain and inflammation in the front, middle or inner part of the eye.
In those with Lyme disease, it typically causes intermediate uveitis. This occurs in the middle part of the eye. Symptoms include eye redness, light sensitivity, blurry vision and floaters.
Granulomatous iritis (anterior uveitis) — A common form of inflammation of the eye that causes the eye to be red and painful.
Neuroretinitis — An inflammatory condition that affects both the optic nerve and the retina. Central vision may become compromised, as well as the ability to see colors. Patients usually do not feel any pain.
In this condition the optic nerve as well as the macula are swollen. The macula may have spoke-like patterns of deposits called a macular star.
Chorioretinitis — A type of uveitis that causes inflammation of the posterior, or back, part of the eye. This area includes the choroid and retina. Chorioretinitis can cause vision loss.
Retinal vasculitis — A condition that causes inflammation of the vessels of the retina. It can threaten your sight.
Exudative retinal detachment — A condition that affects the blood-retinal barrier. The blood-retinal barrier helps to maintain the health of the retina. When this barrier is disrupted, fluid can build up and cause the retina to detach.
Optic neuritis — An inflammatory condition that affects the optic nerve. It usually only happens in one eye. Symptoms include blurry vision, difficulty seeing at night, eye pain with eye movement and vision loss.
Optic neuritis can progress to neuroretinitis when the retina becomes swollen and inflamed as well.
Papilledema — A term used to describe the swelling of the optic disc, typically in both eyes. Symptoms include headaches and double vision. It can also cause transient visual obscurations. This is when your vision becomes obscured for five to 15 seconds at a time.
Stage three eye issues
Keratitis — A condition that involves inflammation of the cornea. It can cause scarring of the cornea, eye redness, eye pain, blurred vision and watery eyes.
Episcleritis — A condition usually seen in stage one. Episcleritis can also occur in stage three. But it is not as common as keratitis.
Symptoms of stage three Lyme disease may not appear for months or years after the patient is infected.
Diagnosis and treatment
It is often difficult to diagnose Lyme disease. Tick bites can go unnoticed because they are not painful. Your doctor will look for the bulls-eye rash and ask if you have been in an area that is prone to ticks. They can also give you a blood test.
Two positive blood tests are needed to receive a Lyme disease diagnosis. However, if you have a bulls-eye rash and have recently spent time in an area where you could have been exposed to ticks, your doctor may start treatment before receiving blood work results.
Lyme disease is usually treated with antibiotics. For those aged 8 and younger, a doctor will typically prescribe amoxicillin or cefuroxime. For those older than 8 years, a doctor may prescribe doxycycline.
The earlier you receive a diagnosis and treatment, the quicker your recovery.
Vision care tips for Lyme disease patients
Once a patient has started antibiotic treatment, they can then start treatment for any ocular issues. Your doctor can prescribe topical corticosteroids for inflammation.
Mydriatics may also be prescribed. These drugs dilate, or open, the pupil. Mydriatics can also assist in treating inflammation.
Prevention and early detection
Around 30,000 cases of Lyme disease are reported in the U.S. every year. The disease is actually caused by a bacterium, Borrelia burgdorferi, which is spread by deer ticks.
Thus, wooded areas where deer reside are the most common locations of contracting Lyme disease. If you are located in the northeastern or midwestern areas of the U.S. and spend time outdoors in the spring, summer and/or fall, you are more susceptible to tick bites.
There are many ways you can prevent Lyme disease. They include:
Covering the skin with long-sleeved shirts and pants. Make sure your sleeves are tight-fitting and you tuck your pants into your socks to deter ticks.
Wearing light-colored clothing. This will make it easier to see any ticks that may be on your clothes.
Wearing a hat to protect your head.
Spraying your clothes with bug repellents that contain DEET. You can also use a spray that contains the insecticide called permethrin. Be careful with overuse.
Avoiding tall grasses and brush when walking on trails.
After spending time outdoors, checking yourself for ticks. Then shower and scrub yourself with a washcloth.
Putting your clothes in the dryer for 15 minutes to kill any ticks that might be on them.
If you have pets that spend time outdoors, checking them for ticks when they come inside.
If a tick has bitten you, use tweezers to tug the head and gently remove it from your skin. Do not use your fingers to squeeze the tick or you could expose yourself to the bacteria. Clean the area with soap and water.
Make an appointment to see your doctor right away if you: have been bitten by a tick, notice a bulls-eye rash on your skin or have spent time outdoors and do not feel well.
If you have been bitten by a tick and experience any eye signs or symptoms, make sure you get a dilated eye exam and inform your eye doctor of your possible exposure to Lyme disease.
Lyme disease. Cleveland Clinic. August 2022.
Lyme disease. StatPearls. May 2023.
Lyme disease. EyeWiki. American Academy of Ophthalmology. May 2023.
Follicular conjunctivitis. Vagelos College of Physicians and Surgeons. Accessed June 2023.
Episcleritis. EyeWiki. American Academy of Ophthalmology. September 2022.
Uveitis. Cleveland Clinic. February 2021.
Granulomatous iritis (anterior uveitis). Medscape. February 2023.
Neuroretinitis. EyeWiki. American Academy of Ophthalmology. May 2023.
Chorioretinitis. StatPearls. May 2023.
Retinal vasculitis. EyeWiki. American Academy of Ophthalmology. June 2023.
Exudative retinal detachment. StatPearls. February 2023.
Optic neuritis. Cleveland Clinic. January 2019.
Papilledema. Cleveland Clinic. November 2022.
Keratitis. Johns Hopkins Medicine. Accessed June 2023.
Mydriatics. Drugs.com. June 2023.
Page published on Tuesday, July 4, 2023
Page updated on Tuesday, July 11, 2023
Medically reviewed on Tuesday, June 20, 2023






