Stye (sty): Treatment, management and diagnosis

Styes: Symptoms and causes
A stye (or a hordeolum) is an infection in the eyelid that causes a tender, red bump near the edge of the eye. The infection is caused by clogged oil glands and bacteria, and it can occur at the base of an eyelash (external stye) or in one of the oil glands within the eyelid (internal stye).
The primary sign of an external hordeolum is a red, inflamed bump that looks like a pimple in or near the eyelashes. Internal hordeola form inside the eyelid, so you can’t see them without everting (flipping) the lid.
Both types can form on either the upper eyelid or the lower eyelid. However, external styes in the lash line are much more common than the type that form internally. Both external and internal hordeola are often painful, and both can sometimes cause the whole eyelid to swell up, especially early on.
What you think is a stye might actually be a chalazion, which is a very similar type of eyelid bump. Chalazia are also caused by clogged oil glands, but they are typically not infected. They can form on their own, or they can form if an internal hordeolum heals without draining properly.
LEARN MORE about stye causes and symptoms
Relieving your symptoms: Do’s and Don'ts
A hordeolum is usually harmless, and most of the time, it won’t require any medical treatment. You can expect it to clear away on its own within just a week or two. Regardless, it can be an uncomfortable nuisance while it lasts. Fortunately, there are some things you can do — and things you shouldn’t do — to help get rid of a stye fast.
DO apply a warm compress or tea bags for your eyes
You can speed up how fast a hordeolum goes away by applying mild heat with a warm compress, such as a tea bag or washcloth. A warm compress can help soften and break up the dirt and oil clogging the gland, as well as draw out infection. For best results, apply the warm compress to the stye for 10 to 15 minutes, three or four times a day.

A basic clean washcloth dipped in warm (not hot) water works well as a compress. Wring the cloth so it is not dripping, then place it over your closed eyes.
If you want to try a tea bag, wait until it cools so it is warm, not hot, and keep it on your eyelid for about 5 to 10 minutes. Use a different tea bag for each eye if you have more than one stye.
You could also try a reusable option, like this Stye Eye Therapy Warming Compress. Some people find that products like these hold warmth a little longer and rest more comfortably on the eye. If you do choose a reusable compress, always make sure to wash it thoroughly between every use.
DO wash your hands and clean your eyelids
Good hygiene goes a long way toward making sure styes heal and stay gone. They are caused by bacteria becoming trapped in a clogged oil gland, so the last thing you want to do is introduce more dirt, oil and bacteria.
Always wash your hands before and after touching the stye. And don't share your towels or washcloths with others.
Keeping your delicate eyelids clean is also key. You can use diluted, tear-free baby shampoo on a cotton ball, washcloth or makeup remover pad. Then rinse your eyelids with warm water and gently pat them dry. You can also use a mild saline solution or a pre-moistened eyelid cleansing pad to clean your eyelids. You can find these non-prescription items in most drugstores.
DO use over-the-counter painkillers for discomfort if needed
Over-the-counter painkillers like acetaminophen and ibuprofen won’t do much to make the hordeolum heal faster. But they can ease any pain or discomfort. Plus, if the eye feels a little better, you’ll be less tempted to touch or rub it.
The less you touch your eye, the less chance there is that you’ll make the stye worse or spread the infection elsewhere.
Always check with your doctor or pharmacist before taking any OTC or prescription painkillers. You’ll need to know if there are any drug interactions with other medications you may be taking. And of course, always take any medication as directed.
DON'T pop or squeeze the stye
Whatever you do, never try to pop a stye. Squeezing or popping it can make the infection worse and even cause the infection to spread deeper into the eye. You also run the risk of damaging and scarring the delicate eyelid tissue.
Using a warm compress will often allow it to open, drain and heal on its own without causing trauma to the eyelid or spreading the infection.
DON'T wear contact lenses or eye makeup
It’s best not to wear contact lenses or eye makeup until your hordeolum has healed. Contact lenses can harbor bacteria that may make it worse or keep it from healing. They can also “bump” or rub the stye and cause more irritation.
Wearing eye makeup can also delay the healing process and potentially introduce more bacteria to the infected area. You should throw out any old makeup or applicators that could be contaminated and cleanse your contact lenses thoroughly before resuming makeup or contact lens wear.
SEE RELATED: How dirty are your facial tools?
DON'T rub your eye or eyelid
Ideally, you should always avoid rubbing or touching your eyes. But it’s especially important when you have any kind of eye infection, including a stye.
The only time you should touch the eye or eyelid is when cleansing the area, and you should always wash your hands both before and after. Rubbing and/or touching the area can cause inflammation to worsen, and it can also introduce more bacteria, dirt and oil.
Diagnosis and preparing for your appointment
If you have any type of eyelid bump, it never hurts to go ahead and schedule a visit with your eye doctor. While styes often clear up without medical treatment, an eye doctor will be able to diagnose and treat any underlying conditions that may be causing them. For example, meibomian gland problems and demodex mites are common issues that can lead to a hordeolum.
You should also see your eye doctor for stye treatment if:
It doesn't start to get better after 48 hours, or it keeps getting larger or worse.
It comes back after going away.
It is affecting your vision.
Your actual eye hurts rather than just your eyelid.
Your eyelid swells up or gets very red.
Your eye won't open all the way.
What to bring to your appointment
Being prepared for an office visit is helpful for both the patient and the doctor. You’ll be better able to answer any questions they have for you, and you’ll be less likely to forget any small details you want to bring up. It’s always a great idea to have certain types of information ready ahead of time, such as:
A list of all medications, vitamins, supplements and herbals you take.
A list of your symptoms and when each symptom began or got worse.
Any personal information that may be relevant to your stye, such as other recent infections, illness or eye injury.
Any photos of yourself that can show the doctor the progression of the stye over time.
Any questions you have for the doctor.
A notepad or your phone so you can be sure to write down any important information.
Treatment
When a hordeolum does require medical attention, the two most common types of treatment are antibiotics and surgical draining. However, both of these treatment types are typically reserved for serious or recurring cases. There is not much evidence that topical or oral antibiotics are effective in directly healing the infection. Instead, they may help to prevent it from spreading.
In some cases, a doctor may recommend eyelash epilation (removing the eyelash from the infected gland). This can allow the infection to drain before resorting to surgical drainage. For a very swollen hordeolum or for a persistent chalazion, a doctor may recommend a steroid injection in the affected area.
Antibiotics for stye treatment
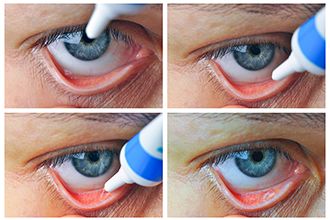
Depiction of how to apply erythromycin ointment to the eye
The most common type of topical antibiotic used in the treatment of styes is erythromycin ointment. Bacitracin ophthalmic ointment is also sometimes used. Erythromycin works by disrupting the bacteria’s protein synthesis process, which it needs to grow and survive. Bacitracin works by disrupting the bacteria’s ability to build and maintain its cell walls.
Oral antibiotics may be more effective for cases that are resistant to home treatments. Doctors will also prescribe oral antibiotics if the infection spreads or if there is a risk of developing periorbital cellulitis. Some of the more common oral antibiotics used for styes include:
Erythromycin – Like its topical version, oral erythromycin inhibits bacterial growth by disrupting its protein synthesis process. It is often used to treat respiratory and skin infections, as well as UTIs and certain STDs.
Tetracycline – This type of antibiotic also works by inhibiting a bacteria’s protein synthesis so that it can’t grow. It is often used to treat skin infections and acne, among other types of infection. A commonly known type of tetracycline is doxycycline.
Amoxicillin – This penicillin-like drug works by disrupting the bacteria’s ability to build and maintain its cell walls (similar to bacitracin). It is an effective treatment against many bacterial infections, including strep throat, pneumonia and UTIs.
Cephalosporin – This type of antibiotic also works like penicillin to attack the bacteria’s cell walls. It is often used to treat infections caused by staph and strep bacteria, including cellulitis and abscesses, as well as ear infections. A commonly known type of cephalosporin is cephalexin.
Stye surgery
In some cases, styes may require minor surgery. If your doctor recommends surgery, they will refer you to an ophthalmologist or oculoplastic surgeon to perform the procedure. Draining a stye is a fairly simple outpatient procedure done in the doctor’s office in about 15 minutes.

Surgical draining or steroid injection to the affected area may help to eliminate a stye.
First, the specialist will inject a local anesthetic into the affected area to numb the eyelid. Once the numbing agent is working, they will use a very fine needle to create a hole that allows the stye to drain. For a large, abscessed stye or a chalazion, they may need to use a surgical implement to create a slightly larger incision for drainage or cyst removal.
This procedure usually does not require stitches, but you may need to wear a pressure patch on your eye for a few days while it heals. You’ll also need to use an antibiotic ointment or cream during the healing process to keep the area from becoming reinfected.
Questions to ask your eye doctor
During your diagnosis appointment, be sure to ask the eye doctor any questions you may have. While the internet can be a great way to find basic information, doctors are always the best resource. They can provide answers, treatment and guidance that may be specific to your case. Don’t assume that your questions aren’t important — or that you already know the answer.
Things you may want to ask your eye doctor include:
What caused my stye?
Is it contagious?
Do I have to change my pillowcase?
How should I wash my eyelids?
How long will it take for the stye to go away?
Should I stop wearing contact lenses until it has healed?
How does my prescribed treatment work? Does it have side effects?
Are there other treatment options?
What will happen if I don’t use/have this treatment as prescribed?
Always feel free to ask for clarification about anything you’re not sure you understand. Your doctor will appreciate it — informed patients have better outcomes!
Stye. American Academy of Ophthalmology. EyeWiki. October 2022.
Chalazion and hordeolum (stye). Merck Manual Professional Version. May 2022.
Chalazion and stye. Kellogg Eye Center. University of Michigan Health. Accessed October 2022.
Chalazion. Icahn School of Medicine at Mount Sinai. December 2020.
Hordeolum (stye). American Optometric Association. Accessed October 2022.
What are chalazia and styes? American Academy of Ophthalmology. EyeSmart. September 2022.
Stye. Cleveland Clinic. October 2021.
Stye. StatPearls [Internet]. August 2022.
Styes. Nemours KidsHealth. Accessed October 2022.
How to treat boils and styes. American Academy of Dermatology Association. Accessed October 2022.
Stye. Patient.info. July 2022.
Why you shouldn’t pop a stye. K Health. February 2022.
Can you wear contacts with a stye or chalazion? ContactsDirect. November 2021.
Eyelid bump. MedlinePlus, National Library of Medicine. August 2020.
Everything you need to know about antibiotics for styes. K Health. February 2022.
Chalazion and stye treatment. Stanford Medicine. Accessed November 2022.
Stye treatments and medications. SingleCare. October 2020.
Do stye antibiotics come in ointment or tablet form? American Academy of Ophthalmology. EyeSmart. February 2022.
Styes in children. Stanford Medicine. Accessed November 2022.
Erythromycin coupons & prices. SingleCare. Accessed November 2022.
Erythromycin. GoodRx. Accessed November 2022.
Bacitracin topical.StatPearls [Internet]. November 2021.
Erythromycin. AHFS Patient Medication Information [Internet]. Bethesda (MD): American Society of Health-System Pharmacists, Inc. September 2019.
Tetracycline. Britannica.com. October 2022.
Doxycycline: Uses, side effects, dosage. K Health. December 2021.
What is amoxicillin: Dosage, side effects, and more. K Health. December 2021.
Augmentin coupons & prices. SingleCare. Accessed November 2022.
Cephalosporins. StatPearls [Internet]. September 2022.
Cephalexin coupons & prices. SingleCare. Accessed November 2022.
Efficacy of care and antibiotic use for chalazia and hordeola. Eye & Contact Lens: Science and Clinical Practice. April 2022.
Antibiotics ineffective in chalazion, hordeolum treatment. Review of Optometry. November 2021.
How to get rid of a stye. K Health. February 2022.
Surgery for stye. NYU Langone Health. Accessed November 2022.
Patient engagement. Centers for Disease Control and Prevention. August 2021.
Page published on Tuesday, February 9, 2021
Page updated on Tuesday, December 6, 2022
Medically reviewed on Saturday, October 15, 2022







