15 keratopathies: Causes, symptoms and treatment
What is keratopathy?
The term keratopathy comes from the root words kera, meaning cornea, and pathy, meaning disease. It refers to a group of diseases of the cornea with a vast array of underlying causes and mechanisms. Some forms of keratopathy are due to an eye condition. Others are due to a systemic condition.
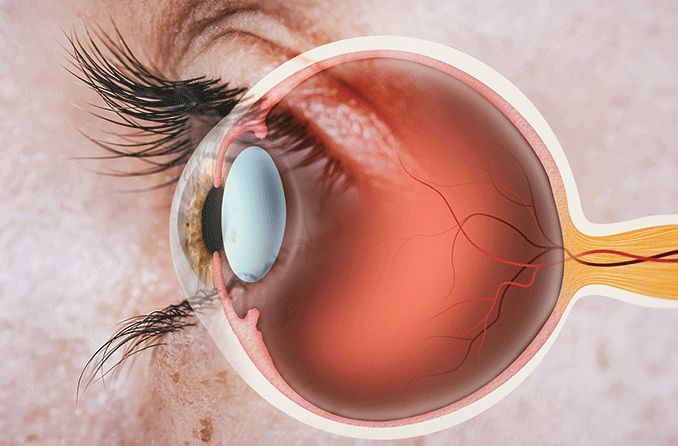
The five layers of the cornea
The cornea is the clear, dome-shaped outer layer of the eye. It plays a critical role in vision — providing the majority of the focusing power of the eye. It is also a barrier to germs and particles, helping to prevent infection and injury.
The corneal diseases that lead to keratopathy cause damage to one, or several, layers of the cornea. This may lead to inflammation, irritation, redness, pain, clouding or scarring of the cornea, and reduced vision.
The five layers of the cornea are:
Epithelium –The outer barrier layer absorbs nutrients and oxygen from tears. It can regenerate in about two weeks. It is sensitive to pain and touch due to its many nerve endings. The epithelium is attached to the rest of the corneal layers by a basement membrane.
Bowman’s layer – The clear, protective layer is composed of collagen. Injury to this layer can result in permanent scarring of the cornea.
Stroma – This middle layer provides 90% of the cornea’s thickness. It supports the cornea’s structure and elasticity. The endothelium helps to regulate its water absorption, thus keeping it transparent.
Descemet’s membrane – This protective membrane is made of collagen fibers.
Endothelium – This layer of cells keeps the stroma from absorbing too much fluid and becoming hazy. It does this by pumping excess water out of the stroma.
Following is an outline of 15 types of keratopathy, as well as their signs, symptoms and treatment options:
1. Superficial punctate keratitis (keratopathy)
Superficial punctate keratitis (SPK) is a type of keratopathy that causes damage to small pockets of epithelial cells. It is commonly seen in corneal inflammation. It can occur due to a number of issues and conditions, including:
Poorly fit contact lenses
Incomplete lid closure (lagophthalmos)
Allergic reaction to ingredients in eye drops, particularly preservatives
Mechanical irritation to the eyes by an eyelash
Viral or bacterial infection
Thygesons (a rare, chronic eye disease that causes SPK in both eyes)
Punctate epithelial keratitis (PEK), or epithelial keratopathy, is quite similar to superficial punctate keratitis (SPK). They are both types of epithelial defects. This means that they both indicate that the epithelial layer of the cornea is damaged. But their appearance is slightly different.
Signs and symptoms
An eye doctor is able to see SPK with the use of a dye, such as fluorescein. Then they observe the eye using a slit lamp, an instrument that provides high magnification to allow a close look at the eye. The dye stains the damaged areas of the epithelium so that they are visible. The location of the staining, in addition to a patient’s history, can help an eye doctor narrow down the cause of SPK.
SPK commonly occurs with additional symptoms such as light sensitivity, red eye, discomfort and mild blurry vision.
Treatment
SPK usually heals completely once the underlying condition is treated. Since there are so many conditions that can cause SPK, the treatment will depend on the cause.
Bacterial infections will require antibiotics.
Contact lens wearers may be asked to stop wearing contact lenses til the cornea heals, and new contact lenses may be prescribed.
Dry eye patients may require moisture therapy such as artificial tears and ointments.
Viral infections do not have any treatment, aside from comfort measures.
READ MORE: Keratitis: Inflammation of the cornea
2. Ultraviolet keratopathy (photokeratitis)
Ultraviolet (UV) keratopathy, or photokeratitis, is the result of damage to the cornea from exposure to UV radiation. Although, in most cases, only the epithelial layer is damaged, studies have found that the deeper layers can also be damaged with prolonged exposure.
Photokeratitis can be caused by sunlight. It can also be caused by artificial sources such as arc welding, metal halide lights, UV germicidal lamps and tanning beds.
Eye damage from sunlight can occur if someone looks directly at a solar eclipse without protection. It can also occur from exposure to UV radiation reflecting off snow at high altitudes (“snow blindness”).
Artificial sources are more common sources for photokeratitis and require shorter periods of exposure to cause damage.
Signs and symptoms
It typically takes from half an hour to about 12 hours after exposure to begin experiencing symptoms of photokeratitis. Vision is typically only mildly reduced.
Additional symptoms include:
Discomfort or pain in both eyes
Light sensitivity
Tearing
Difficulty keeping the eyes open
The cornea may also appear red with signs of superficial punctate keratitis. It may also begin to swell, and there may be some inflammation in the eye.
Treatment
The first step is to avoid further exposure to UV radiation. In addition, artificial tears and pain medication may be prescribed. People who wear contact lenses will need to discontinue for a couple of weeks. Typically, the corneal epithelium will heal in 24 to 72 hours.
3. Band-shaped keratopathy (BSK or band keratopathy)

Band-shaped keratopathy is a corneal degeneration. It causes calcium to deposit in the outer layers of the cornea, particularly in Bowman’s layer.
It is often the result of an underlying medical condition, such as an autoimmune disease or kidney disease. It can also result from a chronic eye condition or eye surgery. In some cases, there are no identifiable causes.
Signs and symptoms
This condition appears as a white/gray band across the cornea. Vision can be reduced, with a greater loss of visual acuity occurring as the disease progresses. The eyes can also feel irritated and appear red.
Treatment
For mild cases, artificial tears can be used to manage symptoms. In some cases, superficial keratectomy with chelation may be necessary. This is a procedure that removes calcium from the cornea.
4. Striate keratopathy
Striate keratopathy after cataract surgery is a temporary and fairly common condition. The edema (swelling) and Descemet’s folds typically clear up in a few days.
Signs and symptoms
Corneal edema in addition to the presence of folds in Descemet’s membrane are a common sign. Vision may be slightly blurry and hazy for a few days.
Treatment
A hypertonic solution may be used to reduce edema. Additionally, topical steroids can be prescribed to decrease inflammation.
5. Neurotrophic keratopathy
Neurotrophic keratopathy is characterized by decreased corneal sensation. It can occur as a result of damage to the fifth cranial nerve due to an eye disease or injury. It can also be the result of an underlying systemic condition.
Causes can include:
Herpes keratitis
Damage to the cornea from surgery, trauma, burns or improper contact lens use
Systemic conditions such as diabetes, multiple sclerosis or leprosy
Signs and symptoms
Reduced or absent corneal sensitivity
Reduced production of reflex tears
Vulnerability to injury due to poor healing.
It is classified into three stages depending on the severity of corneal damage:
Stage 1 – Dry, cloudy epithelium with some corneal swelling
Stage 2 – The upper half of the cornea has round areas of epithelium loss
Stage 3 – The cornea has developed an ulcer; the stroma is breaking down (corneal melting) and may progress to a perforation (a hole in the cornea)
Treatment
Early management includes monitoring the eye and use of artificial tears. If the disease progresses to stage 3, antibiotics may be prescribed. This would be in addition to special medications that help to maintain the integrity of the cornea. If this is not effective, surgery may be recommended.
6. Metabolic keratopathy
Metabolic keratopathy is caused by the abnormal accumulation of proteins, carbohydrates or fats in the cornea due to a wide array of metabolic disorders.
A metabolic disorder occurs when your body is not able to process proteins, carbohydrates or fats properly. It happens because the enzymes needed for chemical reactions in the body are defective.
Some systemic diseases that can lead to metabolic keratopathy include:
Diabetes
Lysosomal storage disorders
Lipid & lipid metabolism disorders
Amino acid, nucleic acid, and protein metabolism disorders
Signs and symptoms
Metabolic keratopathies usually affect both eyes and progress over time. They affect both the central and peripheral parts of the cornea and can involve several layers of the cornea. Signs and symptoms vary widely depending on the underlying systemic disease.
Treatment
Due to the large variation in type and causes of metabolic keratopathies, treatment will vary. The first step is to manage the underlying condition.
READ MORE: Diabetes and eyesight: Symptoms, treatments and eye exams
7. Bullous keratopathy
Bullous keratopathy is due to damage or reduction of the corneal endothelial cell. The endothelial layer pumps water out of the stroma to keep it dehydrated and clear. When the endothelial cells are not able to accomplish this, the stroma (and therefore the cornea) swells.
Some conditions that lead to bullous keratopathy are Fuchs corneal endothelial dystrophy and injury to the corneal endothelium.
Injury to the endothelium may occur during an eye surgery, such as cataract surgery. As a result, bullous keratopathy can be referred to based on the presence of an intraocular lens:
Pseudophakic bullous keratopathy – Also referred to as pseudophakic corneal edema. This is the development of bullous keratopathy, or irreversible corneal edema, that occurs after cataract surgery when an intraocular lens is placed in the eye.
Aphakic bullous keratopathy – Also referred to as aphakic corneal edema. This is bullous keratopathy that occurs after cataract surgery when an intraocular lens is not placed in the eye.
Signs and symptoms
Corneal edema resulting in loss of transparency of the cornea can occur. This leads to blurry, hazy vision. In particular, vision is worse in the morning when the corneal edema has increased overnight.
Treatment
An eye doctor may prescribe the following treatments to manage bullous keratopathy:
Hypertonic drops or ointments to decrease swelling of the cornea (such as sodium chloride 5%)
Medicine that lowers intraocular pressure
Contact lenses that provide therapeutic relief
Antibiotic drops if an infection is present
READ MORE: Fuchs' corneal dystrophy: 7 things you should know
8. Vortex/whorl/hurricane keratopathy (cornea verticillata)
Vortex keratopathy is due to medications or other substances deposited in the epithelial layer of the cornea. It is associated with certain medications as well as some diseases. One such disease is Fabry disease, which causes a buildup of fat in the body’s cells.
One study found that neurotrophic keratitis was a leading cause of vortex keratopathy.
Common medications that can cause vortex keratopathy include:
Amiodarone (for treatment of irregular heartbeat)
Chloroquine and hydroxychloroquine (for prevention and treatment of malaria)
Phenothiazines (for treatment of psychiatric disorders)
Indomethacin (for treatment of pain and inflammation)
Signs and symptoms
There are usually no visual symptoms or eye discomfort caused by this condition. In rare cases, an individual may notice halos or rings with a blue or green tinge. Vertex keratopathy presents as a brownish or gray pattern on the cornea resembling a vortex or whorl.
Treatment
In general, there is no recommended treatment for this condition as it does not cause problematic symptoms.
9. Exposure keratopathy
Incomplete closure of the eyelids, insufficient blink rate or reflex, and an unstable tear film can disrupt the corneal surface. This results in exposure keratopathy. Typically, the corneal surface is protected by the eyelids and tear film. When this protection is compromised, the cornea can become damaged.
Signs and symptoms
There are a number of conditions that can cause the corneal surface to be exposed for an extended period of time. This can lead to the following symptoms:
Foreign body sensation
Blurry vision that comes and goes
Excessive tearing
Pain
In some cases, exposure keratopathy can result in edema, thinning or even ulceration.
Treatment
Treatment consists of management of the underlying condition causing corneal exposure. Artificial tears and overnight ointment are also frequently prescribed. In addition, strategies such as punctal plugs, eyelid taping or eyelid patching may be considered.
SEE RELATED: Pfeiffer syndrome and Apert syndrome
10. Filamentary keratopathy
Filamentary keratopathy is an uncommon condition that results in strands, or filaments, in the cornea. These filaments are made of broken-down epithelial cells and mucus. They are usually due to an unstable tear film and changes in the surface of the cornea.
Conditions that may cause filamentary keratopathy include dry eye, toxicity from certain medications or overuse of contact lenses. A chronic case may indicate the presence of an underlying condition such as rheumatoid arthritis, Sjögren’s syndrome or thyroid disease.
Signs and symptoms
In addition to filaments and mucus in the cornea, this condition can present with an unstable tear film, redness, reduced corneal sensitivity, SPK and epithelial erosion. (Epithelial erosion is when the outermost corneal layer, the epithelium, does not adhere properly to the underlying layers.)
An individual with filamentary keratopathy may experience the following symptoms:
Feeling that something is in the eye, grittiness or general discomfort in the eye
Light sensitivity
Blurry vision
Excessive tearing
Blepharospasm (twitching or difficulty keeping the eyes open)
Treatment
Treatment for filamentary keratopathy can be difficult as it is often chronic. Managing the underlying condition is often the most successful route to treatment. Additionally, symptoms for discomfort can be treated with eye drops such as artificial tears.
SEE RELATED: Acanthamoeba keratitis: What contact lens wearers need to know
11. Crystalline keratopathy
Crystalline keratopathy is a rare keratopathy that presents with white or gray crystal-like opacities in the stromal layer of the cornea.
It can occur in the cornea of an individual who is immunocompromised or has an underlying eye or systemic disease. It is sometimes seen in people who have used steroid eye drops for a long time. It can also appear months or years after an individual has had a corneal transplant.
When infection is the cause, it is referred to as infectious crystalline keratopathy. A number of different bacteria or fungi can be responsible. The most common being Streptococcus bacteria species.
Signs and symptoms
The eye may appear red and irritated. White or gray crystal-like opacities will be present in the stromal layer of the cornea. In cases of infectious crystalline keratopathy, a biofilm, a layer of secretions by the bacteria or fungi that has caused the infection, may be present.
Symptoms include:
Slight discomfort to mild or severe pain
Blurry vision
Light sensitivity
Red, irritated eye
Inflammation
Treatment
This condition often does not respond to treatment with drugs. Doctors believe that this is due to the biofilm that develops in cases of infectious crystalline keratopathy. In a number of cases, a corneal transplant (or keratoplasty) may be necessary.
12. Radiation keratopathy
Radiation keratopathy is a complication of radiation therapy. It can cause dry eye syndrome and an unstable tear film, leading to damage to the cornea from the severe dryness. Lacrimal glands, which produce tears, can be damaged during radiation. Corneal edema (swelling) has also been reported.
According to reports, nearly one in four patients who undergo radiation therapy experience corneal complications.
Signs and symptoms
Severe dryness after undergoing radiation therapy is a commonly reported symptom. Dry eye symptoms include a burning or scratching feeling, redness, light sensitivity and contact lens intolerance, and blurry vision.
Treatment
Treatment of dry eye syndrome is typically how this condition is managed. This includes artificial tears, gels and ointments. For more severe cases, anti-inflammatory medications, nutritional supplements, punctal plugs, eye shields and other dry eye treatments may be used.
13. Climatic droplet keratopathy
Climatic droplet keratopathy is a corneal degeneration that results in golden-colored droplets in the outer layers of the cornea. It is also known as spheroidal keratopathy. It also goes by a number of other names, such as Labrador keratopathy, depending on geographic location.
It is most commonly seen in rural men with a high degree of lifetime exposure to UV rays, particularly from light that is reflected off snow, ice or sand. It is not completely clear why this condition occurs. Some scientists suspect it may be due to an accumulation of plasma proteins.
Signs and symptoms
This condition can be recognized by golden-yellow globules found in the cornea. In general, there are no symptoms that develop from climatic droplet keratopathy unless globules accumulate in the center of the cornea. If this occurs, an individual may experience blurry vision.
Treatment
Most people do not require treatment as this condition usually does not have symptoms. In severe cases in which vision is affected, corneal transplant may be required. The management typically involves reducing sun exposure to slow down the progression of the disease.
14. Lipid keratopathy
This is a rare keratopathy that is thought to be a corneal degeneration in which lipids (fats) are deposited in the cornea. It may occur in the primary form, meaning that there is no underlying cause. This is not very common. Typically, lipid keratopathy is secondary to a systemic condition that affects the body’s ability to metabolize fats. A previous eye injury or disease such as ocular herpes or interstitial keratitis may also be an underlying cause.
Signs and symptoms
An individual with lipid keratopathy will experience a progressive decrease in visual acuity. This is the result of lipids in the cornea causing opacification. The fat deposits may be observed during an eye exam with a slit lamp.
Additionally, abnormal blood vessels may grow into the normally avascular (no blood vessels) cornea (corneal neovascularization). The corneal tissue may also begin to thin.
Treatment
Since most cases of lipid keratopathy are secondary to a systemic disease, the primary goal is to manage the underlying condition. If any abnormal blood vessel growth is detected in the cornea, it must also be treated surgically or medically.
15. Congenital aniridia-associated keratopathy
Congenital aniridia-associated keratopathy (AAK) causes changes in the cornea due to limbal stem deficiency. It occurs in 90% of individuals with aniridia. Aniridia is a rare, genetic condition that results in a partly or fully missing iris (the colored part of the eye). In addition, people with aniridia have decreased visual acuity and are very light sensitive.
AAK is the second most common cause of progressive loss of visual acuity in individuals with aniridia. This is largely due to abnormal growth of blood vessels into the central cornea.
Signs and symptoms
Keratopathy symptoms can begin to appear by age 10, but more commonly appear in the third decade. Aniridia can be associated with a number of genetic conditions that present with many eye and systemic complications.
Symptoms often seen with keratopathy associated with aniridia include:
Increased thickness of the central cornea
Growth of abnormal blood vessels in the cornea
Opacification of the cornea
Fibrosis of the cornea
Vulnerability to recurrent corneal erosions, chronic inflammation and ulcers
Treatment
Treatment will depend on the severity of keratopathy. Mild cases are managed with artificial tears (preservative-free). The more severe stages of keratopathy will require specialized serums and transplants.
Can I prevent keratopathy?
Some types of keratopathy are caused by inherited conditions and cannot be prevented. But, you can decrease your risk of other types of keratopathy. For example, you can reduce the risk of keratopathy caused by injury or UV radiation by wearing protective eyewear.
In addition, maintaining a healthy lifestyle decreases your risk of heart disease and diabetes. Lowering your risk of developing these conditions will improve your overall eye health.
Some additional ways that you can decrease your risk of corneal keratopathy include:
Use safety goggles when there is a risk of eye injury.
Wear sunglasses to protect from UV radiation.
Decrease your risk of diabetes by not smoking and maintaining a healthy weight.
Eat a healthy diet rich in Vitamin A and omega-3 fatty acids.
If you wear contact lenses, follow your doctor’s guidelines regarding wear and care.
Finally, stay current with your annual comprehensive eye exams. If you notice persistent eye pain or blurry vision, contact an eye doctor as soon as possible.
READ NEXT: What Is a corneal descemetocele? and Corneal deposits
Anatomy of cornea and ocular surface. Indian Journal of Ophthalmology. February 2018.
Cornea: Guide your way through SPK. Optometric Management. December 2018.
Superficial punctate keratitis. Merck Manuals Professional Edition. May 2020.
A closer look at corneal inflammation. Review of Cornea and Contact Lenses. November 2012.
Ultraviolet keratitis. University of Iowa Health Care Ophthalmology and Visual Sciences. February 2022.
Photokeratitis. American Academy of Ophthalmology. EyeWiki. February 2022.
A hands-on approach to band keratopathy. Review of Optometry. January 2017.
Band keratopathy. Kellogg Eye Center Michigan Medicine. February 2015.
Calcific band keratopathy. American Academy of Ophthalmology. EyeWiki. January 2022.
Keratopathy. StatPearls — NCBI Bookshelf. February 2022.
Pronounced striate keratitis following intracapsular cataract surgery. University of Iowa Health Care Ophthalmology and Visual Sciences. February 2008.
Neurotrophic keratitis: Background, etiology and pathophysiology. Medscape. September 2018.
Neurotrophic keratitis. StatPearls — NCBI Bookshelf. November 2021.
Metabolic keratopathy. American Academy of Ophthalmology. EyeWiki. January 2022.
Metabolic disorders. MedlinePlus Medical Encyclopedia. August 2016.
Postoperative corneal edema: Background, pathophysiology, epidemiology. Medscape. October 2018.
Bullous keratopathy. Merck Manuals Professional Edition. May 2020.
Pseudophakic bullous keratopathy. American Academy of Ophthalmology. EyeWiki. March 2022.
Cornea verticillata. American Academy of Ophthalmology. EyeWiki. April 2022.
Vortex keratopathy. Columbia University Department of Ophthalmology. Accessed June 2022.
Fabry disease. MedlinePlus Medical Encyclopedia. May 2022.
Etiologic profile of vortex keratopathy. Investigative Ophthalmology and Visual Science. May 2003.
Exposure keratopathy. American Academy of Ophthalmology. EyeWiki. May 2022.
Management of exposure keratopathy. American Academy of Ophthalmology. April 2014.
Exposure keratitis. Columbia University Department of Ophthalmology. Accessed June 2022.
Filamentary keratitis. American Academy of Ophthalmology. EyeWiki. October 2021.
Can you identify this condition? Canada Family Physician. July 2010.
Infectious crystalline keratopathy. American Academy of Ophthalmology. EyeWiki. January 2022.
Infectious crystalline keratopathy (ICK). University of Iowa Health Care Ophthalmology and Visual Sciences. January 2007.
Ocular complications after radiation therapy: An observational study. Clinical Ophthalmology. October 2020.
Diagnosis and treatment of radiation therapy induced ocular surface disorders. OMICS Journal of Radiology. June 20016.
Dry eye. American Optometric Association. Accessed April 2022.
Spheroidal degeneration. American Academy of Ophthalmology. EyeWiki. April 2022.
Climatic droplet keratopathy: An old disease in new clothes. Acta Ophthalmologica. January 2015.
Lipid keratopathy. American Academy of Ophthalmology. EyeWiki. January 2022.
Lipid Keratopathy: A review of pathophysiology, differential diagnosis, and management. Ophthalmology and Therapy. October 2020.
Lipid keratopathy. Columbia University Department of Ophthalmology. Accessed April 2022.
Management of congenital aniridia-associated keratopathy: Long-term outcomes from a tertiary referral center. American Journal of Ophthalmology. February 2020.
Diagnosis and management of aniridia. American Academy of Ophthalmology. November 2014.
Aniridia. MedlinePlus Medical Encyclopedia. August 2020.
Page published on Thursday, June 9, 2022






