Oculomotor nerve
What is the oculomotor nerve?
The oculomotor nerve is one of 12 cranial nerves that supply function to muscles in the face and throat. Also called cranial nerve 3, the oculomotor nerve provides important functions like pupil constriction, eyelid positioning and eye movement.
The oculomotor nerve provides two types of motor functions for the eye: somatic motor function and visceral (autonomic) motor function.
Somatic motor function has to do with skeletal muscles, like the extraocular muscles. Visceral motor function controls soft tissue organs, like the pupils and organs used in digestion.
When illness, trauma or other disorders affect the oculomotor nerve, it can lead to its temporary or long-term paralysis. This is known as third nerve palsy. Third nerve palsy can impair the different functions that the oculomotor nerve provides.
Cranial nerve 3 anatomy
When viewing the anatomical order of the cranial nerves within the brain, the oculomotor nerve comes third. This is why it’s also referred to as “cranial nerve 3” or the “third cranial nerve.”
Because the oculomotor nerve serves both somatic and visceral motor functions, its fibers stem from two different nuclei in the midbrain. The midbrain is the topmost part of the brainstem and is where many cranial nerves begin.
Nerve fibers that control somatic nerve function begin in the oculomotor nucleus. The fibers that control visceral motor function begin in the Edinger-Westphal nucleus.
Though they are separate nuclei, the oculomotor nucleus and Edinger-Westphal nucleus are very close together and have similar routes through the brain to the eyes. And while there are two different nerve fibers that make up the oculomotor nerve, it’s still referred to as a single nerve.
The oculomotor nerve exits the front part of the brainstem, between the midbrain and the pons. From here, cranial nerve 3 moves through the subarachnoid space, traveling to the eyes at the front of the skull. The subarachnoid space is an area between layers of brain matter. It allows cranial nerves, blood vessels and cerebrospinal fluid to travel through the brain.
The oculomotor nerve exits the brain by going through its outermost protective layer (dura mater). It enters the cavernous sinus, which is a hollow space behind the nose. As the nerve moves to the front part of the cavernous sinus, it splits into two branches: the superior branch and the inferior branch.
As they exit the cavernous sinus, both branches enter the orbit (eye socket) via the superior orbital fissure, which is a large hole behind each eye. Before reaching their destination, the two branches divide further to innervate (provide function to) the different muscles in and around the eye.
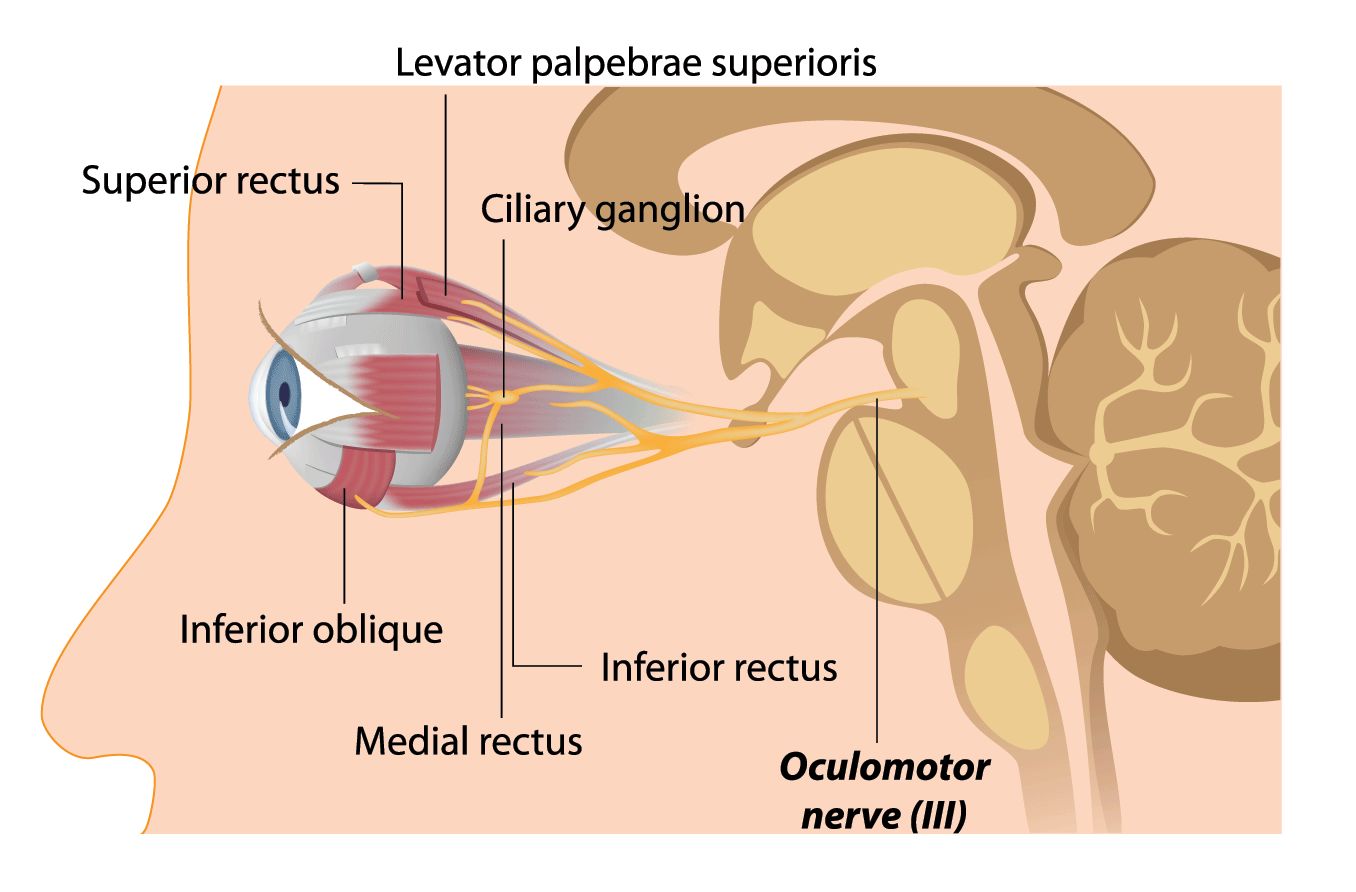
The superior branch splits to innervate the:
Superior rectus
Levator palpebrae superioris
The inferior branch divides to innervate the:
Inferior oblique
Medial rectus
Inferior rectus
Short ciliary nerves
SEE RELATED: Optic nerve
Oculomotor nerve function
The third cranial nerve gives function to four of the six eye muscles that control eyeball movement. The muscles that provide somatic motor function include the:
Superior rectus – elevates the eye when looking straight ahead, known as primary position
Inferior oblique – elevates the eye when the eye is moved inward
Medial rectus – adducts the eye from primary position (moves the eye inward)
Inferior rectus – provides downward movement of the eye from primary position
Levator palpebrae superioris – lifts the upper eyelid
When it comes to visceral motor function, the oculomotor nerve innervates the sphincter pupillae muscle near the pupil. It also allows the function of the ciliary muscles. These muscles are inside the eyeball and control the curvature of the eye’s lens. They also make it possible for the pupils to constrict.
While this may seem like a small task, lens curvature and pupil constriction are critical to vision and make the following actions possible:
Accommodation – focusing on objects as they move closer to or farther away from you
Light reflex – adjusting pupil size to allow the appropriate amount of light into the eye for the clearest vision
Near focus – making it possible to focus on and see close-up objects clearly
Problems that can affect cranial nerve 3
Cranial nerve 3 can be affected by oculomotor nerve dysfunction. This is caused by a group of disorders that result in paralysis of cranial nerve 3. When this occurs, it’s known as third nerve palsy.
Third nerve palsy
Third nerve palsy describes partial or complete paralysis of the oculomotor nerve. There are varying degrees of palsy, and different functions may be affected from person to person.
Oculomotor nerve palsy can be congenital, meaning you’re born with it, or acquired, which means it occurred later in life.
What causes oculomotor nerve palsy?
It’s possible for third nerve palsy to be idiopathic. This means doctors are unsure of the cause.
Potential causes of congenital third nerve palsy include:
Aplasia – the oculomotor nucleus is missing or did not develop normally
Hypoplasia – the oculomotor nucleus is small and/or underdeveloped
Birth trauma – the molding forces used during labor can affect the skull
Intrauterine trauma – an injury or stress to the fetus during gestation
Infection – an infection, such as meningitis, can cause third nerve palsy, though it is rare
Acquired third nerve palsy may be caused by the following:
Poor blood flow related to diabetes and high blood pressure (most common cause)
Trauma to the head or face
Abnormal pressure on the oculomotor nerve due to brain tumor, aneurysm or high intracranial pressure
Bleeding in the brain caused by trauma or aneurysm
Infections, such as Lyme disease and HIV
Autoimmune disease, such as multiple sclerosis
Symptoms of third nerve palsy
As mentioned, symptoms and their severity differ from case to case. However, some signs of third nerve palsy include:
Diplopia (double vision)
Ptosis (droopy eyelid)
Strabismus (misaligned eyes)
Enlarged pupil that does not respond to light (mydriasis)
Tilting the head to compensate for the double vision
Signs of third nerve palsy usually only affect one side of the face, though it’s possible for both sides to be affected. If it’s a partial palsy, it’s possible that only a few of these symptoms are present. For example, you may experience eye misalignment, but you’re still able to lift your eyelid properly.
SEE RELATED: 7th Cranial Nerve
Third nerve palsy treatment
If third cranial nerve weakness or paralysis is due to congenital-related causes, there is no treatment to regain function. On the other hand, acquired cases may resolve on their own, depending on what caused it.
Surgery will be required if the cause is related to a brain tumor, aneurysm or high intracranial pressure.
Otherwise, a doctor will usually wait a few months to see if the palsy improves before recommending eye surgery. In the meantime, they may suggest wearing an eye patch or prism glasses to help with the double vision.
If there is no improvement after a few months, your doctor may recommend strabismus surgery. The procedure will help realign the eyes and can improve the appearance of the eyes and the double vision experienced.
Ptosis surgery is also available to help lift the droopy eyelid, which can help improve visibility in the affected eye.
When to see a doctor
See an eye doctor if you notice sudden changes in your vision, especially if the changes occur after a head or face injury. Changes in the eyes’ appearance, including their alignment and ability to work together, should also be looked at by a doctor.
READ MORE: Trochlear nerve
Neuroanatomy, cranial nerve 3 (oculomotor). Stat Pearls. March 2022.
Oculomotor nerve. Kenhub. July 2022.
What is the difference between somatic and visceral reflex? Pediaa. December 2018.
Summary of the cranial nerves. Teach Me Anatomy. September 2022.
2-minute neuroscience: Oculomotor nerve (cranial nerve III). Neuroscientifically Challenged. October 2019.
Subarachnoid space. Kenhub. July 2022.
Pupillometry: Psychology, physiology and function. Journal of Cognition. February 2018.
Oculomotor nerve. Cleveland Clinic. August 2021.
Third nerve palsy. American Academy for Pediatric Ophthalmology and Strabismus. March 2020.
Cranial nerve III palsy. StatPearls. July 2022.
Page published on Wednesday, October 12, 2022
Medically reviewed on Thursday, September 29, 2022






