Hypertensive retinopathy (HTN retinopathy)
What is hypertensive retinopathy?
Hypertensive retinopathy is when high blood pressure (hypertension) damages the blood vessels on the inside of the eye (retina and choroid). It's generally diagnosed during an eye exam and usually does not affect vision unless it has progressed to an advanced stage.
Some medical professionals call hypertensive retinopathy "HTN retinopathy" instead. It's associated with serious health conditions such as stroke, kidney damage and heart disease.
A diagnosis of hypertensive retinopathy can be a sign that high blood pressure is also damaging other parts of the body. This allows the eye doctor to refer you to a primary care doctor or cardiologist for more testing and blood pressure management. Advanced stages of hypertensive retinopathy are a sign of severe hypertension. It requires immediate blood pressure treatment, often in an emergency room.
Causes and risk factors
Causes of hypertensive retinopathy
Hypertensive retinopathy is caused by high blood pressure. Blood pressure is measured using two numbers:
The first number is called systolic blood pressure and measures the pressure in your arteries when your heart beats.
The second number is called diastolic blood pressure and measures the pressure in the arteries between heart beats.
It is often written as a fraction of systolic/diastolic. For example, a blood pressure of less than 120/80 mm Hg is considered within the normal range.
Blood pressure is considered elevated when the systolic pressure is over 120 mm Hg with a normal diastolic under 80 mm Hg. Stage 1 hypertension is when the systolic is regularly over 130 or the diastolic is regularly over 80, and it is stage 2 hypertension when the systolic is regularly over 140 or the diastolic is regularly over 90.
According to these criteria, 46% of adults in the United States have hypertension. In about 85% of cases, the exact cause of high blood pressure is not known. This is called primary hypertension.
In the rest of cases, elevated blood pressure is directly caused by another disease. This is called secondary hypertension.
Risk factors of hypertensive retinopathy
While an exact cause is unknown, several risk factors for primary hypertension have been identified:
Genetics – Hypertension is 2.4 times more likely when both parents have hypertension. It is thought that 30% to 50% of the risk of hypertension is genetic.
Lifestyle – Physical inactivity, obesity, tobacco use and excessive alcohol use have all been shown to increase the risk of high blood pressure.
Diet – A diet that is too high in sodium and too low in potassium can put one at risk for hypertension.
Age – The rate of hypertension is about 22% among adults aged 18 to 39. This rate increases to about 55% among those aged 40 to 59 and to about 75% among those aged 60 and over.
Pregnancy – Hypertension affects 5% to 10% of pregnancies. It can be a sign of preeclampsia, a serious and potentially life-threatening condition.
Risk factors for secondary hypertension include:
Kidney disease
Hormone imbalance
Vascular disorders
Autoimmune diseases
Sleep apnea
Use of certain medications
Hypertensive crisis, also called malignant hypertension, is when blood pressure rises very quickly to 180/120 or higher. This can cause damage to your eyes, heart and other important parts of the body.
READ MORE: Valsalva retinopathy
Signs and symptoms
There usually aren't any hypertensive retinopathy symptoms until the condition is severe.
If it isn't managed, it could lead to vision loss or blindness. Uncontrolled retinopathy can also lead to other eye complications that have their own symptoms.
A hypertensive crisis can present with:
Anxiety
Chest pain
Nausea and vomiting
Confusion
Not responding to a stimulus (unresponsiveness)
Seizures
Call 911 if your blood pressure is 180/20 or higher and you have symptoms.
When a hypertensive crisis causes symptoms, it's called a hypertensive emergency. This is a sign that high blood pressure is hurting your organs, including your eyes.
But a hypertensive crisis doesn't always cause symptoms. This is called hypertensive urgency.
Talk to a medical professional right away any time your blood pressure reading is 180/120 or higher, even if you don’t have symptoms.
READ MORE: Sudden blurry vision in one eye: What does it mean?
Testing and diagnosis
Hypertensive retinopathy is detected by looking into the eye. To get the best view, the eye doctor will likely dilate the pupils.
They'll perform an ophthalmoscopy, which is a very common eye test. During the test, the doctor will shine a bright light into your eye with a tool called an ophthalmoscope. This helps them see certain changes in and around your retina.
If your doctor sees any signs of hypertensive retinopathy, they may order additional tests or refer you to a retina specialist.
Fluorescein angiography (FA)
In some cases, your ophthalmologist may inject a dye called fluorescein into your arm. The dye then moves into the blood vessels in your eye.
This test is called fluorescein angiography. It makes it easier for the doctor to see any problems with blood flow in or behind your retina.
Your vision will be blurry for several hours afterward, so someone will need to drive you home.
Hypertensive retinopathy stages and progression
Hypertensive retinopathy progresses through four different phases:
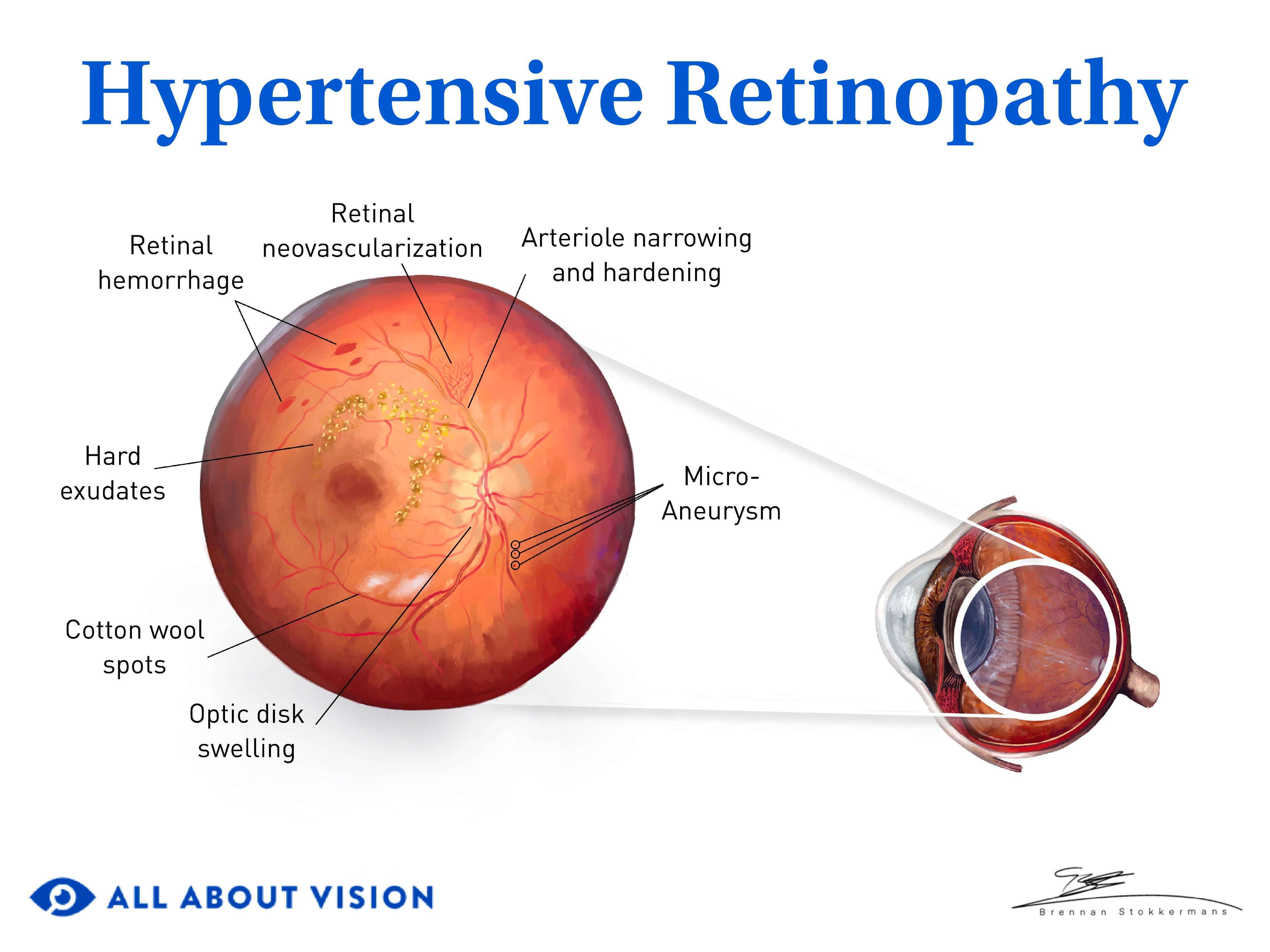
In the vasoconstrictive phase, the small arteries (called arterioles) in the retina become narrow when compared to the small veins (called venules). The size-ratio between arterioles and venules is usually 2 to 3 but may become 1 to 3 in hypertensive patients. In older patients, the narrowing of the blood vessels may be irregular, making the blood vessels appear irregular as well.
The sclerotic phase is when the arterioles harden. Moderate hardening causes the blood vessels to look more yellow (called copper wiring), and severe hardening makes the blood vessels appear silver (called silver wiring). When a hardened arteriole compresses a venule, this is called arteriovenous (AV) nicking.
The exudative phase occurs when the blood vessels start to leak or stop functioning. Leaky blood vessels release plasma (called hard exudate) or blood into the retina. When blood is released into the superficial retina, the hemorrhages have a flame shape. When it is released into the deeper retina, the hemorrhages have a dot or blot appearance.
If blood vessels stop functioning, this creates small areas of reduced blood flow. In these areas, the retina will swell up, causing a grayish discoloration that is called a “cotton-wool spot” (a soft exudate).
In the malignant phase, two tissues close to the retina — the optic disc and the choroid — are also affected.
The optic disc becomes swollen, which is called papilledema. Fluid that leaks from the swollen optic disc may then settle in the center of the retina (the macula). This creates hard exudates in a ring shape called a macula star. When these changes happen, it is called hypertensive optic neuropathy.
The choroid, in turn, can develop areas of blockage. This then creates areas of too much or too little pigmentation in the retina. Pigmented spots surrounded by a halo of less pigment are called Elschnig spots. Lines of pigment loss are called Siegrist streaks. When these changes happen, it is called hypertensive choroidopathy.
Fluid from the choroid may also push against the retina and cause a serous retinal detachment.
READ MORE: Retinal detachment: Types and what to look for
Classifications and grades
A doctor may also grade a patient’s level of hypertensive retinopathy using one of the following classification systems:
Modified Scheie classification
Scheie classification
Keith-Wagener-Barker classification
Each system of hypertension retinopathy grading uses different levels to summarize the signs of hypertensive retinopathy as it develops.
Modified Scheie classification
Grade 0 – No visible changes in the retinal arterioles (small arteries in the retina)
Grade 1 – Slight narrowing of the arterioles
Grade 2 – More noticeable arteriole narrowing
Grade 3 – Grade 2 signs, plus hemorrhages, cotton wool spots and other related problems in the retina
Grade 4 – Grade 3 signs, plus optic disc swelling caused by higher pressure in the head
Scheie classification
Stage 1 – When light is reflected off the arterioles, the reflection looks wider than usual
Stage 2 – Stage 1 signs, plus an arteriole can be seen compressing a small vein (AV nicking)
Stage 3 – Light reflected off small arteries looks copper colored (called "copper wiring" because each arteriole looks like a copper wire in the retina)
Stage 4 – The reflected light looks silver colored (called "silver wiring" because the arteriole looks like a silver wire)
Keith-Wagner-Barker classification
Grade 1 – Arterioles are slightly narrower
Grade 2 – Noticeable narrowing of arterioles, plus an artery is pressing on a vein (AV nicking)
Grade 3 – Grade 2 signs, plus hemorrhages, cotton wool spots and fatty deposits under the retina
Grade 4 – Severe grade 3 signs, plus retinal or optic disc swelling due to higher pressure inside the head
What is AV nicking?
Arteriovenous nicking, or AV nicking for short, is when a small, hardened artery in the retina presses on a vein.
Chronic high blood pressure is the main reason this can happen. It usually happens when someone hasn't controlled their hypertension well for many years.
Chronic high blood pressure puts too much stress on the inner walls of the tiny arterioles. Over time, the stress damages the walls and causes them to become thick and stiff. This is called arteriolosclerosis.
Atherosclerosis is another possible cause of AV nicking. This is when plaque builds up in your arteries and makes them harder and narrowed.
You can't see AV nicking on your own, but an eye doctor can see it during an eye exam. They use specialized tools and tests that help them see the blood vessels in your retina.
Complications
Persistent swelling of the macula and optic nerve can cause permanent damage to both these structures and result in vision loss.
Hypertensive retinopathy is linked to several other eye complications:
Branch retinal artery occlusion can cause complete loss of side-vision in the area of the blockage.
Branch retinal vein occlusion causes partial loss of side-vision or blurry vision in the area of the blockage. It can also lead to swelling of the macula and growth of new blood vessels in the retina or the iris. This can lead to glaucoma.
Retinal macroaneurysm is an outpouching of a retinal artery. It can result in swelling of the retina or bleeding into the eye (vitreous hemorrhage).
Retinal detachment can be caused by fluid from the choroid or from new blood vessels growing in the retina (neovascularization). It can result in blindness if it progresses into the macula.
Retinal neovascularization is when new blood vessels grow from existing retinal arterioles. These new blood vessels are fragile and can cause a vitreous hemorrhage. They can also pull on the retina and cause a detachment.
Diabetic retinopathy is made worse by hypertension. Diabetic retinopathy and hypertensive retinopathy are caused by different health conditions, but they can both cause similar changes to the blood vessels in your retina.
Untreated hypertension can lead to several serious systemic problems. One study found that if patients with grade 4 hypertensive retinopathy did not receive treatment for hypertension, they had a 50% chance of dying within two months and a 90% chance within one year.
READ MORE: Types of diabetic eye problems
Treatment
Lowering your blood pressure is the best hypertensive retinopathy treatment.
Your doctor may recommend taking blood pressure medication to control your hypertension. These drugs — along with healthy lifestyle changes — can lower your risk of retina damage and other eye problems related to high blood pressure.
If another health condition is causing hypertension, your doctor may suggest treating that condition alongside your blood pressure.
Some of the complications of hypertensive retinopathy can be treated with medicine or surgery. For example:
Retinal neovascularization
An eye doctor can treat neovascularization with surgery or eye injections. These treatments help stop more new blood vessels from growing on the retina.
Vitreous hemorrhage
Treatment will vary based on what caused the hemorrhage and how severe it is. Your eye doctor may recommend a type of laser surgery or a vitrectomy.
Glaucoma
While the damage caused by glaucoma is permanent, an eye doctor can treat the condition so you can keep the vision you have.
Medicated eye drops are the most common form of glaucoma treatment.
If eye drops alone aren't enough to lower your eye pressure, your doctor might recommend a laser procedure or traditional glaucoma surgery.
Retinal detachment
Treatment can vary depending on your retinal detachment. Your eye doctor may recommend detached retina surgery to treat your condition.
Retinal macroaneurysm
Many retinal macroaneurysms go away on their own, but your eye doctor will need to monitor your eyes for a while.
Some people will need treatment in the form of injections or eye surgery.
Prevention
Hypertensive retinopathy is prevented by reducing blood pressure. The World Health Organization recommends the following preventative measures:
Dietary changes
Reduce salt intake to less than 2 grams daily
Reduce saturated and trans fats in the diet
Eat more fruits and vegetables
Lifestyle changes
Be physically active
Reduce alcohol intake
Avoid tobacco use
Manage stress
Manage blood pressure
Regularly check blood pressure
Treat high blood pressure
Manage other health conditions
When should I see an eye doctor?
Talk to an optometrist or ophthalmologist any time you notice changes in your vision.
If you’ve already been diagnosed with high blood pressure and haven't had an eye exam in a while, schedule a check-up with an eye doctor near you.
It's important to have regular eye exams to monitor for complications related to your blood pressure, even if your vision seems normal.
Many eye diseases — including hypertensive retinopathy — can damage your eyes for a long time before you start to notice symptoms. An early diagnosis gives you the best chance of protecting your eyesight.
Hypertensive retinopathy. A.D.A.M. Medical Encyclopedia [Internet]. August 2022.
Hypertensive retinopathy. EyeWiki. American Academy of Ophthalmology. January 2024.
High blood pressure and eye disease. A.D.A.M. Medical Encyclopedia [Internet]. August 2022.
Hypertensive retinopathy. Cleveland Clinic. June 2023.
A review of hypertensive retinopathy and chorioretinopathy. Clinical Optometry. May 2020.
Understanding blood pressure readings. American Heart Association. May 2023.
Patient education: High blood pressure in adults (Beyond the Basics). UpToDate. April 2024.
High blood pressure. Merck Manual Consumer Version. September 2023.
High blood pressure (hypertension). Cleveland Clinic. May 2023.
Genetic factors in the pathogenesis of hypertension. UpToDate. April 2024.
Hypertension prevalence among adults aged 18 and over: United States, 2017–2018. National Center for Health Statistics. CDC. April 2020.
Hypertensive disorders of pregnancy. Cardiology Clinics. February 2021.
High blood pressure during pregnancy. National Center for Chronic Disease Prevention and Health Promotion, Division for Heart Disease and Stroke Prevention. CDC. June 2023.
Secondary hypertension. Cleveland Clinic. May 2019.
Autoimmune disease-associated hypertension. Current Hypertension Reports. February 2019.
When to call 911 about high blood pressure. American Heart Association. May 2024.
Hypertensive emergencies. Merck Manual Professional Edition. September 2023.
Ophthalmoscopy. A.D.A.M. Medical Encyclopedia [Internet]. February 2023.
Hypertensive retinopathy. StatPearls [Internet]. July 2023.
Fluorescein angiography. A.D.A.M. Medical Encyclopedia [Internet]. August 2022.
Differential artery-vein analysis in quantitative retinal imaging: A review. Quantitative Imaging in Medicine and Surgery. March 2021.
A literature review of hypertensive retinopathy: systemic correlations and new technologies. European Review for Medical and Pharmacological Sciences. September 2022.
Hypertensive retinopathy. Merck Manual Professional Edition. April 2024.
Retinal hemorrhage. StatPearls [Internet]. August 2023.
Cotton wool spots. EyeWiki. American Academy of Ophthalmology. November 2023.
Malignant hypertension and the role of ophthalmologists: A review article. Cureus. July 2022.
Papilledema. EyeWiki. American Academy of Ophthalmology. December 2023.
Neuroretinitis. EyeWiki. American Academy of Ophthalmology. April 2024.
Siegrist streaks and Elschnig spots. EyeWiki. American Academy of Ophthalmology. April 2024.
Chapter Seven: Ion channels and myogenic activity in retinal arterioles. Current Topics in Membranes. May 2020.
What is the difference between drusen and exudates? EyeSmart. American Academy of Ophthalmology. September 2023.
Patient education: Edema (swelling) (Beyond the Basics). UpToDate. April 2024.
Arteriosclerosis, atherosclerosis, arteriolosclerosis, and Monckeberg medial calcific sclerosis: what is the difference? Jornal Vascular Brasileiro. June 2021.
Case report: The role of hypertension retinopathy graduation in the management of systemic cardiovascular disease. Journal of Family Medicine and Primary Care. February 2024
What is branch retinal vein occlusion (BRVO)? EyeSmart. American Academy of Ophthalmology. November 2023.
Retinal macroaneurysm. StatPearls [Internet]. August 2023.
What are macular neovascular membranes (MNV)? EyeSmart. American Academy of Ophthalmology. November 2023.
Neovascularization: A small solution to a big problem. Review of Optometry. May 2022.
Vitreous hemorrhage. StatPearls [Internet]. August 2023.
Glaucoma. National Eye Institute. November 2023.
Exudative retinal detachment. EyeWiki. American Academy of Ophthalmology. March 2024.
Hypertension. World Health Organization. March 2023.
Page published on Monday, October 31, 2022
Page updated on Tuesday, August 20, 2024
Medically reviewed on Thursday, June 27, 2024






