Abducens nerve

What is abducens nerve?
The abducens nerve, also called the sixth cranial nerve or cranial nerve 6, is a motor nerve that controls the lateral rectus muscle. This is an extraocular eye muscle that allows the eye to perform abduction. Abduction is an outward movement.
For example, crossing your eyes inward to look in at your nose is using adduction — the opposite motion of abduction. So, the eyes’ ability to focus in a direction away from the nose is controlled by the lateral rectus muscle and, in turn, the abducens nerve.
Abducens nerve anatomy
The abducens nerve takes quite a journey from the brainstem to the lateral rectus muscle.

It starts out from the abducens nucleus, which is housed in the pons of the brain. The pons is the largest part of the brainstem and is sandwiched between the midbrain (above the pons) and the medulla (below the pons).
From the abducens nucleus, the abducens nerve travels out of the pons, using the point where the pons and the medulla meet as an exit. At this point, it enters the subarachnoid space, which works like a tunnel through the brain mater.
The subarachnoid space then drops the abducens nerve off at the Dorello canal. This canal channels the abducens nerve to a large vein called the cavernous sinus.
Besides the abducens nerve, several other cranial nerves run alongside the cavernous sinus. The cavernous sinus works as an organizer that transmits the cranial nerves to their respective function.
In the case of the abducens nerve, it travels through the cavernous sinus until it reaches the superior orbital fissure. From there, it enters the bony orbit (eye socket) and latches onto the lateral rectus muscle, where it performs its function.
SEE RELATED: Exotropia
Cranial nerve 6 function
The role of the abducens nerve is to control extraocular motor functions of the eye. The oculomotor nerve and trochlear nerve also help with this function.
While the oculomotor nerve also has non-vision sensory function, the trochlear nerve has purely motor function like the abducens nerve.
The abducens nerve carries nerve impulses to the lateral rectus muscle. This triggers the muscle to contract and abduct the eye on the side being signaled. The contralateral oculomotor nerve stimulates the medial rectus muscle so the eyes can move together in a synchronized manner.
Problems that can affect cranial nerve 6
Dysfunction of the abducens nerve is known as sixth nerve palsy or abducens nerve palsy. It usually occurs when a problem develops somewhere along the path that the abducens nerve takes.
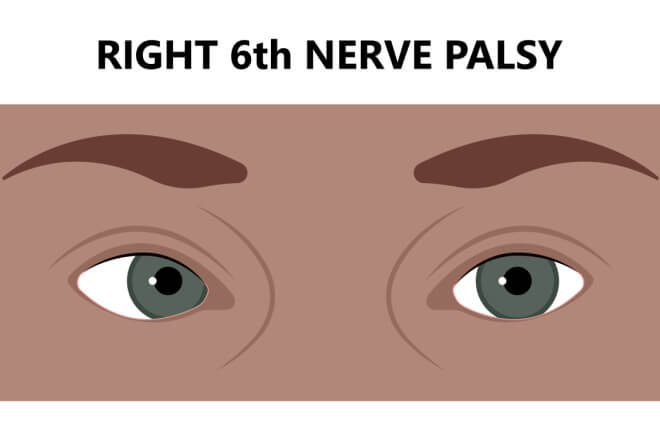
The abducens nerve begins in the brainstem and ends at the orbital socket. If trauma were to occur, or tumors were to develop anywhere along the nerve path, sixth nerve palsy could result.
However, the cause of sixth nerve palsy could lie within specific problems of the:
Brainstem
Intracranial pressure
Petrous apex
Cavernous sinus
Orbital
SEE RELATED: Ocular migraines and visual migraines explained
Brainstem
If sixth nerve palsy occurs and the problem lies in the brainstem, it’s likely because the abducens nucleus or nerve fibers have been affected. Events that can cause this include:
Stroke
Metabolic disease, such as diabetes or Wernicke-Korsakoff syndrome
Lesions that erode the protective layer around the nerves, called myelin sheath. Lesions may be caused by compression, inflammation (seen often in people with multiple sclerosis) or ischemia (low blood flow)
SEE RELATED: 7th Cranial Nerve
Intracranial pressure
The subarachnoid space — the tunnel that guides the abducens nerve through brain matter — can also be a source for abducens nerve palsy. This area can be affected by a pressure imbalance within the brain, called intracranial pressure (ICP).
When ICP becomes too high or too low, it can cause the brainstem to move, which can stretch the abducens nerve. Circumstances that may cause a change in intracranial pressure include:
Aneurysm – A blood vessel in the brain that becomes bulged
Hemorrhage – Bleeding in the brain
Infection – May be fungal (cryptococcus), viral or bacterial (Lyme disease, tuberculosis, or syphilis)
Injury – Often happens after a procedure like spinal anesthesia or lumbar puncture
Inflammatory lesions – Associated with conditions like sarcoidosis or lupus
Carcinomatous meningitis – When cancer cells spread from a primary tumor to the meninges (protective tissue that covers the brain and spinal cord)
Cell infiltration – Associated with conditions like lymphoma, leukemia and carcinoma
If ICP is imbalanced, other symptoms such as headache, nausea, vomiting and optic nerve swelling may be present.
SEE RELATED: Optic nerve
Petrous apex
This area comes into contact with Dorello’s canal, which channels the abducens nerve to the cavernous sinus. For this reason, if one or more of the following problems occur in the area, cranial nerve 6 may be affected.
Complications with a middle ear infection (otitis media), such as abscesses and inflammation
Serious bacterial infection that affects the mastoid bone behind the ear, called mastoiditis
Blood clot in the sinuses that prevent blood from draining out of the brain (sinus thrombosis)
Injury that causes a fracture at the base of the skull
If this area is the cause of abducens nerve palsy, hearing or ear issues may also be present.
SEE RELATED: Third Nerve Palsy
Cavernous sinus
Sixth nerve palsy that stems from problems in the cavernous sinus is usually caused by stretching of the abducens nerve. Some reasons this may happen include:
Blood clot in the cavernous sinus (thrombosis)
An abnormal connection develops between the cavernous sinus and the carotid artery, called a cavernous sinus fistula
An internal carotid artery experiences an aneurysm (when a blood vessel expands) or dissection (when a blood vessel tears)
Orbital
The cause of sixth cranial nerve palsy may be caused by a problem in or around the eye’s structure. If this is the case, bulging eyes may be the first sign that something is wrong. Orbital issues that may result in sixth cranial nerve palsy include:
Trauma
Infection of the soft tissues and fat in the orbital structure behind the eye (orbital cellulitis)
Inflammatory disease, such as orbital myositis, that affects the extraocular muscles
Swelling of the tissue behind the eyes, which gives the impression of a tumor, but is not actually a tumor and does not spread to other parts of the body — called an orbital pseudotumor
Though the cause of 6th nerve palsy usually lies within one of these areas, it’s possible for it to occur spontaneously. Cases like this are referred to as isolated sixth nerve palsy. This means doctors can’t pinpoint a specific cause for the symptoms.
If you notice a sudden change in vision, see an eye doctor. Medical attention should also be sought if there’s a sudden onset of muscle weakness in the eyes. This would present as having difficulty controlling eye movements, blinking, or lifting the eyelid (ptosis).
READ NEXT: Cranial nerve 5 (trigeminal nerve)
Abducens nerve. Radiopedia. June 2022.
The abducens nerve (CN VI). Teach Me Anatomy. March 2019
Abducens nucleus. Radiopedia. March 2022.
The pons. Teach Me Anatomy. December 2020.
Subarachnoid space. Kenhub. June 2022.
Dorello canal. Radiopedia. June 2022.
Cavernous sinus. Radiopedia. December 2021.
Neuroanatomy, cranial nerve 6 (abducens). StatPearls. November 2021.
The 12 cranial nerves. Simply Psychology. June 2021.
Abducens nerve palsy. StatPearls. April 2022.
The six syndromes of the sixth cranial nerve. Journal of Ophthalmic & Vision Research. April 2013.
Definition of carcinomatous meningitis. National Cancer Institute. Accessed July 2022.
Carotid-cavernous fistula (CCF). University of Michigan Radiology. Accessed July 2022.
Aneurysm and dissection. UCLA Health. Accessed July 2022.
Orbital pseudotumor. Cedar Sinai. August 2020.
Page published on Wednesday, August 24, 2022






