Visual snow syndrome: Causes, symptoms and treatment
What is visual snow syndrome?
Visual snow syndrome is a rare neurological condition that causes images and scenery to appear “snowy,” as if the world in front of a person is filtered with television static. The condition does not go away, even when a person closes their eyes, and it can also cause light sensitivity and floaters.
Although visual snow syndrome affects the way someone sees, it is not related to the structure of the eyes. It has to do with the way images are processed in the brain.
What does visual snow look like?
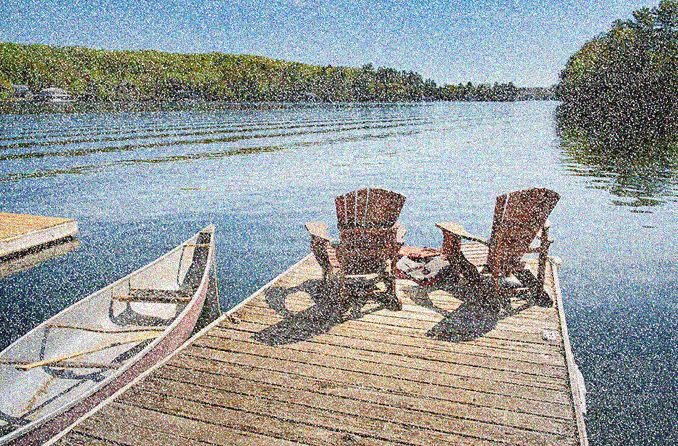
Those who have visual snow syndrome (VSS) see small, scattered dots that occur throughout the field of vision. The dots do not get bigger or smaller and do not form clumps.
There are two types of visual snow syndrome — pulse visual snow (pulse VS) and broadband visual snow (broadband VS):
Depiction of typical vision (left) vs. vision with broadband visual snow syndrome (right). [Image credit: Kara Perricone]
Pulse VS – Dots appear in the same tone as the background present. If you’re viewing a dark background, the dots appear even darker than the background. And if you’re looking at a light-colored image, dots appear lighter than that image.
Broadband VS – Dots appear in a contrasting tone to the background present. For example, if you’re looking at a dark image, dots appear to be light. And if you’re looking at a light image, dots appear to be dark.
The intensity level of visual snow syndrome can range from mild to extreme, depending on the person and the symptoms they experience.
Visual noise (also called eigengrau or eigenlicht) may appear similar to visual snow syndrome. This is the perception that a completely dark room has a pixelated gray appearance consisting of small white and black dots. But unlike visual snow syndrome, visual noise is only visible in the dark.
How rare is visual snow syndrome?
A 2020 study found that about 2% of the United Kingdom’s population has visual snow syndrome. However, the number of people with VSS worldwide is difficult to determine because it’s often misdiagnosed.
Because it is so rare, there’s a great deal of research that needs to be done in order to understand visual snow better and provide proper care for those who have it. Organizations including the Visual Snow Initiative, Eye on Vision Foundation and many more support research behind the disease.
Visual snow causes
While there is no known cause for visual snow syndrome, it most likely results from a malfunction in the brain. VSS researchers consider it a neurological condition with both sensory (visual) and psychiatric aspects.
Since a person’s entire field of vision is affected by visual snow syndrome, experts believe that it occurs in the visual cortex of the brain. In other words, because images are not processed correctly in the brain to begin with, they are not produced (or viewed) correctly in the visual field.
Some researchers believe that there is also an association between the use of antidepressants and visual snow syndrome. Some serotonin reuptake inhibitors caused symptoms such as floaters, light sensitivity and visual snow syndrome, according to a 2022 study published in the International Journal of Risk & Safety in Medicine. Since antidepressants affect the way the brain works, it’s reasonable for patients to experience visual snow syndrome as a result of the neurological change.
A 2021 study published in Frontiers in Neurology showed that blue light makes visual snow syndrome worse. Blue light activates a primitive part of the brain that controls neurological pulses called cortical rhythms.
Several other brain disorders — such as migraines, tinnitus (ringing in the ears) and depression — are associated with abnormal cortical rhythms and are also more common in people with VSS.
Visual snow symptoms
The symptoms of visual snow syndrome are primarily visual, although some people also experience things such as headaches, light sensitivity and ringing in the ears.
Specific signs related to the condition include:
Small dots in the visual field
“Snowy” or “television static-like” appearance of images
Additional visual symptoms associated with visual snow syndrome include:
Light sensitivity (photophobia)
Night blindness (nyctalopia)
Images that stay visible even after you’ve looked away or closed your eyes (known as palinopsia or afterimage)
Halos, floaters and eye flashes
Double vision (diplopia)
Additionally, those with visual snow syndrome may experience symptoms that are non-visual, including:
Tinnitus (ringing in the ears)
Anxiety and/or depression due to the stress of the condition
Having an out-of-body sensation (depersonalization)
Headaches or muscle aches
Fatigue
Poor sleep quality
Someone who experiences migraines may have more intense effects and symptoms of visual snow syndrome while they are having a migraine.
Additionally, recreational drugs and alcohol were reported to worsen symptoms in many sufferers of visual snow syndrome.
How is visual snow syndrome diagnosed?
There is a process of elimination when it comes to diagnosing visual snow syndrome. Patients are initially examined by an ophthalmologist to rule out existing eye problems. An MRI and/or a CT scan is also performed by a neurologist to eliminate the possibility of other neurological conditions.
After these initial tests, a doctor will review the patient’s medical history and make note of any recurring symptoms. If certain symptoms are present after other conditions are excluded, a doctor can conclude whether or not visual snow syndrome is to blame.
In order for visual snow to be diagnosed, static or snowy vision must remain constant, and at least two of the following symptoms must be present:
Light sensitivity
Night blindness
Afterimages
Intense floaters or flashes of light
Visual snow syndrome can be very difficult to diagnose, which is why the testing process is so thorough.
Visual snow treatment
There is currently no cure for visual snow syndrome, but patients can do things to manage their symptoms. For example, you can:
Use soft lighting rather than bright bulbs around the house.
Wear rose-tinted eyeglasses to reduce the intensity of your visual symptoms.
Write on neutral-colored paper, such as a yellow-tinted pad rather than a bright white one.
Use a bookmark to guide and separate the lines on a piece of paper as you read or write.
Treat headache symptoms with pain relievers or other remedies as soon as they start.
Certain anticonvulsant and antidepressant medications are available to treat visual snow syndrome. However, they do not completely eliminate symptoms and the side effects are often worse than the cure.
Talk to your doctor about your symptoms in order to manage them properly. For a condition like visual snow syndrome, it’s important to report your experience to both your eye doctor and your neurologist.
READ NEXT: What are phosphenes (seeing stars)?
Visual snow syndrome. National Organization for Rare Disorders. 2018.
Learn. Visual Snow Initiative. Accessed April 2022.
Visual snow. American Academy of Ophthalmology. January 2022.
Brightness constancy and the nature of achromatic colors. Journal of Experimental Psychology. June 1948.
Prevalence of visual snow syndrome in the UK. European Journal of Neurology. May 2020.
Visual snow syndrome. National Center for Advancing Translational Sciences. Accessed April 2022.
Visual snow syndrome causes becoming clearer. Monash University Medicine, Nursing and Health Sciences. March 2022.
Development and persistence of patient-reported visual problems associated with serotonin reuptake inhibiting antidepressants. International Journal of Risk & Safety in Medicine. February 2022.
Short-wave sensitive (“blue”) cone activation is an aggravating factor for visual snow symptoms. Frontiers in Neurology. August 2021.
Page published on Thursday, July 7, 2022
Medically reviewed on Sunday, June 26, 2022






