Ocular migraine(s)

Schedule an exam
Find Eye DoctorWhat is an ocular migraine?
Ocular migraine is another name for a retinal migraine. It's a rare condition that can cause temporary blind spots, vision loss and flashes of light in one eye. These symptoms usually last one hour or less.
Some people also use the term ocular migraine to talk about a migraine aura because it causes vision changes, too. In fact, many doctors even mix up these terms, especially if they aren’t headache specialists.
But a migraine aura and a retinal migraine are two different things.
A lot of the words people use to talk about migraines can be pretty confusing. For example, migraine doesn't mean headache. A migraine is a type of neurological condition that can have all sorts of different symptoms. Sometimes they include headaches, but sometimes they don't.
Understanding some migraine basics can help patients have better conversations with their doctors.
| Do you experience migraines? |
|---|
| Ocular migraines are rare and often confused with visual migraines. In either case, if you're suffering from migraines and it's affecting your vision, you need to call an eye doctor. They can help determine what kind of migraine you're dealing with, refer you to a neurologist or other medical professional if needed, and offer treatment options. |
Ocular migraines vs. migraine auras
A retinal (ocular) migraine is a type of migraine, but a migraine aura is a group of symptoms. They're similar in some ways, but they aren't the same.
Retinal migraine (ocular migraine)
A retinal migraine starts in the back of your eye (retina) or right behind your eye.
During an ocular migraine, there is a temporary reduction in blood flow to this area. This is why they have a unique type of visual symptoms.
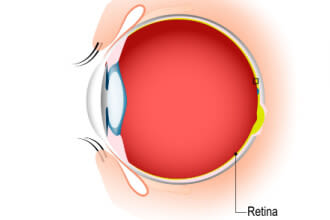
Eye anatomy depicting the location of the retina.
Retinal migraines have been called many different names. In addition to "ocular migraines," some people call them "optical migraines" or "eye migraines."
People can experience pain during or after an ocular migraine, but you can also see vision changes without any pain.
Retinal migraines are rare, but researchers don't know exactly how rare. Some information suggests only one in every 200 migraine patients gets retinal migraines.
Doctors can't diagnose retinal migraines the same way they diagnose other problems. Instead, they diagnose them by ruling out other conditions that cause the same symptoms.
Migraine aura
A migraine aura starts in your brain, not your eye. The aura is one or more symptoms that can happen right before a headache starts. These visual symptoms happen in both eyes.
Some people experience an aura without any pain at all. Doctors call this an “acephalgic migraine” or a “migraine aura without headache.”
It's also common for people to call them "visual migraines." This may be why they get mixed up with ocular migraines so often. Here is an easy way to remember the difference: "visual migraines" happen in your vision, but "ocular migraines" happen in your eye.
About 8% of the population gets migraines with aura.
One in every four people who get migraines sees an aura beforehand. Others will only experience symptoms like headache, nausea and vomiting.
Ocular migraine symptoms
Retinal migraine symptoms only happen in one eye. The visual effects can happen with or without pain.
Symptoms can include:
A blurry or blind spot in your vision that may get bigger as the migraine goes on.
Twinkling lights in your vision.
These visual effects usually last between five minutes and an hour. After that, your vision should go back to normal.
Doctors are usually more concerned about a retinal migraine than a migraine with aura. It's rare, but retinal migraines can sometimes lead to permanent vision loss in one eye. Get medical help if your symptoms last longer than an hour.
Retinal migraines can also have the same symptoms as other serious eye conditions and urgent medical problems. Always tell a doctor when you notice new changes in your vision.
Migraine aura symptoms
Almost all visual migraine auras will make you see at least one unusual effect. Most auras last between five minutes and one hour before they go away on their own.

Visual migraines often appear suddenly and may create the sensation of looking through a cracked window. The visual migraine aura usually moves across your field of view and disappears within 30 minutes.
Visual effects can include:
Flashing lights
Zigzagging lines
Bright spots
Blurry or blind spots
Foggy vision
Wavy or "watery" vision
You can see an aura in both of your eyes. Since they start in your brain, you'll still be able to see things like flashing lights or bright spots with your eyes closed.
But migraine auras aren't always just visual. Around one in three auras comes with sensory symptoms like numbness or tingling in your body. One in every 10 auras includes dysphasic symptoms that make it harder to speak and use language the way you're used to.
Most people get very sensitive to light once their migraine pain starts, even if they don't see an aura beforehand. They can also feel pain or pressure behind their eyes.
SEE RELATED: Other conditions that cause temporary blindness
What causes ocular migraines?
Ocular migraines can be triggered, but researchers don't know exactly why they start happening in the first place. They think that retinal migraines share the same triggers with migraine headaches (with or without an aura).
Possible triggers include:
Stress
Dehydration
Caffeine and caffeine withdrawal
Eye strain
Bright lights
Exercise
Hormonal changes
Contraceptive medication
Food and chemical sensitivity
High blood pressure
Low blood pressure
These are some of the most common triggers, but they aren't the only things that can lead to an ocular migraine.
Ocular migraine treatment
An ocular (retinal) migraine episode is very hard to treat because it lasts such a short time. Drugs that treat migraine headaches usually don't help retinal migraines. That's why doctors usually focus on preventing them instead.
Treating migraine aura alone
It's also hard to stop a migraine aura once it starts, since it usually doesn't last long enough for medicine to kick in.
The FDA hasn't approved any drugs to treat migraine auras without headaches (acephalgic migraines). Possible treatments like magnesium and aspirin have had promising results, but more research is needed.
Treating migraine aura with headache
If you get a headache after an aura, your doctor might suggest treating the pain and other uncomfortable symptoms with:
Over-the-counter pain relievers – Drugs you can buy without a prescription. Some may help treat mild migraines. Common drugs include Advil, Motrin, Excedrin and others.
Triptans – Prescription drugs that block pain inside the brain. Doctors may prescribe Imitrex, Maxalt, Relpax or others.
Ergotamines – A prescription drug that blocks pain inside the brain. Most doctors now prescribe triptans instead of ergotamines. Common drugs include Cafergot, Migranal and others.
Antiemetics – Drugs that treat nausea and vomiting. Common drugs include Reglan, Compazine and others.
Opioids – Prescription narcotic drugs that help relieve pain. Opioid drugs are very addictive, so doctors don't prescribe them unless they need to.
Ocular migraine prevention
Retinal migraines, migraine auras and migraine headaches can be triggered by many of the same things.
Finding and avoiding your triggers may help you have fewer migraines, whether they come with headaches or not. Some triggers can be harder to avoid than others.
Certain medications and supplements may help some people get fewer migraines. Many of these medications were originally used to manage different conditions, such as high blood pressure or depression.
A doctor can help you decide which ones to try. They might recommend:
Antidepressants
Blood pressure medicine
Anti-seizure medicine
Vitamin, mineral or herbal supplements
Devices that temporarily slow down brain activity
Monoclonal antibodies (CGRP)
Always talk to your doctor before you take new drugs or supplements, even if you can buy them without a prescription. Some can aggravate certain conditions or interact with other medications. They can also lead to rebound headaches or even organ damage if you use them too much.
Risk factors
Some things can put you at a higher risk of getting ocular migraines:
Being related to people who get migraines
Being female
Being 30-39 years of age
Retinal migraines are more common in people who have certain health conditions:
Atherosclerosis
Sickle cell disease
Retinal migraines are also more common in female young adults who also suffer from migraines with aura.
Conditions that cause similar symptoms
Certain health conditions can look or feel like an ocular migraine since their symptoms are so similar.
A retinal migraine or visual migraine aura can be confused with:
Retinal tear – A tear or hole in the retina in the back of your eye. It can cause flashing lights, eye floaters, shadows or a "curtain" over part of your vision. Many retinal tears lead to retinal detachments. They can cause permanent vision loss if they aren't treated right away.
Retinal detachment – When the retina separates from the back of the eye. A detached retina can also cause flashing lights, eye floaters, shadows or "curtains'' over part of your field of view. Without immediate treatment, permanent vision loss can occur.
Epilepsy – An overload of electrical activity in the brain that causes someone to move, look or act differently for a short time (a seizure). Some seizures can cause vision problems and nausea, but they usually don't last more than a couple of minutes.
Stroke – A blood clot or burst blood vessel prevents blood from getting to part of the brain. Some strokes can be life-threatening. Migraine is the third most common condition confused with a stroke.
Pseudotumor cerebri (PTC) – High pressure of the fluid inside the skull that can mimic symptoms of a brain tumor, including headaches and vision changes. More than half of people with PTC have temporary episodes of blurry vision.
These aren't the only things that can be confused with ocular migraines. These conditions aren't always serious, but they can be. Visit an eye doctor any time you notice new eyesight changes.
SEE RELATED: 16 of the most common types of headaches
When to see an eye doctor
New vision changes or pain in your head should be diagnosed by an eye doctor or physician.
If you think you're having an ocular migraine, it's important to find out whether it's a true retinal migraine, a migraine aura or something else. When in doubt, talk to a medical professional.
Some migraines can resemble serious health conditions like a stroke. Get medical help right away if you notice any of the signs of stroke.
Clinical features of visual migraine aura: A systematic review. The Journal of Headache and Pain. May 2019.
Migraine with aura. StatPearls [Internet]. December 2022.
Ocular migraine. American Optometric Association. Accessed April 2023.
Retinal migraine headache. StatPearls [Internet]. July 2022.
Retinal migraine: Symptoms, causes and treatment. American Migraine Foundation. May 2022.
Current perspective on retinal migraine. Vision. August 2021.
Migraine headaches. Cleveland Clinic. March 2021.
Migraine aura. Cleveland Clinic. November 2021.
Demystifying migraine with aura. American Migraine Foundation. November 2021.
What ophthalmologists need to know about migraine. EyeNet Magazine. American Academy of Ophthalmology. September 2022.
Retinal migraine. The International Classification of Headache Disorders, 3rd edition. January 2018.
Migraine with aura. The International Classification of Headache Disorders, 3rd edition. January 2018.
Ophthalmologic manifestations of migraines. EyeWiki. American Academy of Ophthalmology. April 2023.
Migraine. Mayo Clinic. July 2021.
Migraine medications. StatPearls [Internet]. May 2022.
Neuromodulation for migraine treatment: An overview. American Migraine Foundation. April 2020.
Migraine prevention 101: What it is, when to use it and why. American Migraine Foundation. August 2021.
What is a torn retina? EyeSmart. American Academy of Ophthalmology. December 2022.
Detached retina. EyeSmart. American Academy of Ophthalmology. October 2022.
Case study: When ocular migraine symptoms indicate impending stroke. Cleveland Clinic. August 2022.
Aura without headache or “silent migraine”: A guide. American Migraine Foundation. September 2021.
Page published on Tuesday, February 26, 2019
Page updated on Tuesday, May 30, 2023
Medically reviewed on Friday, May 12, 2023






