Optic neuritis and neuropathy: Symptoms, causes, treatments
Schedule an exam
Find Eye DoctorThe optic nerve is the connection between the eye and the brain that transmits visual information from the retina. Inflammation of this nerve is called optic neuritis. During optic neuritis inflammation can cause damage to the protective sheath (myelin) surrounding this nerve and the nerve itself. It can effect one optic nerve or both optic nerves at the same time.
Vision symptoms from optic neuritis can include blurring, blind spots or complete loss of vision. You also may notice distorted vision, reduced color vision and pain when you move one or both eyes. These types of symptoms may precede vision loss due to optic neuritis.
The term optic neuropathy more generally describes optic nerve abnormalities or damage. This damage could be from blocked blood flow, certain medical conditions or toxic exposure. Optic neuritis is one specific cause of an optic neuropathy.
What causes optic neuritis?
Optic neuritis can occur in anyone, but usually occurs in adults younger than 45 and affects more women than men. The condition is common in people who have multiple sclerosis (MS), which occurs when the body's own immune system attacks and destroys protective nerve coverings.
Besides affecting eyesight, related nerve damage in MS can lead to loss of mobility and sensory functions, along with other debilitating conditions.
Other causes of optic neuritis include:
Neuromyelitis Optica Spectrum Disorder
Anti-MOG Ab associated Syndrome
Acute Disseminated Encephalomyelitis
Other causes of optic neuropathy include:

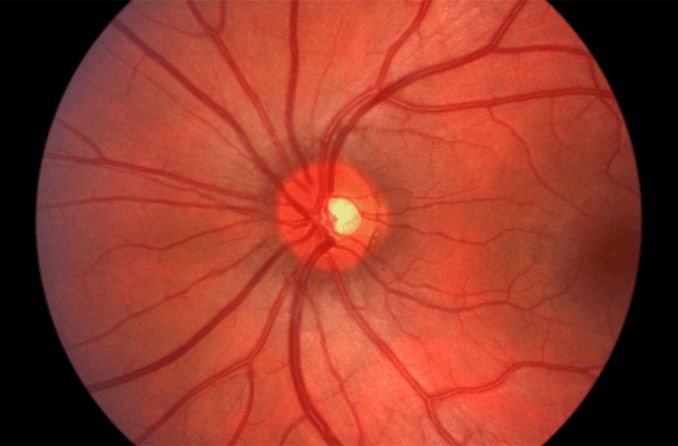
Image of the back of a healthy eye, where the optic nerve is located. When the optic nerve is damaged, poor vision results.
Infections such as toxoplasmosis, cryptococcus, herpes simplex
Other viral infections
Neurological disorders
Leber hereditary optic neuropathy, an inherited form of vision loss that affects mostly males in their 20s or 30s
Certain medications (eg ethambutol, vigabatrin)
Nutritional deficiency
Toxins, including methanol, alcohol and tobacco
When optic neuritis is present, the pupil can react in an abnormal fashion (afferent pupillary defect). This means the pupil actually dilates instead of constricting in the presence of bright light. Depending on the severity of optic neuritis, the optic nerve may appear normal or swollen.
During an eye exam, your eye doctor will look for signs of optic neuritis by conducting tests to evaluate whether you have reduced vision, visual field tests to determine if you have an enlarged blind spot (also known as a scotoma) and optical coherence tomography to determine if there has been damage to the optic nerve fibers.
Your eye pressure may be measured, and your pupils may be dilated to provide a better view of the eye's interior structures, including the optic nerve and retina.
You may also be referred for an MRI of the optic nerves and the brain to detect possible underlying causes of optic nerve inflammation.
A person with optic neuritis usually undergoes an MRI of the brain, to look for central nervous system lesions.
Treatments for optic neuritis
Treatment of optic neuritis has changed in recent years, due to a number of studies. These include Optic Neuritis Treatment Trials (ONTT).
In the ONTT, participants with optic neuritis were randomized for treatment with intravenous (IV) steroids, oral steroids or placebo. Afterward they were evaluated for several years.
From these studies, researchers learned that treatment with steroids had little effect on the final visual outcome as measured by high contrast visual acuity (black letters on a white background), but there was a benefit to vision when measured with more sensitive tests.
However, patients treated with high doses of steroids had fewer repeat attacks of optic neuritis than patients treated with low dose steroids alone. In fact, those treated with oral steroids alone had a higher risk of repeat attacks of optic neuritis than those treated with placebo.
Even more importantly, patients treated initially with IV steroids had about half the risk of developing MS in two years as patients treated with oral steroids only, or placebo. Of those treated with IV (followed by oral) steroids, 7.5 percent developed MS in the following two years, versus about 16 percent in the other groups.
As a result of the ONTT, eye doctors now usually treat patients with a combination of IV and oral steroids or monitor the condition without prescribing medical treatment. Use of low dose steroids alone is not recommended.
For patients who are medically treated, the regimen typically includes three days of high dose steroids, followed by about 11 days of an oral steroid taper.*
Additionally, patients with optic neuritis may be offered treatment with a procedure called plasmaexchange (PLEX). This therapy requires a patient to be connected to a machine for 1-2 hours. During this time, the patient’s blood is taken via an IV to the machine and certain plasma proteins are removed. The patient’s blood is then returned to them having been “cleaned” of some of the immune system components that promote inflammation.
Prognosis for those who have optic neuritis
Visual deficits caused by optic neuritis may worsen over a period of about seven days before vision typically stabilizes at that level for three to eight weeks. Gradual vision improvement then may occur.
About 95 percent of people with optic neuritis will recover much of their vision within six months of onset. However, about 19 percent will have a recurrence of optic neuritis in the affected eye, and 17 percent will develop optic neuritis in the other eye within 10 years.** This is why careful testing to determine the cause is important. Recurrent events are preventable if an underlying disorder can be identified.
As mentioned above, sometimes optic neuritis is a precursor to development of MS, so if you have optic neuritis, your doctor may recommend an MRI. If imaging shows "white matter" lesions indicating damage to myelin in brain-based nerve fibers, there is a 80-90% chance of meeting criteria for MS within 5 years. But even with normal results, a person with optic neuritis has a 22% chance of developing MS.**
Thus, working with an ophthalmologist and neurologist is warranted.
READ NEXT: What is the Optic Disc
*Optic neuritis. Ferri's Clinical Advisor 2009, 1st ed.
**Optic neuritis. Conn's Current Therapy 2008, 60th ed.
Page published on Monday, March 4, 2019






