What is keratoplasty surgery?
Keratoplasty is a general term to describe surgery involving the cornea. When someone uses the word “keratoplasty,” they’re usually talking about a corneal transplant. Keratoplasties can improve eyesight and treat vision damage from corneal scars and distortions from abnormal cornea shape.
If a cornea infection could not be resolved with antibiotics, a keratoplasty can help heal the infection and relieve pain.
Corneal makeup
There are five layers of the cornea: The epithelium, stroma and endothelium are the three main layers.
Between the epithelium and the stroma is Bowman’s layer — a fine sheet of connective tissue. Separating the stroma and the endothelium is a thin layer called Descemet’s membrane. These last two layers work like cheese between hamburger patties to keep everything together.
Types of keratoplasty surgery
Different methods, or types, of keratoplasty are used to treat various vision problems. The type of keratoplasty is determined by which layers of the cornea are replaced.
Penetrating keratoplasty
Penetrating keratoplasty is a full-thickness transplant procedure. This means that all layers of the cornea must be removed and replaced.
The procedure includes using a trephine blade to remove a circle area of the damaged tissue. A trephine is a medical device that works like a cookie cutter to make perfectly circular incisions.
Once the incision is made, the bad tissue is removed and replaced with a healthy donor cornea. The new cornea is stitched into place.
People who have a corneal disease that can lead to blindness, such as unresolved keratitis, typically need a penetrating keratoplasty.
Lamellar keratoplasty
Lamellar keratoplasty is a procedure where the epithelium and stroma are replaced. Descemet’s membrane and the endothelium are still healthy, so they're left behind. Because they aren’t needed, those layers need to be removed from the donor cornea before the transplant.
Once the donor tissue is fit to the existing cornea, it is secured in place with sutures.
People with some form of corneal thinning often need a lamellar keratoplasty. Conditions that cause corneal thinning include keratoconus and keratoglobus.
SEE RELATED: How Much Does Keratoconus Treatment Cost?
Endothelial keratoplasty
An endothelial keratoplasty involves removing the back layers of the cornea, including Descemet’s membrane and the endothelium.
In this procedure, surgeons must remove the back layers of the cornea while keeping the healthy front layers intact. To achieve this, they make a small incision that allows them to reach and remove unhealthy corneal tissue.
After that, surgeons make a small air bubble in the cornea. This allows them to insert and position the new donor tissue against the existing corneal layers.
The air bubble is left in place to ensure the donor tissue attaches to the rest of the cornea. The incision may be closed using a couple of stitches, or it may heal up on its own. The air bubble will naturally dissolve after a few days.
People with Fuchs’ dystrophy or similar conditions are most likely to have an endothelial keratoplasty.
READ NEXT: What is Peters anomaly (PA)?
Corneal transplantation and donation
According to the Eye Bank Association of America, the U.S. provided over 66,000 corneas for transplant in 2020. The donated corneas are used to restore sight for those in need, and help to further medical education and surgical advancement.
The great thing about cornea donation is that anyone can be a donor. Unlike with other organs, blood type does not have to match for a cornea transplant. There are some medical conditions that would cause a cornea to be unfit for donation. However, 97% of cornea transplants performed are successful.
Registering to become a cornea donor is free. All you have to do is sign up online to be a donor in your state.
SEE RELATED: Can You Get An Eye Transplant?
How a cornea transplant is performed
Cornea transplants are usually performed under general anesthesia, so you’ll be asleep during the procedure. Your doctor will also apply numbing medication to the eye, so you won’t feel any pain when you wake up.
Once you get anesthesia, the next steps depend on which type of keratoplasty you’re having. The steps of each procedure are detailed in the “Types of keratoplasty surgery” section above.
The donor tissue used in a cornea transplant can be preserved for up to 14 days after being recovered from the donor, but most cornea transplants happen within a week of recovery.
Surgery takes less than two hours to complete. Once the procedure is over and no complications arise, you should be able to go home.
Postoperative care after keratoplasty surgery
After surgery, your eye will be covered with an eye patch that you must wear when sleeping and showering. Twenty-four to 48 hours after surgery, the doctor will remove the eye patch to assess how the eye is healing.
You may experience irritation, redness and light sensitivity in the affected eye. This is normal. Your eye doctor will likely prescribe over-the-counter medication to help you manage pain.
Postoperative care also typically includes prescription antibiotics and corticosteroids. Using these will reduce the risk of infection and inflammation (swelling). The prescriptions will come in the form of eye drops and/or ointment to be applied as directed by your doctor.
Recovery times vary depending on the type of keratoplasty you had and other factors. The cornea has no blood supply, which means the healing process is fairly slow, but rejection of the donor tissue is less common. Stitches applied in surgery may be left for three to 12 months. If your vision is clear with the stitches in place, they can be left in permanently.
Because the stitches are buried, they don’t usually cause pain or discomfort. However, it is possible for them to break. This can cause a foreign body sensation, which will require the stitches’ removal. They may also be adjusted to improve vision.
Patients who had an endothelial keratoplasty often have a fairly quick recovery time. This is because the incision is very small and usually does not require stitches. However, you will need to lay on your back for a few days following surgery to ensure the transplant tissue sticks to the other layers of your cornea.
Long-term use of steroid eye drops can reduce the risk of graft rejection over a patient’s lifetime.
SEE RELATED: Is Blurred Vision After Eye Surgery Common?
Contact lenses after keratoplasty
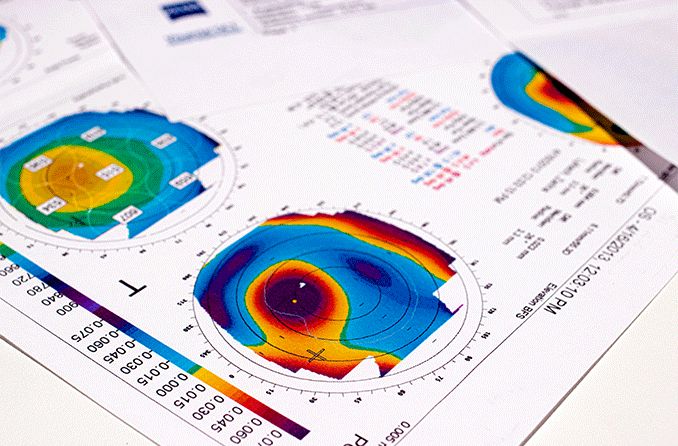
It’s common to have some level of nearsightedness or astigmatism after a cornea transplant. This is because the shape and curvature of the donor tissue will not perfectly match that of your natural cornea.
Once your postoperative vision has stabilized, your eye doctor will assess the astigmatism. It’s very likely that you’ll need to wear glasses or contacts, or need more surgery to correct your vision.
People who have had a penetrating or lamellar keratoplasty often need specialized contact lenses, such as:
Rigid gas permeable (RGP) lenses, which are made with a durable plastic and cover about 75% of the cornea
Scleral lenses, which are large enough to dome over the misshapen cornea and provide clear vision
Both lenses are helpful for people with corneal irregularities, but it’s best to discuss options with your eye doctor. There may be other contact lenses that better suit your particular vision needs.
READ MORE: Guide to LASIK Eye and Vision Surgery
Chapter 12 - Examples of successful biomaterial-based artificial tissues—artificial corneas. Stem Cells and Biomaterials for Regenerative Medicine. 2019.
Cornea transplant. National Health Service. July 2021.
Penetrating keratoplasty. Cornea Research Foundation of America. Accessed November 2021.
Penetrating Keratoplasty. Encyclopedia of the Eye. 2010.
Deep anterior lamellar keratoplasty (DALK). University of Iowa Ophthalmology and Visual Sciences. March 2016.
Lamellar keratoplasty for advanced keratoconus. Asia-Pacific Journal of Ophthalmology. December 2020.
Endothelial keratoplasty (DSEK & DMEK). Cornea Research Foundation of America. Accessed November 2021.
Chapter 86 - Conductive keratoplasty. Corneal Surgery (Fourth Edition). 2009.
Conductive Keratoplasty (CK). University of Michigan Kellogg Eye Center. Accessed November 2021.
Conductive keratoplasty. Current Opinion in Ophthalmology. July 2007.
FAQs. Eye Bank Association of America. Accessed November 2021.
Cornea transplant. Cleveland Clinic. February 2018.
About corneal transplant surgery. National Keratoconus Foundation. Accessed November 2021
Page published on Wednesday, December 8, 2021
Medically reviewed on Friday, November 19, 2021




