Trochlear nerve
What is the trochlear nerve?
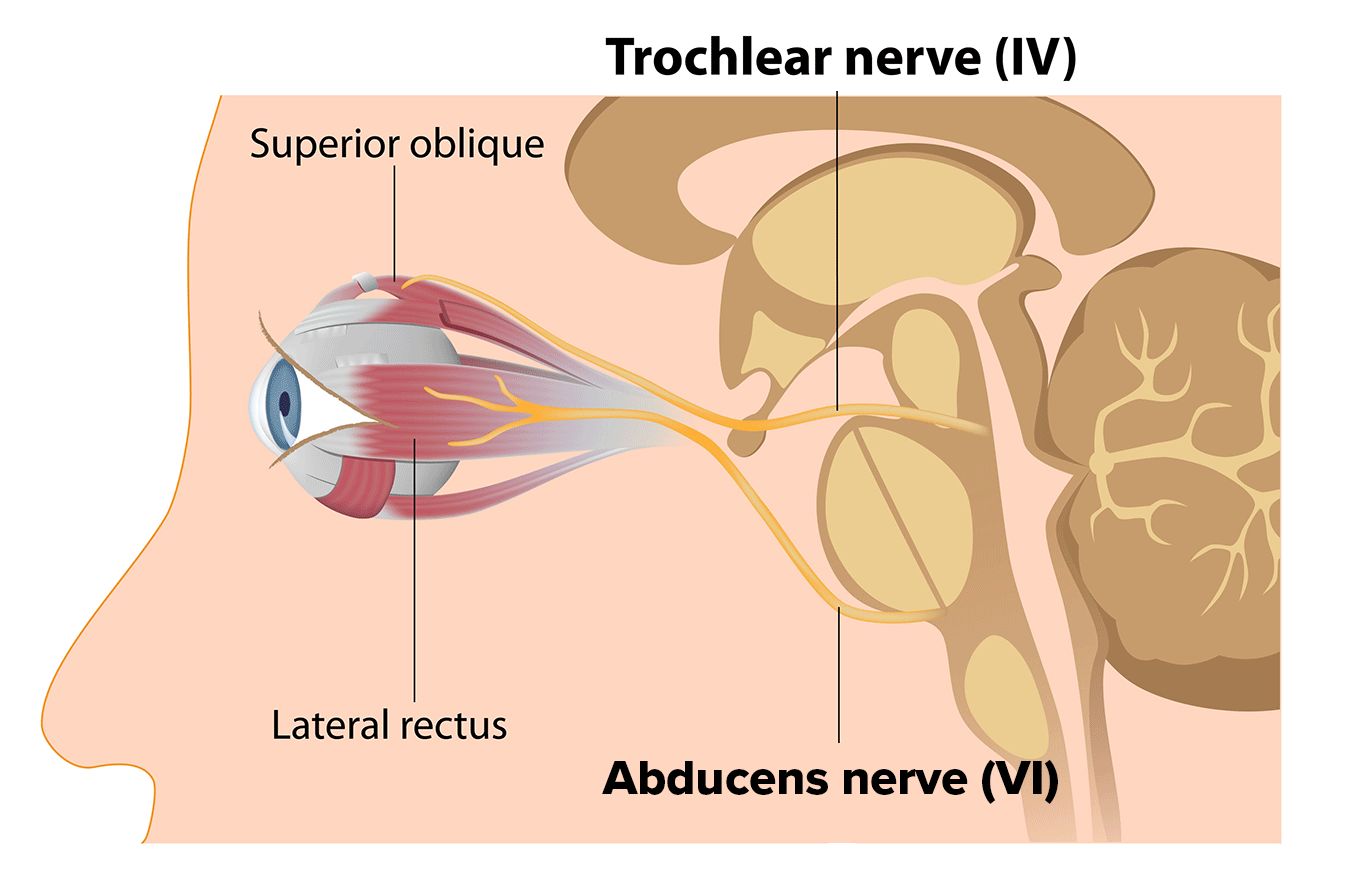
The trochlear nerve is the fourth out of 12 cranial nerves that wire the human brain. Also known as cranial nerve 4 (CN IV), the trochlear nerve controls the superior oblique muscle of the eye. This extraocular muscle allows the eyes to look downward, toward the nose, or away from the nose.
Because the trochlear nerve provides eye movements, it’s considered a motor nerve. It has the longest route of any cranial nerve but is very thin. This makes it fragile. Injury or illness can affect the nerve and cause it to work improperly — a condition called trochlear nerve palsy.
Cranial nerve 4 anatomy
The trochlear nerve is the smallest cranial nerve. This is due to its number of axons (cables within the nerve that relay signals). It also has a longer journey through the brain than any other cranial nerve. There are two trochlear nerves: one for each eye.
They begin in the trochlear nuclei, which are in the the topmost part of the brainstem (midbrain). Before exiting the brainstem, the nerves cross over one another. So, each nerve controls the eye on the opposite side of where they originate. This trait sets the trochlear nerve apart from other cranial nerves.
After crossing, the nerves exit the brainstem from the back (posterior side). This is another characteristic that only applies to the trochlear nerves. From the brainstem, the nerves move up toward the eye via the subarachnoid space. The subarachnoid space is an area between layers of brain matter. This area allows various nerves and cerebrospinal fluid to flow throughout the brain.
Once they get to the front part of the brain, the trochlear nerves poke through the dura mater (outermost layer of the brain) and enter the cavernous sinus.
The cavernous sinus works as a channel for cranial nerves that are traveling from the brain to the eyes. These nerves include the trochlear nerve, as well as the abducens nerve (CN VI) and the oculomotor nerve (CN III). Two branches of the trigeminal nerve (CN V) also run through here: the ophthalmic and maxillary branch.
From the cavernous sinus, the trochlear nerves enter their designated orbit through an opening called the superior orbital fissure. From here, each trochlear nerve attaches to the superior oblique muscle and supplies it with motor function.
SEE RELATED: Optic Nerve: Anatomy, Function and Conditions
Trochlear nerve function
The trochlear nerve is named after a small structure called the trochlea. The trochlea, which comes from the Latin word for “pulley,” makes a big impact on the eyes’ function.
After the superior oblique emerges from the sphenoid bone, it loops through the trochlea, which works as a pulley for the muscle. The trochlea and the superior oblique muscle work together to move the eyes downward, toward the nose and away from the nose. They also create a motion called intorsion, which rolls the eye upward and inward.
The superior oblique muscle and the trochlea perform these actions. But the trochlear nerve sends the motor signals that tell the muscle when and how to move.
SEE RELATED: 7th Cranial Nerve
Problems with the trochlear nerve
The trochlear nerve’s slender size and long journey through the brain make it susceptible to damage. This damage may be caused by injury or illness and can paralyze the nerve that controls muscle movement. When this occurs, it’s known as trochlear nerve palsy or fourth nerve palsy.
SEE RELATED: Third Nerve Palsy
What causes trochlear nerve palsy
Damage to the trochlear nerve may be congenital or acquired. In congenital cases, abnormalities with the trochlear nucleus, or with the nerve itself, are present from birth.
The trochlear nucleus may also be damaged in acquired palsy cases. This typically occurs due to a brainstem stroke. However, cases of acquired trochlear nerve palsy is usually caused by:
Trauma – The most common cause of acquired cases. It often occurs from the same type of trauma that causes whiplash or concussion.
Aneurysm – An artery begins to bulge and can press on the nerve or decrease its blood supply.
Vascular disease – A decrease in blood supply to the nerve can cause fourth nerve palsy. It is commonly seen as a result of diabetes. A stroke can do this as well.
Intracranial pressure – The pressure within the skull (intracranial pressure) can press on the nerve and cause fourth cranial nerve palsy.
Tumor – A brain tumor can press against the trochlear nerve, which may damage the nerve or cut off its blood supply.
Illness – A disease such as Guillain-Barre syndrome, Lyme disease, cavernous sinus syndrome and Herpes zoster can result in fourth nerve palsy.
Trochlear nerve palsy may or may not be isolated (e.g., if a tumor involved the cavernous sinus, other cranial nerves could be affected). An isolated case means nerve paralysis is the only problem experienced. Non-isolated cases mean an underlying cause is responsible.
For acquired cases, examples of underlying causes may include diabetes or stroke. For congenital cases, underlying causes may include malformations, like a misshapen skull, and other health issues. While fourth nerve palsy usually only affects one eye, it’s possible to occur in both.
There are instances in which trochlear nerve palsy occurs for an unknown reason. This is called an idiopathic case. Research suggests around 4% of trochlear nerve palsies are idiopathic.
SEE RELATED: Bell’s Palsy
Signs of fourth nerve palsy
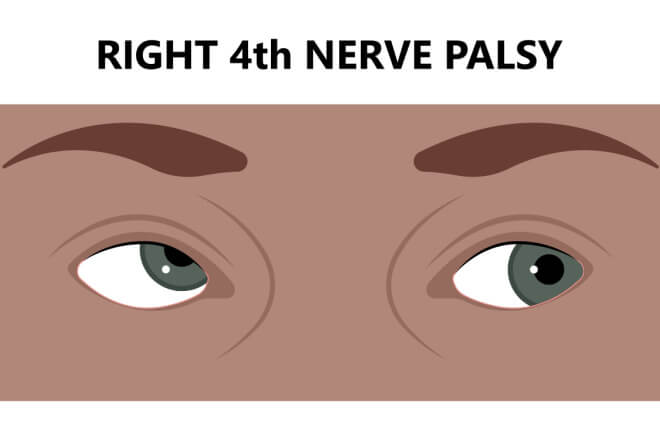
Double vision (diplopia) is a common sign of trochlear nerve palsy. It often appears as vertical or torsional diplopia. This means the “ghost” image is above or diagonal to the actual object.
Diplopia related to trochlear palsy is usually binocular, which means it only occurs when both eyes are open. Closing the affected eye often corrects the double vision.
Other symptoms of fourth nerve palsy include:
Blurred vision
Hypertropia (the eye drifts upward)
Excyclotorsion (the eye drifts upward and outward)
Head tilting to compensate for the strabismus and/or double vision
Pain above the eyebrow, which is most common in idiopathic cases or cases related to diabetes
Fourth nerve palsy treatment
Treatment for trochlear nerve palsy depends on its cause. It also depends on whether the palsy is congenital or acquired.
Congenital palsy can worsen over time and should be monitored with frequent eye exams. The eye doctor will track things like amblyopia (lazy eye), depth perception (3D vision) and the child’s head tilt, if present.
Children with congenital palsy may not need treatment. However, if vision begins to decline or their head tilt becomes more dramatic, strabismus surgery may be required.
Acquired palsy usually requires treatment for the underlying cause. This may include surgery to remove a tumor or to restore normal pressure within the skull.
Palsy caused by injury often improves over time but may never go away completely.
Idiopathic trochlear palsy tends to improve and eventually resolve on its own.
To help with the healing process, one or more of the following treatments may be recommended:
Prism glasses that are designed to help correct double vision
Over-the-counter pain medicine for headaches
Eye patch to alternate between eyes, which prevents weakening of the affected eye
Strabismus surgery to help realign the eyes, fix double vision and resolve the head tilt
When to see a doctor
Consult with your doctor if you notice any sudden changes in your vision, especially after a head injury or facial trauma. Changes in the appearance of the eyes, including their alignment and ability to move together, should also be discussed with an eye doctor.
The sooner an eye doctor is able to diagnose a vision problem, the more quickly a treatment can be administered, and clear vision can be restored.
READ MORE: Can Ramsay Hunt Syndrome Cause Eye Damage?
Neuroanatomy, cranial nerve 4 (trochlear). StatPearls. November 2021.
Trochlear nerve. Cleveland Clinic. August 2021.
Trochlear nerve. Teach Me Anatomy. March 2019.
Axons: the cable transmission of neurons. University of Queensland Brain Institute. Accessed October 2022.
The midbrain. University of Queensland Brain Institute. Accessed October 2022.
Anatomy dissected: cranial nerve IV (trochlear nerve). 3D4Medical From Elsevier. December 2019.
Trochlear nerve. Physiopedia. Accessed October 2022.
Subarachnoid space. Kenhub. July 2022.
Neuroanatomy, cavernous sinus. Stat Pearls. July 2021.
Fourth nerve palsy. Cedar Sinai. Accessed October 2022.
Fourth nerve (superior oblique) palsy. American Association for Pediatric Ophthalmology and Strabismus. March 2022.
Cranial nerve 4 palsy. EyeWiki. American Academy of Ophthalmology. September 2022.
Page published on Wednesday, October 12, 2022
Medically reviewed on Thursday, September 29, 2022






