Keratitis: Inflammation of the cornea
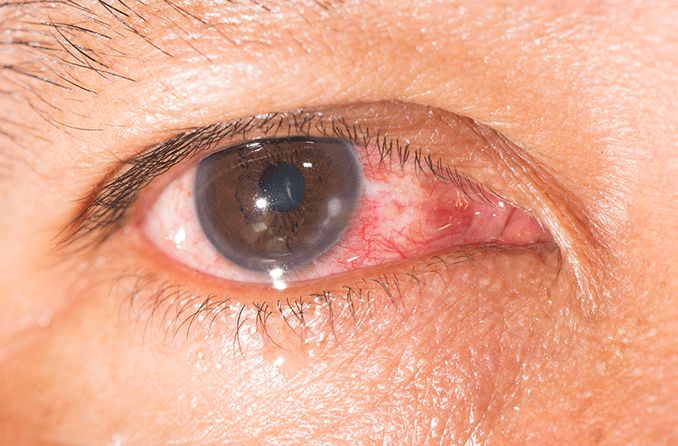
Keratitis is inflammation of the cornea (the clear front surface of the eye). Causes of keratitis include injuries, infections and diseases of the cornea, and wearing contact lenses too long. Keratitis can range from mild and temporary to severe and capable of causing permanent vision loss.
How to pronounce keratitis: “kair-uh-TIE-tis.”
Risk factors and causes
Among those who are at risk of developing keratitis are:
Wearers of contact lenses
Users of steroid eye drops
Sufferers of cold sores, chickenpox or shingles (or those who’ve had it in the past)
Sufferers of dry eye syndrome
Sufferers of eyelid disorders
People who have injured their cornea
People with reduced immunity
Causes of keratitis include:
Eye injury
Dry eye syndrome
Bacterial infection
Viral infection
Fungal infection
Parasitic infection
Allergies
Overexposure to sunlight (UV rays)
Keratitis symptoms
Symptoms of keratitis include:
Eye irritation
Feeling that something is in your eye
If you experience any of these symptoms and suspect you have keratitis, make an appointment right away with an ophthalmologist or optometrist. During the appointment, your doctor will review your medical history, perform an eye exam, and possibly take a sample of your tears or corneal cells for lab analysis.
Types of keratitis: Infectious
There are many types of keratitis. Infectious keratitis, also known as microbial keratitis, can be caused by viruses, bacteria, fungi (such as molds and yeasts) or parasites (Acanthamoeba species). Around the world, infectious keratitis is a major cause of vision impairment and blindness.
Common risk factors for infectious keratitis include wearing contact lenses, having an underlying corneal disease, suffering an eye injury or experiencing ocular surface disease (such as dry eyes).
Acanthamoeba keratitis
Acanthamoeba keratitis is rare, but it can impair your vision or even cause blindness. This type of keratitis is caused by microscopic organisms known as Acanthamoeba. These microorganisms are commonly found in bodies of water like oceans and lakes, as well as in soil or air.
This type of keratitis often affects people who wear contact lenses. Risk factors include:
Incorrect disinfection of contact lenses (such as cleaning them with tap water).
Improper storage and handling of contact lenses.
Swimming (particularly in freshwater rivers and lakes), soaking in a hot tub or taking a shower while wearing contact lenses.
Exposure to contaminated water.
History of corneal trauma.
READ MORE about Acanthamoeba keratitis
Bacterial keratitis
As the name suggests, bacteria cause bacterial keratitis. This form of keratitis can affect people who wear contact lenses along with people who don’t.
Pseudomonas aeruginosa and Staphylococcus aureus are two kinds of bacteria that can lead to bacterial keratitis. Pseudomonas aeruginosa is a leading cause of keratitis among people who wear contact lenses.
Water and soil are common places to find Pseudomonas bacteria. Meanwhile, Staphylococcus aureus bacteria can typically be found on your skin or along the lining (mucous membrane) of your nose. So-called staph infections happen frequently at hospitals and other health care facilities.
Among the risk factors for bacterial keratitis are:
Wearing contact lenses while sleeping.
Wearing rigid contact lenses overnight.
Improperly cleaning contact lenses or contact lens cases.
Storing contact lenses in water.
Rinsing contact lenses with water.
Using contact lens solution that appears to be contaminated.
Sharing contact lenses with other people (cosmetic contact lenses or otherwise).
Suffering an eye injury.
Experiencing eye disease.
Having weak immunity.
Fungal keratitis
Fungi can also cause keratitis. Among the fungi often associated with fungal keratitis are the Fusarium, Aspergillus and Candida species. Fusarium and Aspergillus are environmental fungi. Candida are yeast-like fungi that live on the body as well as inside the body (in the mouth, throat, gut or vagina, for instance).
Eye trauma — particularly trauma triggered by a plant, stick or thorn — frequently leads to fungal keratitis. Other risk factors include contact lens use, an underlying eye disease or weakened immunity.
Fungal keratitis often occurs in tropical and subtropical regions.
READ MORE about fungal eye infections
Viral keratitis
Viruses that cause viral keratitis include herpes simplex (cold sores), varicella-zoster (chickenpox and shingles) and adenovirus (upper respiratory infections, including colds). Unlike bacterial or fungal keratitis, viral keratitis can be chronic and frequent. Stress, a weakened immune system and exposure to sunlight can trigger repeated viral keratitis infections, including:
Herpes keratitis: Herpes keratitis is caused by the herpes simplex virus (HSV), which has two types. Type 1 (HSV-1) is associated with cold sores and fever blisters, and type 2 (HSV-2) is sexually transmitted. Both types can lead to eye infections, but it’s far more common for the highly contagious type 1 to spread to the eyes. According to the World Health Organization, around 3.7 billion people under age 50 (67%) worldwide have the HSV-1 infection, and around 491 million people aged 15-49 (13%) globally have the HSV-2 infection.
Herpes simplex keratitis: In the United States and other developed countries, herpes simplex keratitis is the leading cause of corneal blindness. It can also scar the cornea and decrease vision. This condition affects only one eye. Symptoms include eye redness, eye pain, blurred vision, sensitivity to light and watery discharge.
Herpes zoster keratitis: Herpes zoster keratitis happens when the varicella-zoster virus, which causes chickenpox, reactivates as shingles and spreads to the eye(s). This variety of keratitis can lead to nerve damage or even glaucoma.
READ MORE about herpes eye infections
Types of keratitis by cause
Other types of keratitis are classified by their cause. Some of these include:
Photokeratitis (UV keratitis or “snow blindness”)
Photokeratitis happens when someone is exposed to natural (sunlight) or manmade sources of ultraviolet (UV) light. In terms of the natural source, it may be reflection of sunlight from snow (snow blindness), water, ice or sand. Photokeratitis can also be triggered by staring at the sun without special eye protection. Artificial sources of UV light include tanning beds and tanning lamps.
READ MORE about photokeratitis
Exposure keratitis
Exposure keratitis, also called exposure keratopathy, involves damage to the cornea from dryness due to the eyelids not closing properly or the increased frequency of blinking. It’s typically a mild, easy-to-treat condition. Exposure keratitis is a form of chronic dry eye, which is also called keratitis sicca.
Left untreated, chronic exposure keratitis can lead to corneal scarring, painful corneal abrasions or a corneal ulcer.
Neurotrophic keratitis
Neurotrophic keratitis, a rare disorder, happens when the nerves that aid corneal function don’t work correctly. Symptoms of this kind of keratitis include eye pain, red eyes, dry eyes, decreased vision clarity and light sensitivity.
Contact lens keratitis
The estimated 45 million Americans who wear contact lenses are susceptible to contact lens keratitis. Contact lens wearers can develop bacterial or fungal keratitis or Acanthamoeba keratitis, all of which fall under the umbrella of microbial keratitis. In fact, wearing contacts is the leading risk factor for microbial keratitis. Contact lenses wearers can also contract noninfectious keratitis by wearing their lenses too long.
Types of keratitis by appearance or location
There are many types of keratitis classified by appearance or location in the cornea. Some include:
Diffuse lamellar keratitis
Diffuse lamellar keratitis, also known as “Sands of Sahara” syndrome, affects 2% to 4% of people who choose to have LASIK surgery to correct their eyesight.
Also called DLK, diffuse lamellar keratitis is a noninfectious complication of refractive surgery characterized by white blood cells and other inflammatory cells accumulating under the corneal flap created during LASIK.
Disciform keratitis
Typically associated with the herpes simplex virus (HSV), disciform keratitis — also called HSV endothelial keratitis — is relatively uncommon. In many cases, it causes swelling in the center of the cornea.
Epithelial keratitis
A frequent complication of cataract surgery, epithelial keratitis appears in the form of dendritic, or treelike, lesions or dot- or point-shaped lesions. Epithelial keratitis also is known as superficial punctate keratitis.
Filamentary keratitis
Filamentary keratitis shows up as strands, or filaments, made up of epithelial tissue cells and mucus that stick to the surface of the cornea.
Filamentary keratitis can be caused by dry eyes or corneal swelling. In some cases, it may be associated with glaucoma but sometimes, the cause is unknown.
Infiltrative keratitis
Infectious infiltrative keratitis is corneal inflammation triggered by microorganisms, while sterile infiltrative keratitis is corneal inflammation lacking the presence of microorganisms. Both, however, produce inflammation of the cornea.
Interstitial keratitis
Interstitial keratitis involves inflammation of the middle layers of the cornea. Affecting one or both eyes, interstitial keratitis often affects children and adolescents who’ve had congenital syphilis. It’s also known as stromal keratitis because it occurs in this deeper layer of the cornea.
Marginal keratitis
Marginal keratitis, sometimes called staphylococcal marginal keratitis, inflames the outer edge of the cornea. It’s a form of keratitis triggered by bacterial staph infections.
Pigmentary keratitis
Pigmentary keratitis primarily affects one or both eyes of a dog. This condition happens when brown pigment (melanin) “invades” the cornea. [Read our article on pigmentary keratitis in dogs.]
Punctate keratitis
Punctate keratitis, also known as superficial punctate keratitis, inflames the upper layers of the cornea. It’s common among people with dry eye syndrome. Punctate keratitis often causes round, oval or star-shaped opacities on the cornea.
Ulcerative keratitis
Ulcerative keratitis, also called peripheral ulcerative keratitis, shows up as crescent-shaped inflammatory damage to the cornea. It’s associated with autoimmune disorders such as rheumatoid arthritis and lupus.
Keratitis treatment
Treatment methods for keratitis depend on the type of keratitis you have.
Common keratitis treatments include:
Applying antibiotic drops
Taking antibiotic or antifungal drugs
Using topical prescription ointment
Applying artificial tears or using other dry eye remedies
Discontinuing use of contact lenses
See an eye doctor
To get relief from red, irritated eyes, see an eye doctor as soon as possible to determine the specific type of keratitis you may have and the best possible treatment.
In most cases, keratitis can be effectively treated relatively quickly with no serious complications.
SEE RELATED: Cogan's Syndrome
Page published on Tuesday, February 23, 2021






