Scleritis
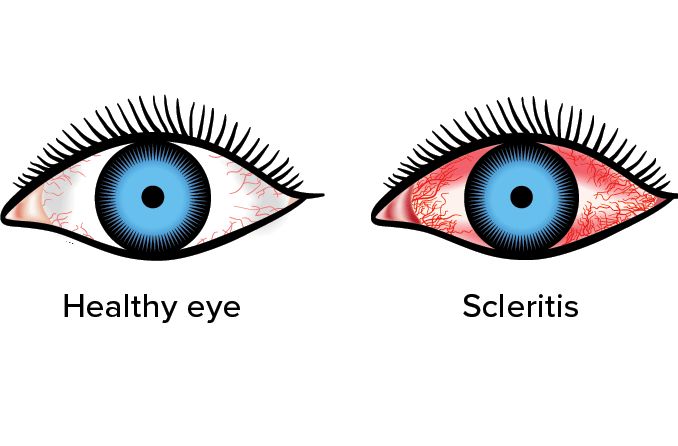
If the whites of your eyes become inflamed, you may have scleritis. This is a tricky diagnosis, however, for many reasons related to the external layers of the eyeball and the body’s natural immune defenses.
Scleritis can point to serious eye problems. In rare cases, it may cause permanent vision loss. To sort it all out, you need answers to several questions:
How do we define scleritis?
What do the symptoms of scleritis look and feel like?
Why does scleritis happen?
Which varieties of scleritis are most likely?
Which eye diseases are similar to scleritis?
What are the common treatments for scleritis?
Let’s work our way through quick answers to these questions:
What’s the medical definition of scleritis?
Sclera is the medical term for the whites of the eyes.
The sclera is made up of strong, dense tissues that keep your eyeballs round and protect the delicate parts within the eye that make vision possible. The sclera starts on the front side of the eyeball, where it connects to the cornea. It goes all the way to the back of the eye to the connection point with the optic nerve.
Scleritis happens when there’s inflammation in the sclera. Women are more likely to have scleritis, which happens most often in ages from the 30s through the 50s.
The outer surface of the eye (aside from the cornea) has three primary layers:
Sclera, at the bottom.
Episclera, on top of the sclera.
Conjunctiva, on top of the episclera.
Naturally, there’s a different medical term for inflammation in each of these layers. We’ll explore these conditions in the question below about diseases similar to scleritis.
Next up, however, we’ll take a look at the symptoms resulting from inflammation of the sclera.
What are the symptoms of scleritis?
How can you tell if you have scleritis? The most common symptoms are:
Sharp, piercing eye pain that can radiate out into the face. Often, the pain develops over several days.
Swelling and redness (bloodshot eyes). Doctors look for a blue cast to the redness to distinguish scleritis from other conditions.
Excessive tears.
Why would you have these symptoms? Let’s find out.
What causes scleritis?
The body’s immune system is one of the most common causes of scleritis. The immune system is supposed to fight off germs and prevent diseases, but it occasionally develops quirks that cause inflammation throughout the body. This includes the eyes.
Thus, autoimmune diseases such as lupus, rheumatoid arthritis, scleroderma and granulomatosis are often connected to outbreaks of scleritis.
Injuries and infections also may trigger scleritis, but they are far more rare.
Scleritis also reflects the sclera’s unique biological structure. There’s little blood in the sclera because it has few blood vessels (though it does have a large quantity of sensory nerves). The sclera draws nutrients from other channels called the choroid and episcleral vascular complexes.
The tissues of the sclera are weaved together like a web that helps make it strong. But the lack of blood vessels makes it tough to get rid of toxins and germs. That’s basically a breeding ground for inflammation.
What are the most common varieties of scleritis?
The type of scleritis determines how doctors decide how to treat it. The primary classifications come from the locations on the eyeball
Anterior scleritis – Inflammation in the front surface of the sclera. Keratitis, or inflammation of the cornea, may show up along with anterior scleritis. This is the easiest to diagnose because the doctor can see it unobstructed.
Posterior scleritis – Inflammation in the rear surface of the sclera. Posterior scleritis is more difficult to diagnose because the doctor cannot easily see the rear of the eyeball. Posterior scleritis can lead to vision loss because the back side of the sclera connects to the optic nerve. Inflammation and swelling near the optic nerve can interrupt the transmission of visual information to the brain.
Scleritis also comes in three varieties classified by how they attack the eyeball.
Diffuse scleritis – Inflammation across the surface of the sclera. This is the most common kind of scleritis.
Nodular scleritis – Distinct nodules in specific areas of the sclera. These raised areas can cause severe pain.
Necrotizing scleritis – A tissue-destroying variant of scleritis. Necrotizing scleritis is the most dangerous variant because it’s essentially killing eyeball tissue. Indeed, it can cause loss of an eye in the most severe cases. Extreme pain is typical.
All of these variants underscore the complexity of diagnosing scleritis. And there’s more: Doctors have to make sure they’re not confusing it with similar conditions.
Which eye diseases are similar to scleritis?
Because scleritis happens on the bottom layer of the sclera — below the episclera and the conjunctiva, it’s easy to confuse it with nearby problems. These are the three biggest points of confusion:
Scleritis vs. episcleritis
The episclera is a thin layer above the sclera. Thus, episcleritis usually means inflammation, pain and redness in this layer. Moreover, the autoimmune diseases that cause scleritis also tend to cause episcleritis.
The main difference is that episcleritis is usually harmless and goes away on its own. By contrast, scleritis attacks the surface of the sclera and is a more serious condition. It causes more pain and swelling and may lead to blurry vision and other problems.
Scleritis vs. conjunctivitis
The conjunctiva is the layer above the sclera. Conjunctivitis (commonly called pink eye) is inflammation leading to redness, itchiness and other symptoms, depending on the cause.
Allergies and infections are the most common causes of conjunctivitis. Bacterial infections may create a green or yellow discharge in the corner of the eye. Allergic conjunctivitis may cause watery eyes.
Both conditions may cause redness, but conjunctivitis is less likely to cause pain and cloudy vision. Moreover, if the patient has autoimmune conditions, scleritis may be more likely. A doctor has to weigh all these factors when making a diagnosis.
Scleritis vs. uveitis
Inflammation may strike the uvea, a layer beneath the sclera, leading to uveitis. The uvea has three parts:
The iris, the colored part of the eye, which filters light reaching the retina.
The ciliary body, which controls the pupil and adds liquid to the interior of the eyeball.
The choroid, which lies between the sclera and the retina.
Uveitis has many of the same symptoms as scleritis, including redness and blurry vision, but it has many subtle differences. An eye doctor who sees these conditions frequently can tell them apart.
Scleritis treatment
Because scleritis can damage vision if left untreated, it’s imperative to get symptoms checked as soon as possible.
Doctors start by examining your eyes with a slit lamp. This helps distinguish between scleritis and other kinds of inflammation. You may also be tested to check for signs of autoimmune disease.
If you’re already being treated for a condition like rheumatoid arthritis, your doctor will coordinate your treatment with your rheumatologist. Similarly, if an injury or infection is related, your eye doctor will work with your other doctors.
Treatment may include corticosteroids, which reduce inflammation. You might also take over-the-counter anti-inflammatories like aspirin or ibuprofen. Eye drops and antibiotics might be used if there’s an infection.
Depending on the seriousness of your case, you might have to take immune-suppressing medications.
The most serious cases of scleritis may thin the sclera and threaten to punch through it. This may require surgery that grafts sclera tissue onto these thin points.
SEE RELATED: Blue sclera
When to see a doctor about scleritis
Contact an eye doctor right away if you’re experiencing the symptoms outlined here. The sooner you figure out what’s going on, the better off your vision will be.
Page published on Wednesday, February 24, 2021




