Symblepharon
What is symblepharon?
Symblepharon is a condition that affects the conjunctiva — the membrane that protects the eye. It can occur as a result of inflammatory diseases, conjunctival infections or trauma. Cases range from mild to severe. There is a possibility that symblepharon can threaten your sight.
Cats can also experience symblephara. They occur between the conjunctiva, cornea and the third eyelid. In cats, they are caused by a herpesvirus infection.
Signs and symptoms
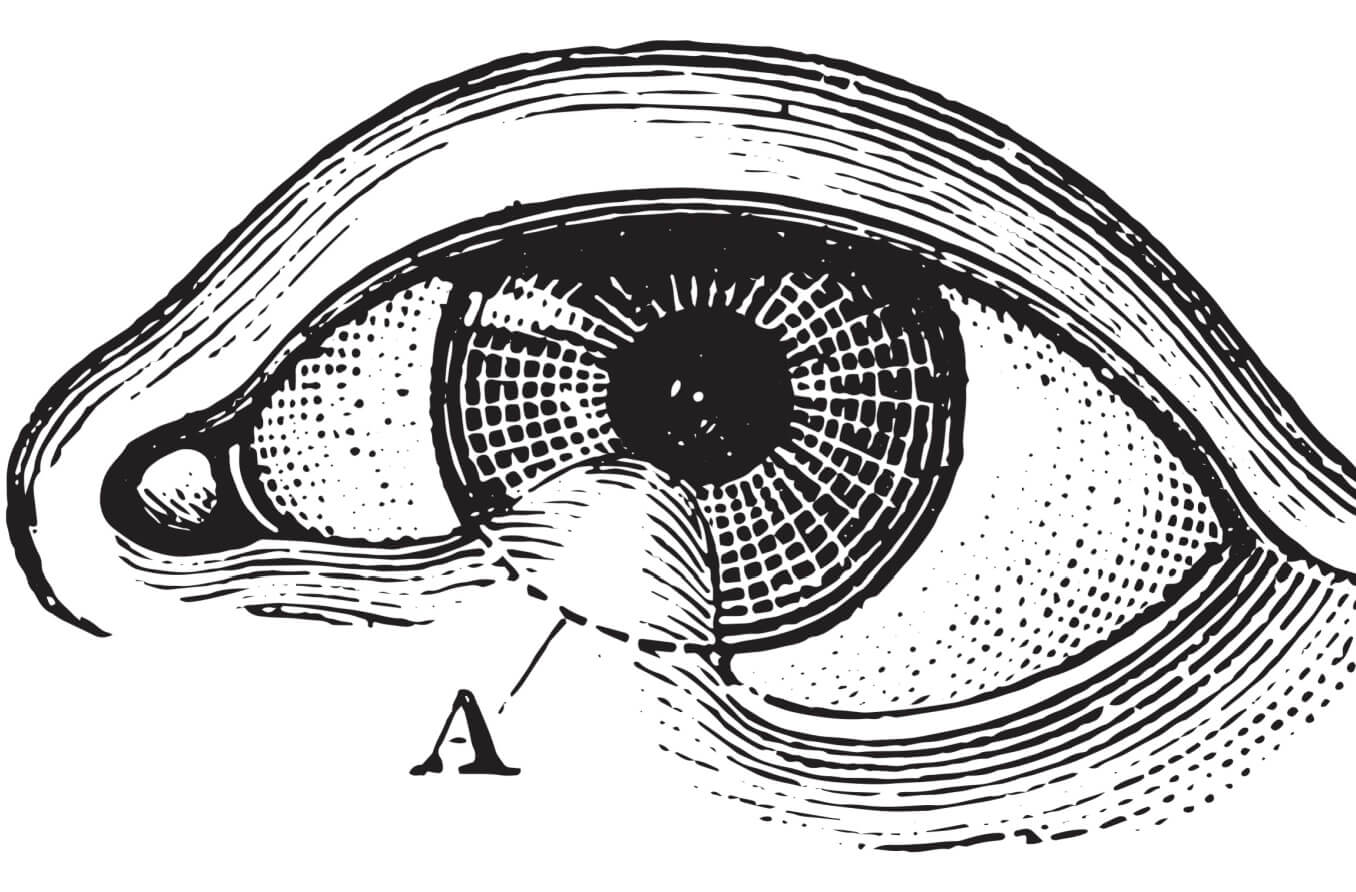
Symblepharon occurs when an adhesion forms between two parts of the conjunctiva: the palpebral conjunctiva and the bulbar conjunctiva. The palpebral conjunctiva lines the eyelids. The bulbar conjunctiva covers the eyeball.
During the healing process from a disease, infection or injury, protective epithelial cells can be lost from these two areas of the conjunctiva. This can cause an abnormal adhesion, resulting in symblepharon.
If the adhesion is small, there may not be any issues with eye movement (ocular motility). However, if the adhesion is larger, ocular motility problems may be present.
Depending on the severity of the condition, a variety of other symptoms may include:
Burning
Light sensitivity
Vision problems
Diplopia – double vision
Entropion – a condition in which the eyelid turns inward toward the eyeball
Lagophthalmos – the inability to properly close the eyelid
In severe instances, the conjunctiva fornix may become damaged. The conjunctiva fornix is the area of the conjunctiva where the palpebral and bulbar conjunctiva converge. This can lead to more blinking than usual, and the eye may be unable to retain tears. Keratinization of the surface of the eye can result.
Causes
Because damage from trauma can cause the eye to heal in an abnormal way, this can cause symblepharon. Types of trauma include: chemical or thermal burns, as well as burns caused by fireworks.
Conjunctival infections are another possible cause of symblephara. These infections include different types of conjunctivitis and keratoconjunctivitis, such as:
Chlamydial conjunctivitis
Chlamydial conjunctivitis is a sexually transmitted disease in which bacteria can infect the eye.
Trachoma
Trachoma is spread by a similar bacterium as the one that causes chlamydial conjunctivitis but is not a sexually transmitted disease. It can be spread through person-to-person contact or by flies.
It is uncommon in Europe and North America but common everywhere else in the world, especially in poorer communities.
Epidemic keratoconjunctivitis (EKC)
EKC is a viral infection that can affect the surface of the eye. It can affect the gastrointestinal tract and respiratory system as well.
EKC can cause the formation of a membrane on the part of the conjunctiva that is on the inside of the eyelid. This membrane requires careful treatment by an eyecare professional to avoid symblepharon formation.
Vernal keratoconjunctivitis
Vernal keratoconjunctivitis is a disease that causes small bumps on the conjunctiva. It is more commonly found in males in tropical climates. But it is also not uncommon in the U.S., including in the north.
Atopic keratoconjunctivitis
Atopic keratoconjunctivitis is a chronic disease that affects those with atopic dermatitis. Also known as eczema, atopic dermatitis is an inflammatory skin disease.
Bacterial conjunctivitis
This is an infection of the conjunctiva caused by bacteria. It is one of the most common eye problems and can be prevented with good hygiene.
Herpes zoster
Herpes zoster is a virus that causes shingles. It can cause symblepharon when it infects the surface of the eye.
There are also a variety of diseases and other conditions that can cause ocular inflammation, leading to symblephara. These include:
Stevens-Johnson syndrome and toxic epidermal necrosis (SJS/TEN)
These are skin conditions caused by infections or allergies to medications that cause rashes and blisters. These symptoms can lead to the skin peeling.
Both are serious conditions that can also affect the eyes. Blisters can form on the eyes and mucus membranes. The blisters can then seal the eyes shut. Other ocular complications can include the formation of symblephara.
Ocular cicatricial pemphigoid (OCP)
OCP is an autoimmune disease that affects the conjunctiva and eyelids. Besides symblepharon, a patient with OCP can develop ankyloblepharon — the upper and lower eyelids fusing together. This disease may lead to blindness if left untreated.
Mucous membrane pemphigoid (MMP)
When other mucous membranes than those in the eye are affected, it is called MMP. In about 60% of cases of MMP, the eye is involved — OCP — and symblepharon is a possibility.
Erythema multiforme
Erythema multiforme is a condition that involves skin lesions. These lesions are often caused by the herpes virus. It can also affect the membranes of the eyes potentially causing symblephara.
Graft-versus-host disease (chronic)
This is a disorder that can occur after a bone marrow or stem cell transplant. The transplanted cells attack the recipient’s body. It can affect your gastrointestinal tract, liver, skin and the surface of your eye.
Granulomatosis with polyangiitis (GPA)
GPA is a rare inflammatory disease that affects the blood vessels and tissues. This results in damage to the organ systems of the body. Inflammation can also affect the eyes and cause symblepharon.
Recessive dystrophic epidermolysis bullosa
This is a disease that produces blisters in and on the body, including the eyes. It can lead to vision loss.
Sarcoidosis
Sarcoidosis is a condition that occurs when your immune system overreacts and causes granulomas, or lumps, to form on the body. These lumps can form in places like the lungs, the heart, on your skin and also in the eye.
Vitamin A deficiency
This condition can occur due to poor nutrition and also after gastric bypass surgery. Symblephara can be present along with night blindness and are also used to diagnose Bitot spots (deposits on the whites of the eyes).
Most cases of symblepharon are acquired. Though there are some instances in which it is present at birth (congenital). This has been seen in those with cryptophthalmos. This is a hereditary disease that causes ankyloblepharon and usually results in blindness.
Complications
When symblepharon forms, serious complications can arise due to the adhesion. These include, but are not limited to:
Double vision
Inhibited eyelid function
Limited eye movement
Dry eye syndrome
Vision loss, if the symblepharon grows over the cornea
Treatment and prevention
Treating underlying conditions and diseases is important in managing and preventing symblephara. For those with autoimmune diseases, your doctor may prescribe certain medications. Immunomodulators and immunosuppressive drugs adjust the response of the immune system. This can lessen inflammation. Steroids can also be used to reduce inflammation.
Because symblepharon can cause dry eye, your doctor may prescribe preservative-free eye drops. They may also prescribe eye lubricants. These medicines can be used to manage dry eye irritation.
A surgeon may also perform surgery to treat symblepharon. These procedures can include:
Tissue grafting and reconstruction of the conjunctiva fornix – A surgeon takes living tissue from another part of the body. They then reconstruct the conjunctiva fornix.
Limbal stem cell transplantation – This procedure helps heal the epithelial layer on the surface of the eye. It is for patients with symblepharon resulting from a burn.
Oculoplastic surgery – Also known as eyelid surgery, this type of surgery is done to release the symblepharon.
Amniotic membrane application – amniotic membranes prepared from human placentas can be placed on the eye for several days to help it heal.
When to see a doctor
In mild cases, you may not have any symptoms. However, if you have a conjunctival infection or any of the underlying diseases listed above, it is important to see your doctor. They can start treatment to help prevent symblepharon. Also, if there has been any trauma to or a burn on your eye, make an appointment with your doctor right away.
Symblepharon. EyeWiki. American Academy of Ophthalmology. April 2023.
Conjunctiva. Cleveland Clinic. October 2022.
Application of superficial keratectomy and soft contact lens for the treatment of symblepharon in a cat: a case report. Journal of Veterinary Science. February 2021.
Anatomy, head and neck, eye conjunctiva. StatPearls. August 2022.
Diplopia (double vision). Cleveland Clinic. December 2021.
Lagophthalmos. StatPearls. April 2023.
Adult inclusion conjunctivitis. Merck Manual Professional Version. April 2023.
Trachoma. Mayo Clinic. October 2020.
Epidemic keratoconjunctivitis. EyeWiki. American Academy of Ophthalmology. June 2023.
Symblepharon. Vagelos College of Physicians and Surgeons. Accessed June 2023.
Vernal keratoconjunctivitis. StatPearls. May 2023.
Atopic keratoconjunctivitis. EyeWiki. American Academy of Ophthalmology. March 2023.
Atopic dermatitis. National Institute of Arthritis and Musculoskeletal and Skin Diseases. November 2022.
Bacterial conjunctivitis. EyeWiki. American Academy of Ophthalmology. November 2022.
A practical guide to Herpes zoster. Ophthalmology Management. July 2020.
Stevens-Johnson syndrome. Cleveland Clinic. December 2020.
Ocular pemphigoid. StatPearls. March 2023.
Ocular cicatricial pemphigoid. EyeWiki. American Academy of Ophthalmology. January 2023.
Ocular citatrical pemphigoid - mucous membrane pemphigoid. Johns Hopkins Medicine. Accessed June 2023.
Cicatricial pemphigoid. StatPearls. April 2023.
Ocular pemphigoid. StatPearls. March 2023.
Erythema multiforme. StatPearls. May 2023.
Graft vs. host disease. Cleveland Clinic. February 2023.
Graft-versus-host disease. StatPearls. October 2022.
Granulomatosis with polyangiitis. Cleveland Clinic. July 2019.
Severe generalized recessive dystrophic epidermolysis bullosa. Genetic and Rare Diseases Information Center. February 2023.
Sarcoidosis. Cleveland Clinic. January 2023.
Cryptophthalmos. University of Arizona Health Sciences. Accessed June 2023.
Limbal stem cell transplantation. Vagelos College of Physicians and Surgeons. Accessed June 2023.
Oculoplastic surgery - eyelid surgery. Stanford Medicine. Accessed June 2023.
Page published on Wednesday, July 5, 2023
Page updated on Tuesday, July 11, 2023
Medically reviewed on Wednesday, June 21, 2023






