Eye redness (bloodshot eyes)
Why are my eyes red?
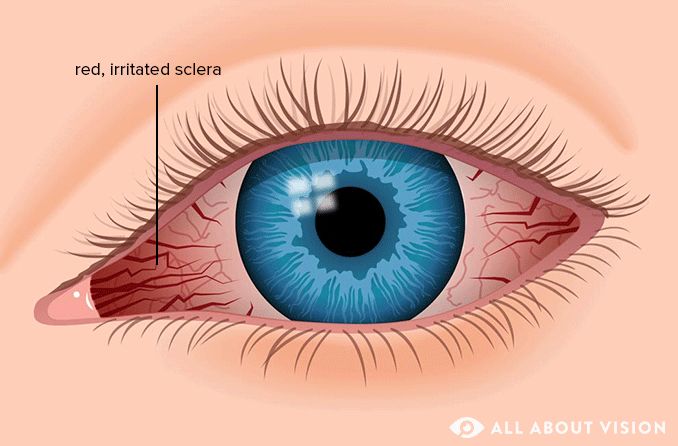
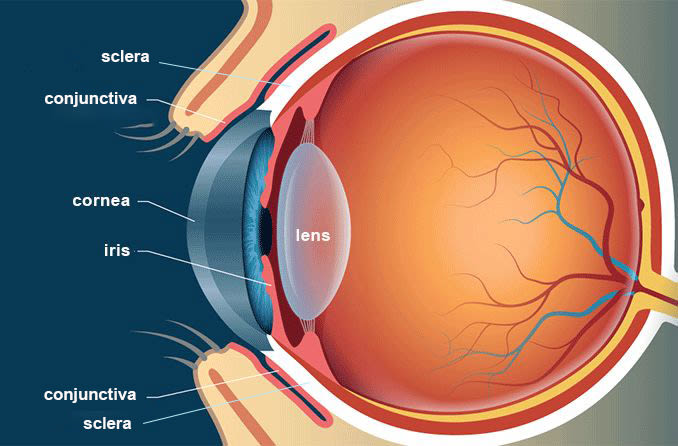
Eye redness usually refers to when the white part of the eye (the sclera) appears reddened or "bloodshot." It may occur when blood vessels located on the eye’s surface swell or become enlarged. Red eyes may result from an injury, an infection, inflammation or an eye condition.
Click on image to enlarge.
Along with the sclera, other areas of the eye may take on a red or bloodshot appearance. These include the conjunctiva (the thin layer covering the sclera and the inner eyelids), the episclera (the membrane between the conjunctiva and sclera) and the iris (the colored portion of the eye).
The overall appearance of red eyes can vary. It can look like there are squiggly pink or red lines on the sclera, or the entire sclera may appear pink or red. In other instances, there may be a red spot or splotch or a larger area of redness on the eye.
Eye redness may develop gradually or occur without warning. It is often temporary and typically goes away once the underlying cause resolves.
Signs and symptoms associated with bloodshot eyes
Eye redness can develop in one or both eyes. It can be associated with several other signs or symptoms related to the eye, including:
Bloodshot eyes may also occur with no other signs or symptoms, but this tends to be less common.
Red eyes occur when the blood vessels on the surface of the eye expand.
Many people think of eye redness as a symptom, but it is actually a sign of a condition or other concern. An easy way to remember is that a sign is what a doctor sees, and a symptom is what the patient tells the doctor.
Red eyes are often a sign of eye conditions that can range from benign to serious. However, some serious conditions may only cause mild eye redness. The appearance of other signs or symptoms (such as vision disturbances or eye pain) with redness may point to a more serious issue.
Causes of red eyes
Red or bloodshot eyes can result from a variety of factors. While many red eye causes are less concerning or minor, others can indicate a medical emergency and require prompt care.
The appearance of red eyes is caused by the dilation of blood vessels on the eye’s surface. These blood vessels (many of which normally are invisible) can become swollen, allowing more blood to enter the eye. This causes the eye to look red, pink or bloodshot.
Red eyes are most often caused by inflammation of the conjunctiva. Pink eye (conjunctivitis) and allergens are the most common culprits.
Red eyes are also frequently the result of dry eyes and the extended wear of contact lenses.

In some cases, a blood vessel may break, causing a bright red spot to develop on the white of the eye. This is called a subconjunctival hemorrhage and may result from an eye injury, straining, coughing or other factors. A subconjunctival hemorrhage is more likely to occur when taking a blood thinner (such as Coumadin) or an NSAID (such as ibuprofen).
Eye redness causes may include a variety of environmental or lifestyle-related reasons. However, bloodshot eyes may also signal specific eye problems.
Read on to learn more about the causes of eye redness.
Common eye conditions
A number of minor eye problems can cause the white of the eye to appear red, pink or bloodshot. These include:
Pink eye
Subconjunctival hemorrhage
Serious eye conditions
Red or bloodshot eyes may result from more concerning issues involving the eye, such as:
Herpes simplex keratitis (ocular herpes)
Herpes zoster ophthalmicus (eye shingles)
Allergies
Red eyes are often a sign of eye allergies. Allergens, or factors that trigger an allergic reaction to something, can be found in both indoor and outdoor environments.
When airborne allergens (such as pollen, dust, mold and pet dander) come into contact with certain types of cells in your eyes, a substance called histamine is released. Histamine causes the blood vessels beneath the eye’s surface to expand and become inflamed, often causing the eyes to become red and swollen.
Contact lens irritation
Wearing contact lenses for an extended period of time can affect the cornea, leading to eye redness and irritation. Sleeping with contact lenses in and not keeping up with proper contact lens hygiene can lead to an eye infection and cause a variety of issues, including bloodshot eyes.
Contact lens irritation may also result if the lens is poorly fitting or old, if there is debris trapped beneath it or if it is not used correctly.
Eye injury
Injury or trauma to the eye can range from minor to severe and may cause eye redness. Eye injuries may involve getting hit in the eye (blunt eye injury) or corneal abrasions, chemical burns and foreign body exposure, among others.
Lack of sleep
Not getting enough sleep can affect the eyes in several ways. It can contribute to conditions like blepharitis and dry eye, which may cause eye redness. Sleep deprivation can also decrease tear production and may cause bloodshot eyes and other signs or symptoms.
Sun damage to the eyes
Exposing your eyes to sunlight, especially without the protection of UV-blocking sunglasses, can cause a condition known as photokeratitis. Similar to the skin’s reaction to sunburn, the whites of the eyes may appear red when this condition occurs.
SEE RELATED: 5 eye conditions linked to sun damage
Eye strain caused by digital device use
Eye strain, or eye fatigue, comes from focusing the eyes on something for long periods of time. This can include watching TV or looking at a computer monitor or mobile device. Digital eye strain (also called computer vision syndrome) is a common cause of eye fatigue.
Straining the eyes, especially in the presence of glare, can make viewing a digital screen more difficult, making the eyes work harder. Eye strain can lead to bloodshot eyes and other vision and health-related problems.
Debris
Debris or a foreign object in the eye is among the common causes of bloodshot eyes. Dust, sand, dirt, eye makeup and flecks of metal are common objects that may fall or get blown into the eye, resulting in redness and other issues.
Eye irritants
Many types of environmental factors can irritate the eye and cause redness or other effects. Some of these factors include:
Smoke (fire-related and cigarette smoke)
Airborne fumes (such as perfumes and gasoline)
Chemical exposure (such as chlorine in swimming pools)
Dry air (such as in arid climates, airplane cabins and office buildings)
Other common eye irritants include preservatives (such as benzalkonium chloride) found in some eye drops. The overuse of ocular decongestant medications (such as naphazoline) may also lead to eye redness.
Lifestyle factors
Lifestyle factors can contribute to your red eye risk. For example, smoking (tobacco or marijuana) can cause red eyes, as can significant alcohol consumption. The sustained use of digital devices and insufficient sleep are other lifestyle-related causes of red eyes.
SEE RELATED: How alcohol can affect your eyes
Other health conditions
Colds or general allergies are other health conditions that can make the eyes appear red at times. For instance, COVID-19 is known to cause several types of eye problems, including the appearance of bloodshot eyes.
How to treat eye redness
Many instances of bloodshot eyes are minor and not harmful to your eye health — and may even clear up with over-the-counter (OTC) remedies.
But if you suddenly develop red eyes or have eye redness that lasts more than 24-48 hours, visit an eye doctor to determine the cause and learn about your red eye treatment options.
Treatment for red eyes may include home remedies, over-the-counter drops or professional medical care.
Home remedies
Visiting your eye doctor is the best and safest way to determine the cause of your bloodshot eyes and receive the most effective red eye treatment options. In mild cases of eye redness, and until you can see your doctor about your red eye problem, a few home remedies may provide some relief.
Apply a cool compress – Applying a cool compress to red, irritated eyes can help alleviate this concern. A compress, such as a clean washcloth, can be moistened with cold water and placed over closed eyes a few times a day.
Rest your eyes – Getting better quality sleep and giving your eyes a break from digital screen time can improve eyes that are bloodshot from fatigue or eye strain.
Change or remove your contact lenses – Changing old contact lenses to new ones or taking out your contacts and wearing your glasses until the redness improves can help manage this problem. Limiting the amount of time spent wearing contacts may reduce the risk of red eye recurrence.
Avoid allergens and irritants – Minimizing your exposure to irritants like dust, pollen, pet dander and smoke may improve your red eye problem or prevent it from worsening.
Rinse your eyes – Rinsing your eye with a proper eye wash solution or tap water can flush out dust, sand and other small debris.
Blink your eyes more often – Blinking helps keep the eyes moist by maintaining tear production. This can flush a particle from your eye or help keep your eyes from drying out when using digital devices.
Over-the-counter options
Over-the-counter red eye treatment options may reduce the appearance of bloodshot eyes. Remember to confirm the use of any nonprescription medication with your health care provider or eye specialist before taking or using OTC medicinal products.
Artificial tears – You may want to moisten your eyes frequently with preservative-free lubricating eye drops until you can see your eye doctor for red eye treatment. Lubricating drops, commonly referred to as artificial tears, may be used up to four times per day.
Decongestant (redness-relieving) eye drops – Some OTC drops, such as Visine, use decongestants like tetrahydrozoline and naphazoline to temporarily decrease swelling in the blood vessels on the eye’s surface. This can minimize the appearance of red or bloodshot eyes. Decongestant eye drops should not be used for longer than two to three days.
Low-dose brimonidine eye drops – Brimonidine tartrate 0.025% OTC eye drops (such as Lumify) can help relieve minor eye redness. These drops can be used up to four times a day. They tend to have fewer side effects and can be used for longer periods of time compared to other decongestant redness-relieving drops.
Antihistamine eye drops – OTC antihistamine drops may help relieve eye redness and itchiness caused by seasonal allergies. These eye drops also should not be used for longer than two to three days.
Be sure to see your eye doctor before using "red eye remover" eye drops, even if they are the over-the-counter variety. This is important since some of these drops may contain decongestant medications that shrink blood vessels.
Making blood vessels on the sclera smaller can help whiten your eyes. However, if you use red eye remover drops frequently over a period of time, you may need to use them more often to keep the redness from coming back. And you might experience more severe eye redness if you stop using the drops.
Seeing your eye doctor is the safest way to identify the best red eye treatment for your needs.
SEE RELATED: How to put in eye drops correctly
Medical treatments
Treatment for red eyes can vary widely and may depend on the reason behind their occurrence. Your eye doctor can determine how to treat red eyes and any other signs or symptoms you might be experiencing. Bloodshot eyes alone do not necessitate a specific type of treatment. Rather, treating the underlying cause generally improves the redness of the eye.
When you visit your eye specialist for red eyes, they will likely review your health history and perform an eye exam. Depending on the cause of eye redness or other issues you may be experiencing, eye redness treatment might include:
Saline eye rinse
OTC eye drops
Prescription eye drops, ointments or antibiotics
Steroids
Topical allergy drops
Foreign body removal
Eye surgery or other procedures may be recommended to treat and manage underlying conditions causing the eye redness.
Risk factors and complications
Because red eyes have many causes (including some that are serious and need immediate attention), it is important to see an eye specialist right away if you have red or bloodshot eyes. This is particularly important if the redness comes on suddenly and is associated with discomfort or blurred vision.
Some causes of eye redness are more concerning and could pose a threat to your eyes or cause vision loss without prompt medical care. Eye redness on one side (as opposed to in both eyes) may also indicate a more serious eye condition.
Conditions like glaucoma and eye injuries could cause vision loss, blindness and eye damage. Since red eyes can point to vision-threatening conditions, it is essential to seek professional treatment as soon as possible.
Red eyes in children

Eye redness in children should be evaluated by an eye specialist, as it can indicate the presence of various eye conditions. Taking your child to an eye specialist is recommended to determine the cause of the redness.
If your child experiences bloodshot eyes in addition to either light sensitivity, changes to their vision or eye pain, immediate care may be needed.
Preventing red eyes
While you may not be able to prevent certain conditions or factors that cause bloodshot eyes, there are steps you can take to reduce your general risk. These include:
Wash your hands frequently and always before touching your eyes.
Avoid rubbing your eyes, especially if they feel irritated or you have other eye symptoms.
Adjust your home’s humidity. A dehumidifier can reduce molds and allergens that cause red eyes, while a humidifier may help relieve redness from dry eyes.
Avoid exposure to allergens and irritants, such as pollen, pet dander, dust, fumes, smoke and chemicals.
Practice good contact lens hygiene and avoid sleeping in your contacts if possible.
Remove makeup around the eye thoroughly.
Take short breaks or reduce your time spent viewing digital screens.
Get a sufficient amount of sleep.
See your eye care professional for more tips on preventing red eyes.
When to contact an eye doctor
Bloodshot eyes may not always be a major cause for concern, but they can indicate serious eye conditions that require immediate care.
Seek immediate emergency treatment at the hospital if you have eye redness and experience one or more of the following:
Nausea and/or vomiting
Visual disturbances, such as halos around lights
Headache accompanied by confusion or blurry vision
Contact your eye doctor right away if you have red eyes and experience one or more of the following:
Eye redness that persists for more than one to two days
Eye pain or changes to your vision
Sensitivity to light
Debris in your eye (such as metal, glass or other objects)
Green or yellow discharge coming from your eye
If you suffer an eye injury, see your eye doctor as soon as possible, even if the injury does not seem severe. Go to your closest emergency room if you are not able to see an eye care professional right away.
Schedule an appointment
Red eyes are a very common eye concern, and, chances are, you may experience bloodshot eyes at some point in your life. While this is often a minor issue that lasts only a brief time, it can signal serious eye conditions and should be evaluated by an eye care specialist. If you have eye redness or other concerns about your vision or eye health, contact an eye professional to schedule an appointment.
READ NEXT: How to whiten your eyes
Redness-relieving eye drops. American Academy of Ophthalmology. EyeSmart. April 2023.
Eye redness. A.D.A.M. Medical Encyclopedia. [Internet]. August 2022.
Eye redness. Merck Manual Consumer Version. June 2021.
Red eye. Cleveland Clinic. January 2023.
Home remedies for bloodshot eyes. American Academy of Ophthalmology. EyeSmart. April 2023.
Why are my eyes red? 9 causes of red, bloodshot eyes. GoodRx Health. May 2023.
Is the sclera avascular (without blood vessels)? American Academy of Ophthalmology. EyeSmart. January 2019.
What is a subconjunctival hemorrhage? American Academy of Ophthalmology. EyeSmart. May 2023.
Cogan syndrome. American Academy of Ophthalmology. EyeWiki. October 2023.
Eye allergy. American College of Allergy, Asthma, & Immunology. Accessed October 2023.
Eye infections from contact lenses. American Academy of Ophthalmology. EyeSmart. May 2023.
Blunt eye injuries. Merck Manual Consumer Version. March 2022.
Eye corneal injuries. Penn Medicine. August 2022.
How lack of sleep affects your eyesight. American Academy of Sleep Medicine. June 2020.
What is photokeratitis — including snow blindness? American Academy of Ophthalmology. EyeSmart. May 2023.
Eyestrain. Johns Hopkins Medicine. Accessed October 2023.
Computer vision syndrome. American Optometric Association. Accessed October 2023.
Foreign bodies in the eye. Children’s Hospital of Philadelphia. Accessed October 2023.
Cornea (or other superficial ocular) foreign body. The College of Optometrists. October 2023.
The adverse effects of air pollution on the eye: A review. International Journal of Environmental Research and Public Health. January 2022.
Bloodshot eyes. A.D.A.M. Medical Encyclopedia [Internet]. August 2022.
COVID-19 can affect your eyes: How COVID causes eye pain and eye infections. GoodRx Health. September 2023.
Managing contact lens-associated red eye. Review of Cornea and Contact Lenses. December 2021.
Recognizing and treating eye injuries. American Academy of Ophthalmology. EyeSmart. April 2023.
Excessive blinking in children. American Association for Pediatric Ophthalmology and Strabismus. March 2022.
Which over-the-counter medications treat itchy eyes? GoodRx Health. April 2022.
What are eye allergies? American Academy of Ophthalmology. EyeSmart. September 2023.
Uveitis. National Eye Institute. November 2023.
Evaluation of red flags minimizes missing serious diseases in primary care. Journal of Family Medicine and Primary Care. March – April 2018.
Glaucoma. National Eye Institute. November 2023.
10 child eye problems parents should never ignore. American Academy of Ophthalmology. EyeSmart. July 2022.
How does marijuana affect vision? Canadian Association of Optometrists. March 2023.
How to cope when smoke gets in your eyes. American Academy of Ophthalmology. EyeSmart. September 2020.
Page published on Tuesday, December 11, 2018
Page updated on Tuesday, January 23, 2024
Medically reviewed on Friday, December 15, 2023






