What is blepharitis?

Recognizing the symptoms of blepharitis
Blepharitis is an eye condition characterized by eyelid inflammation. It causes red, swollen eyelids and crusted eyelashes, particularly at the base of the lashes where they attach to the skin. Often a chronic eyelid disease, blepharitis can be challenging to manage and tends to recur.
Eyelid inflammation usually does not cause serious harm to the eyes or a person’s vision. However, it can feel unsightly and uncomfortable.
Common blepharitis signs and symptoms include:
Red eyes
Swollen eyelids
Itchy eyes and eyelids
Crusty eyelids or eyelashes
Sticky or greasy eyelids
Burning or stinging of the eyes
Light sensitivity (photophobia)
Grittiness or a foreign body sensation
Flakes, scales or oily debris around the eyes
Dry skin on the eyelid
Spider veins on the eyelid (telangiectasia)
In some cases, blepharitis causes more severe signs and symptoms, such as:
Loss of eyelashes (madarosis)
Misdirected eyelashes (trichiasis)
Loss of eyelash pigmentation (poliosis)
Blepharitis symptoms are often worse and more pronounced in the morning. Seeking prompt care from an eye doctor can reduce their severity. However, the condition and its symptoms may go through flare-ups and remissions (inactive periods).
SEE RELATED: How to relieve eyelid pain
Primary causes of blepharitis
Blepharitis is among the most common diseases affecting the eyes. Studies have shown that between 37% and 47% of eye care patients had some degree of eyelid inflammation. People of all ages may experience the condition, but it is more frequently diagnosed in those over age 50.
It is common for both eyes to be affected by blepharitis. Causes of this eye disease can include:
Bacterial eyelid infection
Dry eyes
Parasites (eyelash mites or eyelash lice)
Seborrheic dermatitis (dandruff of the scalp and eyebrows)
Allergies
Acne rosacea
Viruses (such as herpes simplex or varicella zoster)
Seborrheic dermatitis is the most common cause of the condition. People with this skin issue often have blepharitis, eyelid dermatitis and other eye concerns.
Types of blepharitis
There are two primary types of blepharitis. They are classified by the portion of the eyelid affected by the disease:
Anterior blepharitis involves the area where the eyelashes extend from the eyelid. People with this form commonly have dandruff in their eyebrows or scalp. Bacteria and a type of yeast on the skin are often contributing factors. It can also be caused by eyelash mites or allergies.
Posterior blepharitis impacts the outer part of the inner lining of the eyelid, where it meets the eye’s surface. Clogged meibomian oil glands in the eyelids often cause this form of the disease. Scalp dandruff and skin concerns (such as rosacea) may also be causative factors.
Microorganisms that cause blepharitis
There are three types of microorganisms known to cause eyelid inflammation. These include:
Bacteria – Bacteria-induced blepharitis is mainly caused by Staphylococci. However, the condition may also result from Corynebacterium and Propionibacterium species.
Mites – Demodex mites are tiny parasites that live in human skin (including the eyelids) and are a major cause of blepharitis. Demodex brevis and Demodex folliculorum, specifically, are known to cause the condition. Demodex mites are associated with rosacea blepharitis and acne rosacea.
Yeast – A skin yeast known as Malassezia spp is also a common cause of eyelid inflammation. These organisms cause seborrheic dermatitis (dandruff) and may play a role in the development of seborrheic blepharitis.
All of these microorganisms are lipophilic, meaning they are attracted to oils in the skin. They make their way into the oil glands in the eyelids (at the base of the lash) and those that make oil for the tear film (meibomian glands). When these microorganisms become overpopulated, blepharitis may develop.
READ MORE: Eyelid: Parts of the eyelid and how they work
How it develops

Blepharitis may arise in a variety of ways. It often occurs from an overgrowth of the normal bacteria that live along the edge of the eyelids and at the base of each eyelash.
Over time, these bacteria multiply and help form a structure called a biofilm. The biofilm coats the edge of the eyelid. It becomes a toxic environment in which disease may develop, much like the plaque that forms on teeth.

Eyelash mites called Demodex are also a common cause of eyelid inflammation. These organisms are present in most people. They live within hair follicles in the skin, including the eyelash follicles in the eyelids. An overgrowth of Demodex mites is often associated with this condition.
Bacteria in the biofilm also produce substances called exotoxins. These cause inflammation of the tiny glands that secrete oil into tears. This can result in meibomian gland dysfunction, which may lead to eyelid inflammation.
Conditions associated with blepharitis
Blepharitis may be associated with skin concerns such as oily skin and dandruff. Eczema, psoriasis and ocular rosacea are other skin disorders linked to eyelid inflammation.
Chronic cases can also lead to the development of the following eye concerns:
Stye – An eyelid stye (hordeolum) is a bacterial infection. It occurs at the base of an eyelash or inside an oil-producing gland in the eyelid. A stye causes a painful red bump at the edge of the eyelid. Individuals with blepharitis have a higher risk of styes.
Periorbital cellulitis – A stye can lead to an infection of the whole eyelid, which becomes red and swollen. This condition can lead to a much more dangerous, deeper infection called orbital cellulitis.
Chalazion – A chalazion is a clogged oil gland in an eyelid that may begin as a stye. It causes a red, swollen bump or nodule on the eyelid. Inflammation of the eyelids increases the chance of chalazia.
Dry eye syndrome – The clogging of the eyelid glands can cause the tear film to evaporate quickly, leading to dry eye syndrome. Among people with dry eye disease, around 25%-40% also have seborrheic blepharitis and meibomian gland dysfunction.
Eyelid scarring – Blepharitis may result in scarring of the eyelid margin. This can occur around the meibomian glands located in the upper and lower lids.
Conjunctival concretion – Long-standing blepharitis can cause small calcium deposits called concretions to build up on the inside of the eyelid. These concretions can occasionally scratch the surface of the eye, causing pain like there is a piece of sand in the eye.
Entropion and ectropion – Inflammation and scarring of the eyelid tissue from chronic blepharitis may affect the position of the lid. Entropion is when the edge of the eyelid turns inward. Ectropion is when the eyelid margin turns outward. Both of these may develop with eyelid inflammation.
Eyelash problems – Scarring and inflammation of the lid margin can lead to misdirected eyelashes. Eyelash loss and the growth of new lashes in the wrong place may also occur.
Cornea problems – Eyelid swelling and inflammation may affect the cornea (the clear outer surface on the front portion of the eye). Blepharitis can cause keratitis or inflammation of the cornea. It may also lead to corneal ulcers (open sores on the surface of the cornea). The misdirection of eyelashes from inflammation can cause trauma to the cornea.
Pink eye – Eyelid inflammation can lead to pink eye (conjunctivitis). When the condition and pink eye occur together, it is called blepharoconjunctivitis.
Effective treatment options for blepharitis
There is no cure for blepharitis. However, it can be treated and managed with proper care.
Blepharitis treatment should begin with a visit to an eye specialist to determine the cause of eyelid inflammation.
An examination of the eyes and eyelids will be performed, often with a slit lamp. This equipment contains a magnifying microscope that eye specialists use to examine parts of the eye. Treatment will then be recommended based on the type of blepharitis present.
Blepharitis treatment may include one or more of the methods discussed below.
Eyelid scrubs: The first line of defense
Keeping the eyelids clean is often the primary defense in treating and preventing blepharitis. A daily regimen of warm compresses and lid scrubs may be recommended to clean the eyelids. This can help reduce the amount of bacteria and debris around the eyes.
Applying a warm compress to the eyes two to four times a day for about five to 10 minutes can loosen eyelid crusting. The warmth can also help open the meibomian glands in the lids and melt the oil inside.
Gentle massaging of the eyelids can increase the flow of fluid from the glands. It is important to use light pressure when massaging the eyelids to avoid causing further irritation or damaging the eye. An eye doctor can recommend the best technique to use.
Gently scrubbing the eyelids helps remove the buildup of debris and bacteria from the lid margins. Cleaning products for eyelid scrubs include:
Prescription eyelid cleansers
Non-prescription eyelid wipes
Diluted baby shampoo
Tea-tree oil and hypochlorous acid scrubs and shampoos may help treat blepharitis by reducing the number of microorganisms on the eyelids. Treatment with these products has proven effective at decreasing the amount of Demodex mites and Staphylococcus bacteria when used for six weeks or longer.
An eye specialist can help determine the ideal products to use for optimal eyelid hygiene.
In-office procedures for severe cases
While at-home eyelid scrubs are helpful, in-office eyelid cleansing procedures may be advised in some cases.
In-office blepharitis treatment can include:
Electromechanical lid margin debridement (such as BlephEx treatment) – This treatment can remove bacteria, biofilm and mites from the eyelids. It is also helpful in opening clogged oil glands. The debridement handpiece is fitted with a medical-grade sponge that removes debris from the eyelashes and edges of the lids.
Thermal pulsation treatment (LipiFlow or iLux, for example) – Thermal treatment helps melt and express particles blocking the eyelid glands. Gentle pulses of heat and pressure are applied to the eyelids through the treatment device. The process also clears flakes and other debris from the gland openings in the eyelid.
Intense pulsed light (IPL) therapy – IPL helps open clogged eyelid glands and improve the flow of oils into the tear film. With IPL treatment, pulses of red light are administered to the skin around the eyes. The warmth from the light helps destroy bacteria. It also reduces mites and allows for easier removal of material blocking the gland openings.
Manual expression – Firm pressure on the eyelids helps unclog the gland openings to improve function. A warming eye mask may be used beforehand to help soften the debris and allow for easier removal. (Manual expression should only be performed by an eye doctor.)
Meibomian gland probing – A thin instrument may be used to gently open and clear blocked oil gland ducts in the eyelid. This process helps relieve blepharitis symptoms by balancing pressure in the oil gland ducts and restoring the natural flow of oils.
Medicated eye drops and ointments: When to use them
Topical medications may be prescribed to destroy bacteria and control blepharitis symptoms. One or more of the following medications may be used to treat and reduce eyelid inflammation:
Antibiotics – Topical antibiotic ointments or eye drops target harmful bacteria on the eyelids and can relieve blepharitis symptoms. Chronic or resistant cases of the condition may require oral antibiotics.
Steroids – Topical steroid solutions can reduce eye inflammation and other blepharitis symptoms. These medications may be combined with topical antibiotics, especially in cases where conjunctivitis or other eye diseases are also present.
Immunomodulators – Topical medications that help suppress the body’s immune system may be prescribed for some patients. These therapies, such as ophthalmic cyclosporine eye drops, help reduce eyelid inflammation and increase tear production.
Ectoparasiticide (anti-parasitic) medication – Lotilaner (brand name XDEMVY) is a treatment for rosacea blepharitis. This type of blepharitis, also called Demodex blepharitis, is caused by Demodex skin mites. XDEMVY eyedrops are taken for six weeks and kill Demodex in the eyelids.
The role of diet: Omega-3 fatty acids
Increasing the intake of essential fatty acids has been recommended in some cases of meibomian gland dysfunction. Treating this condition can aid in controlling eyelid inflammation and its effects.
Many natural products contain omega-3 fatty acids. Sardines, salmon and other types of fatty fish are good sources of this nutrient. Nuts such as walnuts and seeds such as flax and chia seeds are also good sources.
Nutritional supplements like omega-3 fatty acids may help keep the eyelid glands healthy and the eyes moist and comfortable. It is important to consult a doctor before taking any dietary supplements to ensure they are appropriate for specific health needs.
Treating the root cause
In addition to treating eyelid inflammation directly, identifying and addressing the root cause of the condition is also key to managing it.
Special shampoos to reduce dandruff on the scalp and eyebrows may be prescribed in some cases of blepharitis. Eye drops, topical creams, nasal sprays and oral medications may be used to treat conditions that cause or contribute to eyelid inflammation.
Eye specialists often work with other health care professionals to provide comprehensive care for patients.
SEE RELATED: The fastest way to heal a swollen eyelid
Preventing blepharitis: Tips and techniques
Blepharitis is usually a chronic issue, meaning it can come back often. While it might not be possible to prevent all cases, there are ways to minimize the risk and reduce blepharitis symptoms.
The optimal way to prevent eyelid inflammation or keep it from coming back is to clean the eyelids daily. Doing so decreases the buildup of bacteria, biofilm and mites around the eye. It also helps minimize the occurrence of crusty eyelids.
Several non-prescription lid scrub products are available that can be used with the same eyelid-cleaning techniques described below. Prescription-strength eyelid cleansers may also be recommended by an eye doctor.
Eyelid hygiene: Daily practices
Eyelid hygiene is essential to controlling and preventing eyelid inflammation. It often involves the use of warm compresses to loosen and remove debris from the meibomian glands. Eyelid hygiene also includes a cleansing process to remove bacteria and other materials from the lids and lashes.
How to open clogged eyelid glands
To begin, use a clean, warm compress to melt blocked residue (meibum) in the eyelids’ oil glands.
Follow these steps:
Wash your hands, then dampen a clean washcloth with warm water.
Place the compress over your closed eyelids for five to ten minutes.
Gently rub the edges of your eyelids with the washcloth before opening your eyes. Do not press hard on your eyes.
Follow your eye doctor’s recommendations on what type and how often to use a warm compress and how long to keep it in place. It is important to use a clean compress each time.
When you first start blepharitis treatment, you could be instructed to do this several times a day.
How to clean your eyelids
Cleaning your eyelids is an important step toward preventing eyelid inflammation. Your eye doctor can recommend what to use for the cleaning agent. Options may include warm water, diluted baby shampoo or an eyelid cleanser. Cleansers can be over-the-counter or prescription.
To clean the eyelids:
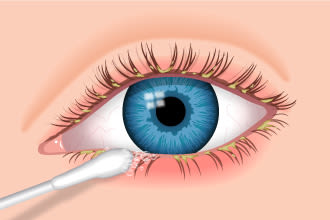
Use a cotton-tipped swab to apply cleaning solution recommended by your eye doctor. Rub gently around the edges of your upper and lower eyelids, but do not get cleaning solution in your eye.
The goal of blepharitis treatment is to return your eyelids to a normal, healthy state.
Wash your hands.
Moisten a clean washcloth, cotton swab or gauze pad with the cleaning solution.
Gently wipe your eyelashes and the edges of your eyelids.
Rinse the area with clean water.
Repeat the process for your other eye, using a different washcloth, swab or pad.
This eyelid cleaning process could be recommended more than once a day to start. In chronic cases, daily eyelid cleansing may be required long-term to manage blepharitis symptoms.
It is a good idea to avoid or limit how often you apply eye makeup when you have this eye concern. Mascara, eyeliner and other eye makeup can interfere with eyelid hygiene.
If your doctor recommends an anti-dandruff shampoo for your scalp and eyebrows, make sure you keep the shampoo out of your eyes to avoid irritation.
Contact lenses and blepharitis: What to know
Blepharitis is also a common cause of contact lens discomfort. It can change the tear film in the eye, making contact lenses difficult to wear.
If blepharitis develops while wearing contacts, it might be recommended to avoid wearing the lenses until the condition has been treated successfully. Eyeglasses may need to be worn until the infection clears up. An eye doctor can provide an exam to update an eyeglass prescription if necessary.
Wearing contacts with eyelid inflammation can result in bacteria and other debris sticking to the lenses. This could cause pink eye or other potentially serious eye diseases.
Those who wear reusable contact lenses might consider switching to daily disposable contacts. Disposable lenses may have a lower risk of blepharitis-related problems. Gas permeable contacts and scleral contacts are other options for those prone to flare-ups.
Many people with eyelid inflammation develop dry eye syndrome, which can make them sensitive to light. In such cases, photochromic lenses may be considered. These lenses have a special coating that automatically darkens in sunlight and lightens indoors.
After the condition has been treated successfully, many people find they can resume wearing contacts.
When to see a doctor
It is important to seek medical care at the first sign or symptom of blepharitis. Eye care professionals can perform an eye exam and determine a diagnosis. They can also provide blepharitis treatment to manage and provide relief from its effects. Since this condition can mimic other eye diseases, it is important to get prompt treatment when symptoms occur.
FAQs
Q: Is blepharitis contagious?
A: No, blepharitis itself is not contagious. However, it may be associated with contagious eye conditions like bacterial and viral conjunctivitis.
Q: How long does blepharitis last?
A: Blepharitis might be chronic (long-lasting) or acute (occurring suddenly but for a short time). Chronic cases may persist for several months to years. Acute cases may cause symptoms that last a week or so.
Q: Can you get blepharitis from eyelash extensions?
A: It is possible for eyelash extensions to inflame the eyelid and cause blepharitis. The eyelash glue is the most common culprit. Doing a test patch for product allergies before having a cosmetic procedure done on the eyelashes is important. Ensuring the lash extension professional practices proper hygiene may help reduce the risk of eyelid inflammation. It is also essential to properly clean and care for eyelashes and eyelids after any procedure.
Q: What is the difference between blepharitis and styes?
A: Blepharitis is inflammation of the eyelids. It causes red, swollen eyelids and crustiness around the eyelashes. Having the condition increases the chance of developing styes. A stye is a pimple-like bump on the eyelid caused by an infected oil gland or eyelash follicle.
READ NEXT: What is blepharospasm (BSP)?
What is blepharitis? American Academy of Ophthalmology. EyeSmart. November 2023.
Blepharitis. National Eye Institute. November 2023.
Blepharitis. American Academy of Ophthalmology. EyeWiki. September 2023.
Blepharitis. American Optometric Association. Accessed October 2023.
Blepharitis. Merck Manual Professional Version. May 2022.
Blepharitis. Cleveland Clinic. December 2022.
Blepharitis. StatPearls [Internet]. January 2023.
Blepharitis, stye and chalazion. University of Illinois College of Medicine. Accessed October 2023.
Blepharitis. Johns Hopkins Medicine. Accessed October 2023.
Dental plaque biofilm: Development, pathogenicity and analysis. International Journal of Science and Healthcare Research. July – September 2021.
Are tiny mites causing your blepharitis? American Academy of Ophthalmology. EyeSmart. March 2022.
Demodex (face mites). Cleveland Clinic. April 2022.
Hyperkeratinization and proinflammatory cytokine expression in meibomian glands induced by staphylococcus aureus. Investigative Ophthalmology and Visual Science. October 2021.
Meibomian gland disease. StatPearls [Internet]. December 2022.
Psoriasis beyond the skin: Ophthalmological changes (Review). Experimental and Therapeutic Medicine. July 2021.
Ocular rosacea. American Academy of Ophthalmology. EyeWiki. June 2023.
Stye. Cleveland Clinic. October 2021.
Stye. Penn Medicine. August 2022.
Chalazion. American Academy of Ophthalmology. EyeWiki. October 2023.
Entropion and ectropion. Merck Manual Consumer Version. May 2022.
Trichiasis. American Academy of Ophthalmology. EyeWiki. September 2023.
Diseases of the eyelashes. StatPearls [Internet]. April 2023.
Keratitis. StatPearls [Internet]. August 2023.
What is a corneal ulcer (keratitis)? American Academy of Ophthalmology. EyeSmart. November 2023.
Blepharoconjunctivitis. StatPearls [Internet]. July 2023.
Eye exam: What to expect. Cleveland Clinic. December 2020.
Meibomian gland dysfunction and treatment. American Association for Pediatric Ophthalmology and Strabismus. March 2023.
Effects of lid debris debridement combined with meibomian gland expression on the ocular surface MMP-9 levels and clinical outcomes in moderate and severe meibomian gland dysfunction. BMC Ophthalmology. April 2021.
How BlephEx works. BlephEx. Accessed October 2023.
Intense pulsed light (IPL) therapy. American Academy of Ophthalmology. EyeWiki. September 2023.
Dry eye disease associated with meibomian gland dysfunction: Focus on tear film characteristics and the therapeutic landscape. Ophthalmology and Therapy. March 2023.
Cyclosporine ophthalmic. AHFS Patient Medication Information [Internet]. October 2018.
A systematic review of the effect of omega-3 supplements on meibomian gland dysfunction. Therapeutic Advances in Ophthalmology. October 2020.
Why do I have eyebrow dandruff? Seborrheic dermatitis explained. GoodRx Health. March 2022.
Disinfect the natural way. Review of Optometry. August 2019.
Clinical efficacy of eyelid hygiene in blepharitis and meibomian gland dysfunction after cataract surgery: A randomized controlled pilot trial. Scientific Reports. July 2020.
What is sleep crust? American Academy of Ophthalmology. EyeSmart. March 2021.
Treating blepharitis: Self-care. UC San Diego Health. August 2021.
Anterior blepharitis: The front line of OSD. Review of Optometry. November 2021.
When blepharitis interferes with contact lens wear. Modern Optometry. April 2023.
Blepharitis treatment. Stanford Medicine. Health Care. Accessed October 2023.
Conjunctivitis (pink eye). National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. CDC. January 2019.
Eye infections from contact lenses. American Academy of Ophthalmology. EyeSmart. May 2023.
Dry eye syndrome. A.D.A.M. Medical Encyclopedia [Internet]. November 2022.
Effect of photochromic contact lens wear on indoor visual performance and patient satisfaction. Ophthalmology and Therapy. July 2022.
Pink eye (conjunctivitis). Cleveland Clinic. August 2022.
Eyelid cosmetic enhancements and their associated ocular adverse effects. Medical Hypothesis Discovery & Innovation in Ophthalmology. July 2019.
Eyelash extensions. American Academy of Ophthalmology. EyeWiki. September 2023.
Review of literature on intraductal meibomian gland probing with insights from the inventor and developer: Fundamental concepts and misconceptions. Clinical Ophthalmology. February 2023.
Page published on Wednesday, January 30, 2019
Page updated on Tuesday, January 23, 2024
Medically reviewed on Saturday, December 16, 2023






