How the 7th cranial nerve impacts eye function and vision
What is the 7th cranial nerve?
The 7th cranial nerve is also known as the facial nerve. It controls movements such as smiling and frowning, forceful eyelid closure, normal blinking and raising the eyebrows. It also relays taste from the tongue and sensation from the outer ear and regulates tears and saliva production.
Nerves are the “wiring” that carries signals between the brain and different parts of the body. They are made of fibers that innervate—supply—your muscles, glands and organs. Nerves move the muscles and receive sensations such as sight, smell, taste, hearing and touch. They also help regulate functions such as digestion and breathing.
The facial nerve is an essential connection between the brain and many facial muscles, enabling them to perform a wide range of complex movements. Without the seventh cranial nerve, expressing emotions or savoring the taste of our favorite flavors would be impossible.
It also controls several different functions in the eyes, including:
Regulating the lacrimal gland, which produces tears in the eyes
Controlling eyelid closure
Controlling normal blinking
Moving the eyebrows
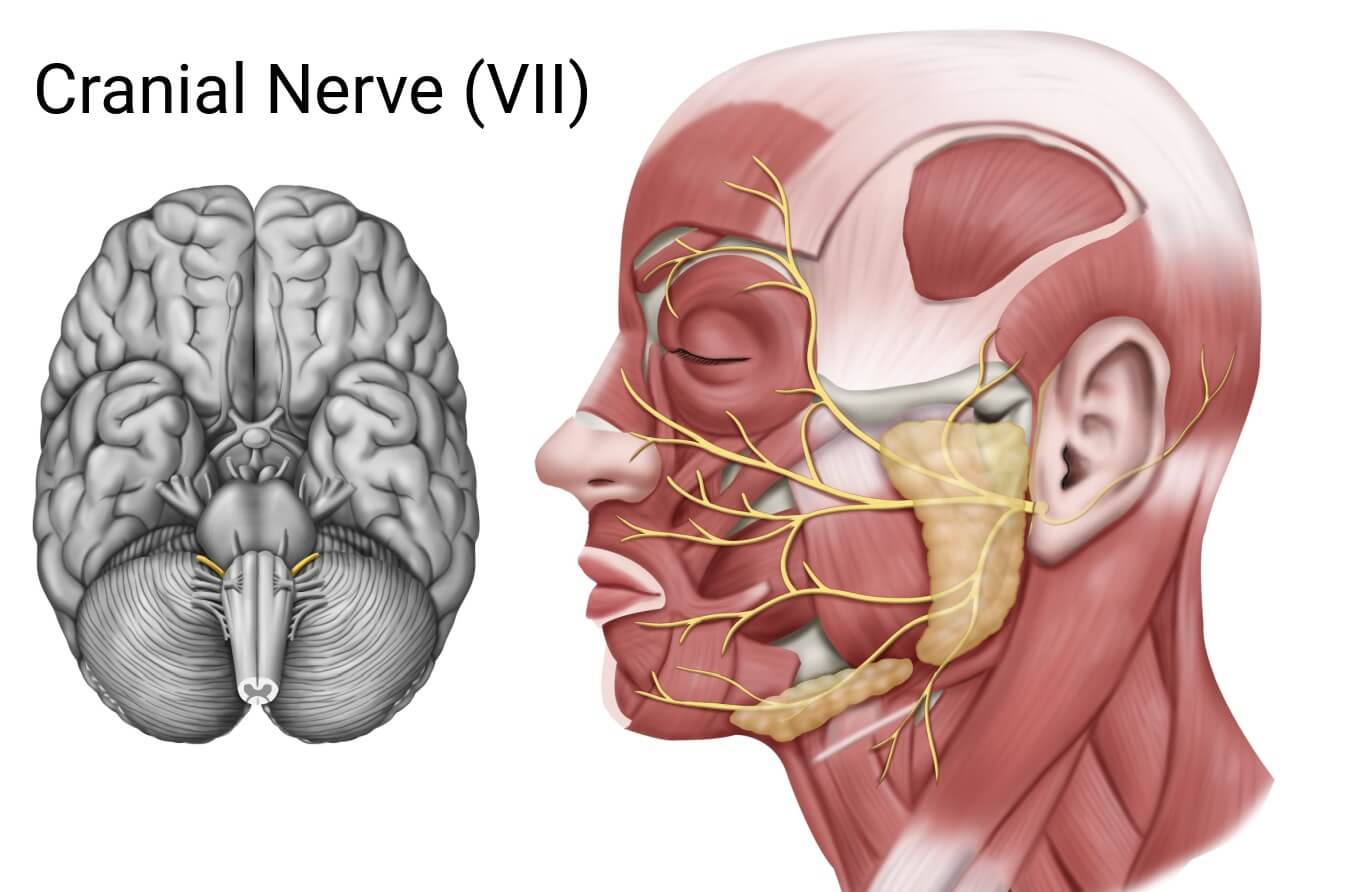
Anatomy of the 7th cranial nerve
Twelve pairs of nerves on each side of the head travel from the brain to the face, head or torso.
The facial nerve is the 7th cranial nerve and starts from the brain stem.
From there, it travels from the base of the skull to the muscles of the face through an opening in a bone by the ear.
It then spreads out by the ears into five branches across the face.
Function of the 7th cranial nerve
The overall functions of the 7th cranial nerve can be categorized into three general nerve fiber types:
Motor – These carry signals from the brain to muscles.
Sensory – These receive signals from the body and carry them back to the brain.
Parasympathetic or secretomotor – These regulate the function of a gland.
Motor functions
The facial nerve moves muscles in the face and has the following five branches:
Frontal (temporal) branch – Moving the muscles of the forehead and eyebrows
Zygomatic branch – Closing the eyes
Buccal branch – Blinking, moving the nose, smiling
Marginal mandibular branch – Frowning, middle ear noise response
Cervical branch – Moving the chin and lower corners of the mouth
Sensory functions
The facial nerve receives sensory signals, which it relays to the brain. These signals are received from the following:
Tongue – Taste from the front two-thirds of your tongue
Ear – Sensations from the outer ear and ear canal
Parasympathetic or secretomotor functions
The facial nerve regulates the function of the following glands:
Lacrimal gland – The lacrimal gland is located on the outside corner of the eyelid. It secretes the watery portion of the tear film. Tears are essential for clear vision and keeping the eyes moist and comfortable.
Salivary glands – The salivary glands empty saliva into the mouth to aid in lubrication and digestion. The facial nerve supplies the submandibular and sublingual salivary glands.
What is facial nerve palsy?
Facial nerve palsy is weakness or paralysis in an area of the face that is controlled by cranial nerve VII. It results from injury or dysfunction of that nerve. It most often occurs in individuals aged 15-45.
The difference between facial palsy and facial nerve palsy
Facial palsy refers to weakness in the facial muscles, often called a “facial droop.” Facial palsy may be due to cranial nerve VII palsy, but it could also be caused by a condition impacting the brain or brainstem, such as a stroke or multiple sclerosis.
Facial nerve palsy refers to conditions where facial weakness (or facial droop) results specifically from a problem with cranial nerve VII on the affected side of the face.
READ MORE: A guide to vision changes that can occur after a stroke
Causes of facial nerve palsy
Over half of all cases of facial nerve palsy are idiopathic (the cause is unknown). Other causes include:
Infection
Injury
Inflammation
Tumor
Medical or surgical treatment
Congenital (present at birth)
Idiopathic facial nerve palsy has typically been referred to as Bell’s Palsy. More recently, Bell’s palsy has been specifically defined as:
Having a rapid onset (<72 hours)
Having an unknown cause (idiopathic)
Occurring on one side of the face
Resolving on its own (spontaneously)
Doctors suspect that some idiopathic seventh nerve palsy cases may be caused by a virus infection or an immune disorder and now categorize these separately.
READ MORE: Bell’s Palsy: Symptoms, Risks, Diagnosis and Treatment
Symptoms of facial nerve palsy
Facial nerve palsy occurs on one side of the face. It often begins with pain behind the ears. Within hours, facial palsy symptoms begin, becoming severe within 48 to 72 hours. Additional symptoms include:
Drooping face
Weakness and numbness
Lack of facial expression
Inability to smile
Inability to blink or fully close eyes
Inability to wrinkle the forehead
Limited or no ability to grimace
Facial twitching or spasm
Involuntary movements of the face
Difficulty chewing
Trouble pronouncing certain sounds
Decreased tolerance to noise
Change in taste
Dry mouth
In severe cases, the distance between the eyelids widens, and the eye cannot be closed, drying out the front of the eye.
Diagnosis of facial nerve palsy
There is no single test that can detect facial nerve palsy. A doctor will diagnose this condition based on an evaluation, such as how well you can make facial expressions, open and close your eyes or raise your eyebrows. They may also order the following tests to determine whether the cause of facial palsy is due to facial nerve damage or inflammation or due to another underlying issue:
Chest x-ray
CT
MRI
Laboratory tests
EMG (electromyography)
READ MORE: Eye symptoms commonly seen in multiple sclerosis
How facial nerve palsy affects the eyes
Facial nerve palsy can affect the ability to close the eyes, causing the eye's front surface to become dry, irritated and uncomfortable. Facial nerve palsy can cause:
Redness
Burning
Tearing
Feeling something is in the eye
Drooping eyes
Drooping eyebrow
READ MORE: Cranial nerve palsy – CN III, IV, VI & VII palsy
Managing vision problems caused by facial nerve palsy
Facial nerve palsy can improve within several months on its own. Idiopathic facial nerve palsy improves on its own in about 70% of people within 6 weeks. However, it may require treatment and is sometimes permanent.
Management of eye issues
The cornea and conjunctiva, tissues at the front of the eye that are normally kept moist by the eyelids and tear film, may dry out if the eye can’t shut properly. To address this, an eye doctor may:
Patch the eye
Tape or suture the eye shut
Recommend artificial tears or ointments
Recommend a salt solution
Put in punctual plugs
Recommend surgery to add weights to the upper eyelids to help them close
Management of facial issues
The treatment for facial nerve palsy can vary depending on the underlying cause. Some of these treatments include:
Oral corticosteroids – These drugs are prescribed to patients 16 years and older if symptoms have been present for fewer than three days. They help decrease nerve swelling and can speed up the recovery of facial movement.
Antiviral drugs – These drugs are sometimes prescribed to fight possible infections, but their effectiveness has not been proven.
Botox injections – These injections may be given to help the upper eyelid close, treat involuntary facial movements or improve the symmetric appearance of the face.
Speech therapy – This therapy helps treat speech and swallowing issues.
Occupational therapy – This therapy works with regaining facial expressions and communication ability.
Physical therapy – This therapy improves facial muscle coordination, symmetry and strength.
Surgery – The type of surgery necessary can vary depending on the underlying cause and symptoms. Surgery to treat eyelid issues and cosmetic surgery may be necessary if the condition is permanent.
When to see an eye doctor
If you experience any of the symptoms listed above, it is important to seek urgent medical care. The underlying cause for some of these symptoms may be a medical emergency, and earlier treatment can result in a better long-term outcome.
See an eye doctor if you have been diagnosed with facial nerve palsy and are experiencing eye or vision symptoms. Routine, comprehensive eye exams are important for maintaining eye health and clear vision.
Nerves. Cleveland Clinic. March 2022.
Cranial nerve palsy. American Association for Pediatric Ophthalmology and Strabismus. April 2022.
Facial nerve palsy. EyeWiki. American Academy of Ophthalmology. January 2024.
Facial nerve anatomy and clinical applications. StatPearls [Internet]. May 2023.
Facial nerve. Cleveland Clinic. December 2021.
How the ear works. Johns Hopkins Medicine. Accessed May 2024.
Anatomy, head and neck: Eye lacrimal gland. StatPearls [Internet]. July 2023.
Salivary glands. Cleveland Clinic. July 2022.
Facial nerve disorders. University of Utah Health. Accessed May 2024.
Facial paralysis. Cleveland Clinic. December 2022.
Facial nerve palsy. Merck Manual Professional Edition. November 2023.
Page published on Friday, July 12, 2024
Page updated on Tuesday, July 16, 2024






