How transient ischemic attacks (TIAs) can impact your vision
What is a transient ischemic attack (TIA)?
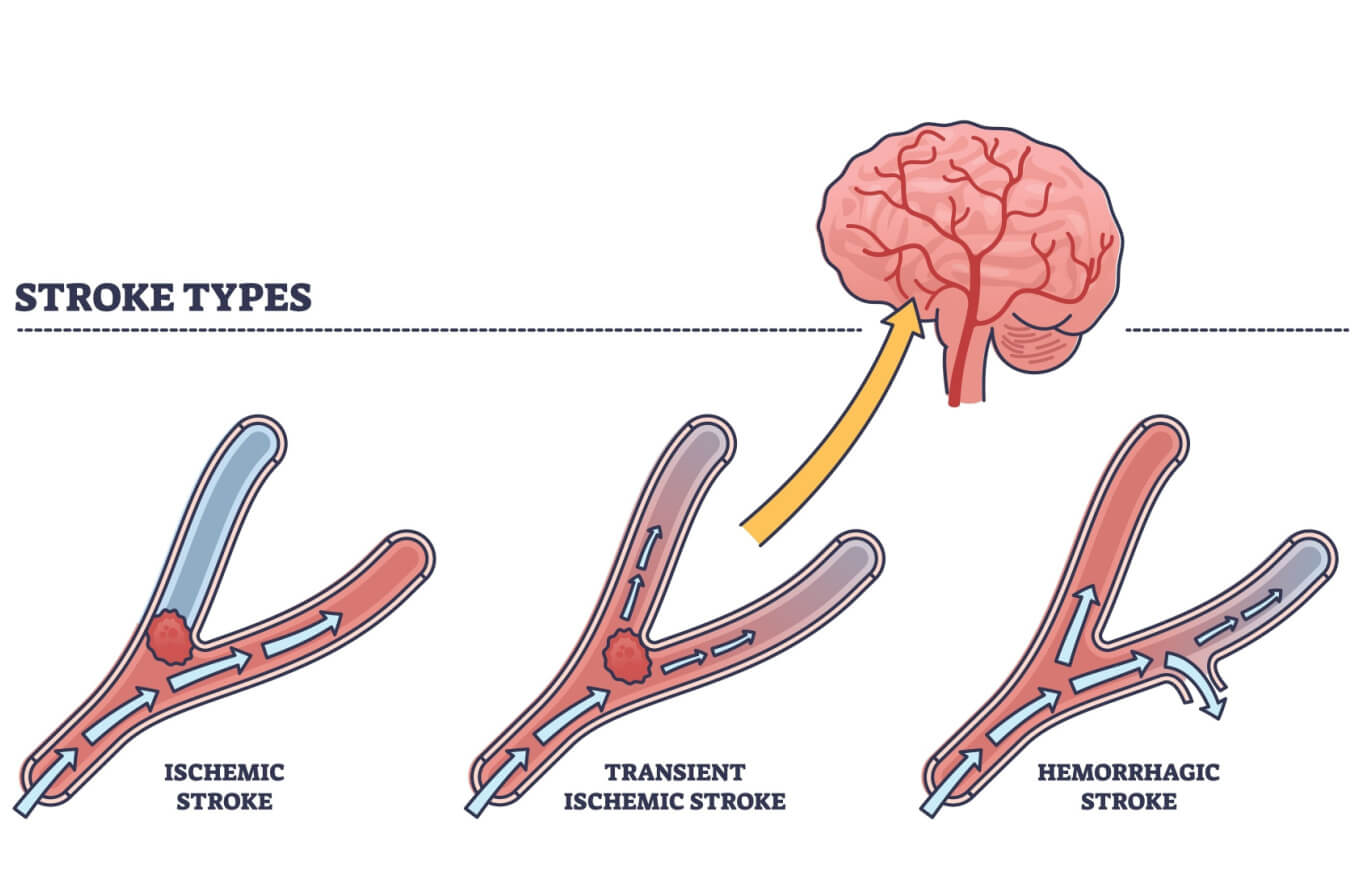
A transient ischemic attack (TIA) is a medical emergency. It occurs when blood flow to the brain suddenly becomes blocked for a brief period. It is sometimes called a “mini-stroke” because symptoms are the same as a stroke. But, because the blockage clears after a short time, they are temporary.
Because a transient ischemic attack (TIA) is a stroke-like episode, the risk factors and signs are the same as for a stroke. In the past, a person with stroke or TIA symptoms was considered to have had a TIA if symptoms went away within 24 hours. However, doctors now look at imaging such as an MRI and clinical and laboratory tests to determine whether someone had a TIA or a stroke.
Although an individual experiencing TIA or stroke symptoms may feel fine after a few hours, it is important to seek urgent medical care. A TIA is a warning that occurs before approximately 15% of strokes. In fact, of individuals who have a TIA, one-third will have a stroke within the next year. The risk of a stroke is greatest in the first two days after a TIA.
READ MORE: A guide to vision changes that can occur after a stroke
What causes a TIA?
A TIA typically occurs due to blockage or constriction of an artery to the brain, resulting in insufficient oxygen and nutrition to the part of the brain the blood vessel supplies.
Some common causes of a TIA include:
A blood clot in a brain artery
A blood clot that has moved to the brain from another part of the body
Narrowing of blood vessels causing decreased or turbulent blood flow
Injury to blood vessels causing decreased or turbulent blood flow
Risk factors for a TIA
There are a number of risk factors that increase the likelihood of having a TIA.
These include:
High blood pressure – This is the most important risk factor for TIA. High blood pressure causes arteries to become leaky and lose their elasticity, limiting blood flow and causing it to become turbulent.
High cholesterol – Low-density cholesterol circulating in the bloodstream tends to build up in the walls of arteries. With age, the interior of these arteries becomes narrowed by cholesterol plaques, causing a blockage.
Diabetes – High blood sugar caused by diabetes causes blood vessels to become damaged, leading to poor blood flow.
Smoking – Cigarette smoking compounds the damage to blood vessels caused by existing risk factors.
Older age – As people age, their arteries become hardened and less elastic, and cholesterol deposits (plaque) accumulate on the walls of arteries, increasing the risk of blood flow blockage.
Other risk factors that increase the risk of TIA include alcohol abuse, blood clots, poor diet, high stress and a sedentary lifestyle.
READ MORE: 15 ways heart disease affects eye health
Transient ischemic attack and vision
Vision processes take up about one-third of the brain. As a result, a TIA, like a stroke, often causes vision and eye symptoms.
The following eye and vision symptoms can occur during a TIA, usually only lasting for a few hours or less:
Blurry vision in one or both eyes
Double vision in one or both eyes
Temporary loss of vision in one or both eyes
Eye movements are controlled by nerves whose pathways can be affected during a TIA. Due to this, the eyes may temporarily not align or move together. This can also result in double vision.
Depending on what part of the visual pathway is affected, temporary blurry vision or vision loss in an individual’s field of view can result.
Retinal TIA (amaurosis fugax)
In some cases, a TIA may only affect the eyes. This is called an ocular/retinal TIA. This can occur when a blood vessel supplying one or both eyes becomes blocked, resulting in a lack of blood flow to the retina. This is a cause of amaurosis fugax — a short-term loss of vision in one or both of the eyes.
A retinal TIA may result from blockage of the internal carotid artery. This temporary loss of vision in one eye can last up to 30 minutes. It is a warning sign that a stroke may happen, much like a cerebral (brain) TIA.
SEE RELATED: Is eye twitching a sign of a stroke?
Signs you are having a TIA
A TIA will cause symptoms that are essentially the same as a stroke. A doctor can determine whether you experienced a TIA or stroke based on test results. Vision loss and other symptoms will vary depending on the part of the brain that is affected.
Signs and symptoms usually begin suddenly and include:
Difficulty seeing in one or both eyes
Weakness or numbness on one side of the body
Difficulty with balance, coordination or walking
Trouble speaking
Confusion or difficulty understanding speech
The acronym FAST refers to the main symptoms of a TIA or stroke:
Face drooping – Drooping face or eyelid, inability to smile
Arm weakness – Arm weakness or numbness, inability to keep both arms lifted
Speech difficulty – Slurred, unclear speech, inability to talk
Time – Time to call 911 immediately
TIA prognosis
Symptoms of a TIA usually do not last more than an hour, although they can continue for up to 24 hours in some cases.
Importantly, the risk of stroke in the next three months after a TIA increases significantly to about 20%. Around half of the strokes that occur after a TIA will happen within the first two days.
A stroke can cause long-term damage to brain tissue. This is why you must seek medical care immediately, even if the symptoms don’t last.
How to decrease your chances of a TIA or stroke
In addition to addressing any underlying conditions and risk factors, the following lifestyle habits have been shown to decrease the risk of a TIA or stroke:
Eat a nutritious diet – Eat meals that are composed of unprocessed, whole foods such as vegetables, fruits, beans, legumes and other lean proteins. Reduce your salt intake.
Exercise and maintain a healthy BMI – Studies have found that exercising 150 minutes a week improves overall health.
Quit smoking – Consult your doctor to create a strategy to stop smoking.
Avoid excessive alcohol consumption – Limit to two drinks per day for men and one drink per day for women.
Manage your stress – Stress may be associated with increased blood pressure and other health issues.
READ MORE: What your eye doctor can tell about your heart health
When to see a doctor
A transient ischemic attack is a medical emergency. Often, TIA symptoms have disappeared by the time a person sees a medical professional. It is still important to seek medical care as the risk of stroke in the next few days is higher.
In addition to a thorough medical history, your healthcare provider will need the following information from you:
What symptoms you experienced
When the symptoms started
How long the symptoms lasted
Any events that you feel may have triggered the symptoms
It is important to provide a thorough medical history to your healthcare provider. Treating the risk factors that may have caused the TIA has been found to greatly reduce the risk of a future TIA or stroke by at least 80%.
Remember, if you experience symptoms associated with a TIA or stroke (such as the symptoms in the FAST acronym), call 911 immediately, even if the symptoms pass quickly.
READ MORE: Stroke Awareness Month
Let’s talk about transient ischemic attack (TIA). American Stroke Association. January 2020.
Transient ischaemic attack (TIA). NHS Stroke Association. Accessed Februrary 2023.
Retinal TIAs: a medical emergency. American Academy of Ophthalmology. March 2018.
Transient ischemic attack. StatPearls. July 2022.
Transient ischemic attack. Mount Sinai. April 2022.
High blood pressure dangers: Hypertension's effects on your body. Mayo Clinic. January 2022.
Diabetic retinopathy. National Eye Institute. July 2022.
Smoking and your heart. National Heart, Lung, and Blood Institute. March 2022.
Heart health and aging. National Institute on Aging. June 2018.
Stroke-related vision loss. Wilmer Eye Institute. Accessed February 2023.
Stroke/hemianopsia. VisionAware. American Printing House for the Blind. Accessed February 2023.
Amaurosis fugax. MedlinePlus Medical Encyclopedia. May 2022.
Amaurosis fugax. StatPearls. August 2022.
Transient ischaemic attack (TIA). NHS Inform. National Health Service (Scotland). February 2023.
Page published on Tuesday, March 7, 2023
Page updated on Tuesday, March 14, 2023
Medically reviewed on Tuesday, January 31, 2023






