Retinal Detachment FAQ

What is retinal detachment?
Retinal detachment is a serious eye condition that occurs when the retina separates from its normal location in the eye. The retina (a light-sensing structure in the back of the eye) transmits chemical and electrical signals to the brain, allowing it to process what you see.
A detached retina cannot function properly.
Part or all of the retina may become detached. Any amount of detachment affects vision in some way and could even lead to blindness.
Having a detached retina, or being at risk of one, is a frightening situation, leading many people to ask questions like:
How do you get a detached retina?
What does a detached retina feel like?
What happens when your retina detaches?
Can a detached retina be fixed?
Can a detached retina heal itself?
What are the warning signs of a detached retina?
Read on to learn more about retinal detachments and explore some of the most frequently asked questions about this sight-threatening condition.
SEE RELATED: Retinal detachment: Causes, symptoms and treatments
How does a retina detach?
“How does your retina detach?” is a question undoubtedly asked by those facing this serious vision concern. The retina detaches from the back of the eye wall when this thin layer of tissue is pushed or pulled away from its normal position. This also allows fluid to leak into the space beneath the retina. The force created by the fluid pushes the retina away from its normal location, causing it to separate from the eye wall.
Certain factors may cause the retina to detach, including:
The vitreous (a gel-like substance in the center of the eye) shrinks with age, pulling away from the back of the eye. While this is often a normal part of aging (called posterior vitreous detachment), it can tug on the retina and cause it to tear.
The growth of new, abnormal blood vessels in or around the retina creates scar tissue that pulls the retina away from the back of the eye.
Fluid accumulation beneath the retina (caused by certain eye or health conditions) causes the layers of the retina to pull apart.
Blunt force trauma to or around the eye can shake the vitreous, causing it to tug on and tear the retina.
Seeking prompt medical care for a detached retina is crucial and often necessary to prevent further detachment and vision loss.
What is the most common cause of retinal detachment?
Age and eye trauma or injury are the most common causes of retinal detachment. There are three types of retinal detachment, each with unique characteristics and causes:
Tractional retinal detachment
This occurs when scar tissue on the retina pulls it away from the back of the eye. It is common in people with diabetes because of the damage the disease can cause to blood vessels in the retina.
Rhegmatogenous retinal detachment (RRD)
A rhegmatogenous (reg-mah-TAH-jeh-nus) retinal detachment is the most common type of detached retina. It is caused by a hole or tear in the retina. The vitreous can leak through the hole and collect behind the retina, pushing it farther away from the back of the eye until it detaches. Age-related retinal tears are the most common cause of RRD. Injury and eye surgery are also possible causes.
Exudative retinal detachment
Similar to RRD, exudative retinal detachment involves fluid buildup behind the retina. However, no holes or tears are present in this form. Instead, the buildup results from leaking blood vessels and swelling in the eye. As the fluid gathers, it pushes the retina away from the back of the eye, causing it to detach. This type of retinal detachment is often related to:
Inflammation
Infections
Tumors
Eye conditions such as age-related macular degeneration
How might one develop a detached retina?
Some people may be at a higher risk of experiencing a detached retina. Age is one of the most common risk factors for this condition. Retinal tears or holes are another. But you could also be at risk due to factors such as:
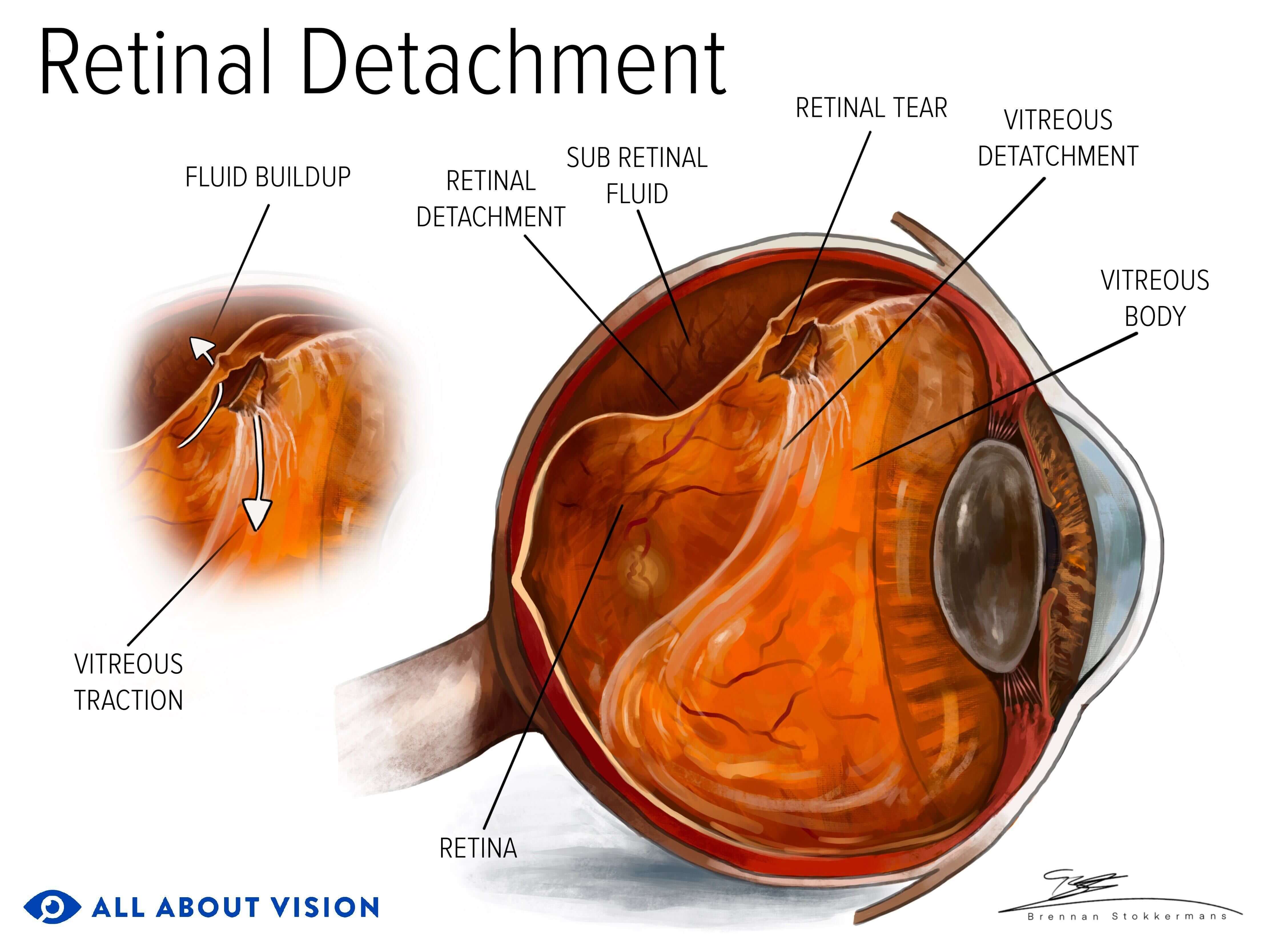
Click image to enlarge.
Posterior vitreous detachment (PVD)
Extreme nearsightedness (high myopia)
Eye injury or trauma
Family history of retinal detachment
Personal history of retinal detachment
Eye conditions (such as lattice degeneration and glaucoma)
Understanding retinal detachment symptoms and risk factors plays a key role in catching this condition as early as possible. If you may be at risk for this condition, visit your eye doctor for a dilated eye exam as soon as possible.
Does retinal detachment happen suddenly?
Retinal detachment can happen suddenly or gradually, depending on the cause.
If trauma or injury to the eye is responsible for the detachment, it typically occurs suddenly. This may be due to the vitreous applying significant traction on the retina, causing it to tear and detach from the back of the eye.
Usually, with age-related retinal detachments, the vitreous will tug on or rub against the retina for a period of time before the retina eventually detaches. In these cases, the vitreous will pull against the retina and cause floaters and flashes without causing a torn or detached retina right away.
What are the early warning signs of a detached retina?
Early warning signs of a detached retina may come in the form of visual symptoms, such as the sudden onset of flashes or new floaters. Retinal tears, retinal holes, PVD, scar tissue formation and excess fluid around the retina can all lead to retinal detachment. The presence of these conditions (among others) could mean retinal detachment is more likely to occur.
An eye doctor may detect signs of a detached retina during a routine eye exam. In other instances, a patient may visit an eye doctor when experiencing retinal detachment symptoms. A doctor may conduct a dilated eye exam and use other techniques to visualize the retina and confirm detachment.
Getting routine dilated eye exams is important, as some retinal detachments may not cause any symptoms.
How long before retinal detachment causes blindness?
There is no definitive answer for how long it might take retinal detachment to lead to blindness. The loss of vision can be sudden or occur over the course of days or weeks, depending on the circumstances surrounding the detachment. The longer the reattachment is delayed, the greater the chance of vision loss.
A detached retina is a medical emergency and requires prompt care. To help preserve your vision and prevent blindness, it is best to get regular eye exams and seek medical care immediately if symptoms occur.
Is retinal detachment painful?
No, retinal detachment is not painful. In fact, most people do not feel anything at all. So when symptoms of retinal detachment appear, they may not realize what is happening.
That is why recognizing symptoms of retinal detachment is so important. They can alert you that something is wrong with your eye so you can seek medical attention before severe damage results.
How does a detached retina feel?
As mentioned, a detached retina is not a painful condition. In some instances, there may be no initial symptoms. But “what does retinal detachment feel like” is something people often wonder. Symptoms of retinal detachment are not necessarily physical but, rather, are visual. Most people have blurry vision, floaters, flashes of light or a dark gray veil or curtain in their vision. Symptoms may get worse as the retina becomes further detached.
What are the symptoms of a detached retina?
Symptoms of a detached retina include varying degrees of the following:
Flashes of light in your vision
The sudden appearance of or a considerable increase in eye floaters
Shadows that develop in your peripheral vision (sometimes described as a “dark curtain”)
Blurry vision
Since you won't feel it when a retina detaches, it's important to know the visual symptoms. They will alert you to the problem so you can seek treatment as soon as possible.
Are flashes in the eye dangerous?
Seeing flashes of light is a common symptom of retinal detachment. However, their presence is not necessarily dangerous.
When vitreous gel within the eye tugs, bumps or rubs against the retina, this mechanical traction on retinal cells triggers a flash of light. More often than not, this phenomenon is harmless, and there is no need for alarm.
If you suddenly notice frequent flashes of light, see an eye doctor. Your doctor can determine if the flashes mean you are at risk for or already have a detached retina.
How can you confirm if your retina is detached?
The onset of concerning symptoms often prompts people to visit their eye doctor. In rarer cases, a detached retina is detected during a routine eye exam. How do you know if your retina is detached? The only way to confirm a retinal detachment is to see your eye doctor for an exam.
Your doctor will place drops in your eyes to dilate (widen) your pupils, which allows them to see more of your retina. They will check to see if any part of the retina has become detached and for the presence of fluid around the retina. Imaging techniques and retinal scanning are also used to diagnose retinal detachment.
READ MORE: Retinal imaging and scans
Is it possible to fix a detached retina?
In most cases, a detached retina can be treated and repaired. The type and severity of the detachment help dictate the form of treatment provided. Smaller detachments are often repaired with cryotherapy (freezing) or laser surgery. More advanced detachments may require a surgical approach.
Can a detached retina heal on its own?
Most cases of retinal detachment do not heal without treatment. Although very rare, it may occasionally heal and reattach on its own. However, this condition usually requires professional care to prevent further damage and vision loss.
Treatment reattaches the retina to the back of the eye and restores its blood supply, which the eye will not do on its own.
Minor retinal tears can sometimes form scar tissue at the border of the torn retina. This scar tissue may keep a small tear from worsening. In such cases, surgery may not be required.
Is retinal detachment an emergency?
Yes, a detached retina is a medical emergency that requires immediate attention. While there is no need to panic, symptoms of retinal detachment are definitely not something to ignore.
If you begin having symptoms of retinal detachment, contact an eye doctor immediately and tell them about your symptoms.
If your symptoms are caused by a detached retina, failure to seek immediate care from an eye doctor and have timely retinal detachment surgery could result in permanent vision loss and even blindness.
READ MORE: When to see a retina specialist
How long can one wait before treating a detached retina?
Treating a detached retina as soon as possible can prevent unnecessary vision loss.
Research was conducted to evaluate the outcomes of macular retinal detachment surgeries performed at Stanford University Hospital. It found that earlier surgery led to better visual outcomes.
Patients in the study were divided into two groups:
Group 1 had surgery within three days of detachment.
Group 2 had surgery within four to seven days of detachment.
Group 1 experienced significantly better final visual acuity after surgery:
Group 1 (approximately 20/30)
Group 2 (approximately 20/70)
A study involving data from the Japan-Retinal Detachment Registry also showed significant findings. Surgeries were conducted at intervals ranging from two days to six days after detachment began. The patients were evaluated six months after surgery.
The results showed that earlier surgery provided progressively better results:
Within two days of onset – Better visual acuity than having surgery after three days
Within three days of onset – Better visual acuity than having surgery after four days
Within four days of onset – Better visual acuity than having surgery after five days
Within five days of onset – Better visual acuity than having surgery after six days
The question of “How long can retinal detachment go untreated?” may not have a definitive answer. However, these data emphasize the importance of seeking treatment for retinal detachment as soon as possible.
What happens if a retina detaches and isn't treated immediately?
Retinal tears or holes identified before the retina detaches may be repaired with laser or cryopexy (cold) therapy. However, more extensive detachments generally require surgery. In the majority of cases, retinal detachments are emergencies and need immediate care.
The time frame during which treatment should take place varies according to how severe the detachment is and the specific part of the retina that has detached. If the detachment does not involve the macula (the part of the retina responsible for central vision), surgery should take place immediately (within one day).
To optimize the chances of preserving vision, it is crucial to undergo treatment for a detached retina shortly following its detachment. The earlier retinal detachment is diagnosed and treated, the better the chance of treatment success and vision preservation. The longer the time that passes before treatment takes place, the greater the risk of permanent vision loss and blindness.
How do you repair a detached retina?
How do you fix a detached retina? Detached retinas are often repaired with retinal detachment surgery. Different types of retinal detachment surgery include:
Vitrectomy
In a vitrectomy, an eye surgeon removes the gel-like vitreous from the back of the eye to relieve tugging on the retina. An air, oil or gas bubble is then injected to press the detached portion of the retina against the back of the eye so healing can occur. Eventually, the air or gas is absorbed by the body, and the vitreous space refills with fluid produced by the body. (An oil bubble will usually be removed from the eye a few months after surgery.) In some cases, a vitrectomy may be performed in conjunction with a scleral buckling procedure (listed below).
Pneumatic retinopexy
In this procedure, a retina surgeon injects a gas bubble into the vitreous body in the back of the eye. Your head is positioned so that the bubble floats to the area of the retinal detachment. The bubble presses the detached portion to the back of the eyeball to reconnect it to its blood supply while healing occurs. The surgeon then seals any tear in the retina using a laser or freezing probe.
Scleral buckle
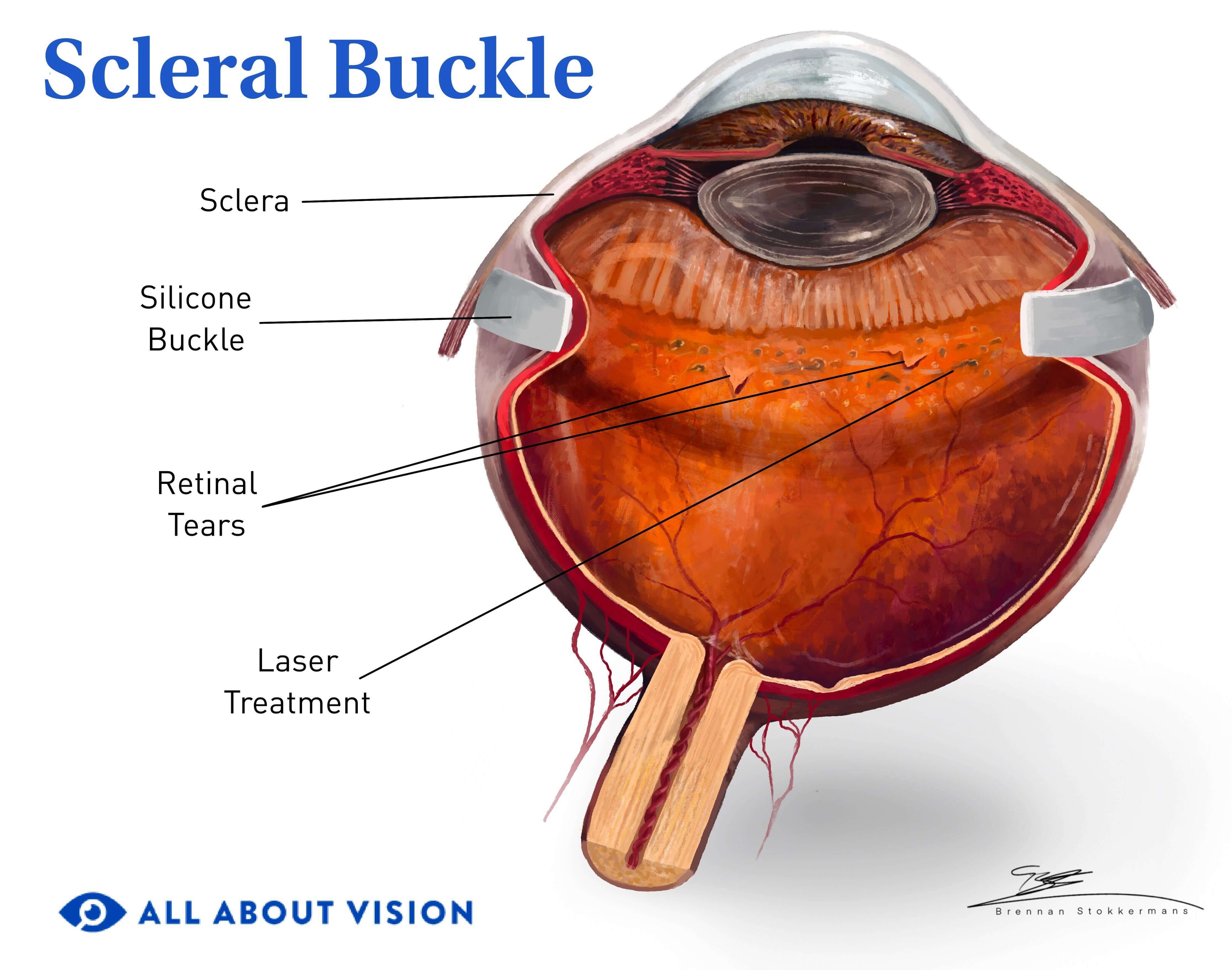
Click image to enlarge.
Rather than addressing a detached retina from the inside of the eye like the other two procedures, a scleral buckle approaches retinal reattachment from the outside. A pliable band made of soft plastic or rubber is fastened to the outer wall of the eyeball, exerting gentle inward pressure on the eye. Using this method, the retina is able to reattach and heal against the eye wall.
Because a detached retina is such a serious condition, it is important to have regular eye exams to make sure your retinas look healthy. An eye doctor can determine if you are at risk for retinal detachment or other vision problems.
How to manage an air bubble in the eye post-treatment
A gas, air or oil bubble may be placed in the eye during some retinal detachment treatments. This bubble functions to hold your retina in place as it heals. You may need to keep your head in a certain position for a period of time following the procedure to keep the bubble in the proper place. This may be anywhere from several days up to two weeks.
Though you might wonder how to get rid of the air bubble in your eye or how long it might be there, it is important to follow your doctor’s aftercare instructions, as it is an important part of the treatment process.
A gas or air bubble will eventually dissolve, and the body will produce fluid that takes the place of the bubble. An oil bubble will usually be removed from the eye during a follow-up procedure within six months after the retinal detachment procedure.
READ MORE: Detached retina surgery recovery
Detached retina. EyeSmart. American Academy of Ophthalmology. November 2023.
Anatomy, head and neck: Eye retina. StatPearls [Internet]. August 2023.
Detached retina (retinal detachment). Kellogg Eye Center. University of Michigan Health. Accessed February 2024.
Retinal detachment. Johns Hopkins Medicine. Accessed February 2024.
Retinal detachment. National Eye Institute. November 2023.
Retinal traction detachment. StatPearls [Internet]. August 2023.
Pathophysiology of secondary macular hole in rhegmatogenous retinal detachment. Investigative Ophthalmology & Visual Science. October 2023.
Types and causes of retinal detachment. National Eye Institute. December 2020.
Exudative retinal detachment. EyeWiki. American Academy of Ophthalmology. June 2022.
Detached retina. Harvard Health Publishing. Harvard Medical School. April 2019.
Posterior vitreous detachment. StatPearls [Internet]. August 2023.
Retinal detachment. StatPearls [Internet]. December 2022.
Experimental evidence to understand mechanical causes of retinal detachment following blunt trauma. Experimental Eye Research. August 2023.
Demographics and seasonality of retinal detachment, retinal breaks, and posterior vitreous detachment from the Intelligent Research in Sight Registry. Ophthalmology Science. American Academy of Ophthalmology. June 2022.
What are floaters and flashes? EyeSmart. American Academy of Ophthalmology. December 2023.
Exudative retinal detachment. StatPearls [Internet]. February 2023.
Retinal tears can cause vision loss. Here are why they happen and symptoms you don’t want to miss. GoodRx Health. December 2023.
Bilateral retinal detachments in a healthy 22-year-old woman after Moderna SARS-COV-2 vaccination. The Journal of Emergency Medicine. July 2021.
Retinal detachment caused by injury to the eye. Merck Manual Consumer Version. May 2022.
Retinal detachment. Merck Manual Professional Version. April 2022.
Retinal detachment repair. A.D.A.M. Medical Encyclopedia [Internet]. August 2022.
Case of spontaneous reattachment of rhegmatogenous retinal detachment. Oxford Medical Case Reports. September 2021.
Retinal detachment: Diagnosis and treatment. EyeSmart. American Academy of Ophthalmology. September 2020.
Silicone oil removal: Timing and retinal detachment recurrence. Investigative Ophthalmology & Visual Science. July 2019.
Page published on Tuesday, October 20, 2020
Page updated on Tuesday, August 20, 2024
Medically reviewed on Sunday, April 7, 2024






